ABSTRACT
Introduction and objectives: Chronic total coronary occlusion (CTO) is often a complex entity to deal with through a percutaneous coronary intervention, and the clinical benefits of successful recanalization still remain uncertain. Most registries feature data in limited time periods and do not reflect the impact that specific dedicated programs have on recanalization. Our study evaluates the results of a CTO program on a long-term period of time.
Methods: All patients’ CTOs treated with percutaneous coronary interventions at our center from 2002 through 2017 were prospectively included in the registry. The clinical, angiographic and procedural data were collected, and clinical follow-up was conducted. Three consecutive periods of time were considered for the analysis of temporal trends.
Results: Atotal of 424 CTOs (408 patients) were included. In 339 patients (80%) the procedure was successful. The rate of success increased over time, from 57% in 2002-2006 to 87% in 2012-2017 (P = .001). The most important independent predictor of procedural failure was lesion tortuosity. After a median follow-up of 39.7 months, the rates of major adverse cardiovascular events and cardiovascular mortality in success vs failed groups were 13.9% vs 24.7% (P = .015) and 3.6% vs 14.1% (P = .001), respectively. These were the independent predictors of cardiovascular mortality: chronic kidney disease, left anterior descending artery occlusion, and procedural failure.
Conclusions: Our series shows a high rate of success in CTO recanalization, which has increased over the last few years due to greater expertise and improved program-specific technical advances. Several angiographic and procedural variables have been identified as predictors of failure. Successful procedures, especially on the left anterior descendent coronary artery, were associated with lower rates of cardiovascular mortality.
Keywords: Chronic total coronary occlusion. Percutaneous coronary intervention. Ischemic heart disease.
RESUMEN
Introducción y objetivos: La oclusión total coronaria crónica (OTC) es generalmente compleja de abordar con intervencionismo percutáneo y el beneficio clínico de su recanalización sigue siendo incierto. La mayoría de los registros aportan datos limitados en el tiempo y no reflejan el impacto de un programa específico para su tratamiento. Nuestro estudio evalúa los resultados de un programa de OTC a largo plazo.
Métodos: Se incluyeron de forma prospectiva todos los pacientes tratados con un intento de revascularización percutánea de una OTC entre los años 2002 y 2017. Se obtuvieron datos clínicos, angiográficos, intraprocedimiento y del seguimiento. Se consideraron 3 periodos temporales consecutivos para el análisis.
Resultados: Se incluyeron 408 pacientes (424 OTC). La desobstrucción fue exitosa en 339 lesiones (80%). El éxito se incrementó con el tiempo, de un 57% en 2002-2006 a un 87% en 2012-2017 (p = 0,001). El predictor independiente más potente de procedimiento fallido fue la tortuosidad intralesional. Tras una mediana de seguimiento de 39,7 meses, las tasas de eventos adversos cardiacos mayores y de muerte cardiaca en los grupos de éxito y fracaso fueron del 13,9 frente al 24,7% (p = 0,015) y del 3,6 frente al 14,1% (p = 0,001), respectivamente. Los predictores independientes de mortalidad cardiaca fueron la insuficiencia renal crónica, la oclusión de la arteria descendente anterior y el fallo del procedimiento.
Conclusiones: Nuestra serie muestra unas tasas elevadas de éxito en la recanalización de una OTC, incrementada en los últimos años debido a la experiencia y al desarrollo técnico del programa. Se han identificado numerosas variables clínicas y angiográficas como predictoras de fallo del procedimiento. El éxito en el procedimiento, en especial en la arteria descendente anterior, se asoció con una menor mortalidad cardiaca.
Palabras clave: Oclusión total crónica. Intervención coronaria percutánea. Cardiopatía isquémica.
Abbreviations ACS: acute coronary syndrome. CABG: coronary artery bypass graft. CTO: chronic total coronary occlusion. LAD: left anterior descending coronary artery. MACE: major adverse cardiovascular events. PCI: percutaneous coronary intervention.
INTRODUCTION
Percutaneous coronary interventions (PCI) of chronic total coronary occlusions (CTO) represent up to 12% of all PCIs performed.1 The reason to perform the percutaneous recanalization of a CTO is to improve clinical symptoms which, ultimately, has potential survival benefits as suggested by some observational studies.2-4 However, the clinical benefits of successful recanalization remain undefined and to this day accepting that opening CTOs saves lives, despite the favorable consistent results from several contemporary registries, is still not supported by randomized clinical trials.5
Given the complexity of these procedures, a specific program with dedicated CTO-trained operators is encouraged. Also, most of the published registries and randomized clinical trials are performed in highly skilled centers and feature results in limited periods of time usually on specific devices, but not long-term results.2-5
We present the results of a specific PCI program for CTO lesions, starting with the introduction of drug-eluting stents from 2002 through 2017. The profile of patients and lesions, procedural data, results, and long-term clinical outcomes have been analyzed during the time frame of the program.
METHODS
This prospective registry conducted in a single center with an active PCI program for CTOs started back in 2002. It included 1 single operator who would progressively develop proper skills.
All consecutive patients treated of their CTOs, at least once, through percutaneous recanalization during the period 2002–2017 were included. Clinical data, angiographic characteristics, and procedural features were collected. The patients gave their informed consent and the study was approved by the local review board.
The indication for the recanalization of the CTO was the presence of angina, confirmation of ischemia through provocation tests or viable myocardium assessed through magnetic resonance imaging since 2004 when this diagnostic imaging modality became available at our center. No angiographic exclusion criteria were applied. Therefore, long occlusions, severely calcified lesions, and ostial locations were included if clinically indicated. Patients with an indication for coronary artery bypass graft (CABG) were excluded.
CTOs diagnosed in the setting of an ST-segment elevation acute coronary syndrome were scheduled for intervention that was performed at least 4 weeks after the index procedure. In cases of non-ST-segment elevation, CTOs were approached during the initial catheterization or in a subsequent staged procedure at the operator’s discretion. Also, in 28 out of the 101 cases of CTOs diagnosed in the context of an ACS, the ad-hoc desobstruction of the CTO was attempted.
Most CTOs were performed by the lead operator who focused their experience on trying to improve the rate of success for the benefit of the patient.
For the analysis of temporal trends regarding techniques and results, patients were classified into 3 consecutive periods of time: 2002-2006, 2007-2011, and 2012-2017. Also, the entire cohort was divided into 2 groups regarding success or failure in the recanalization of the CTO. Follow-up data were obtained from hospital records and the contact kept with the patients and the information provided were prospectively included in a database. No routine angiographic follow-up assessment was conducted.
Procedures were performed according to standard practices through the femoral or radial approach. Antithrombotic therapy consisted of unfractionated heparin (100 U/Kg) with additional administration when appropriate, to achieve activated clotting times of 250 seconds or 300 seconds using the antegrade and retrograde approaches, respectively. Aspirin 100 mg was administered orally prior to the PCI. Before stent implantation patients received perioperatively 300 mg to 600 mg of clopidogrel followed by a daily administration of 75 mg for the prescribed period of dual antiplatelet therapy.
CTOs were defined as coronary obstructions with TIMI flow grade 0 of at least 3 months duration.
Procedural success was defined as achieving residual post-PCI stenosis < 30% associated with TIMI flow 2–3.
Mortality was considered cardiovascular unless an evident non-cardiac cause was identified. Myocardial infarction was defined according to the Third Universal Definition established by the European Society of Cardiology and the American College of Cardio- logy Foundation. Target lesion revascularization was defined as a repeated PCI on the target lesion or CABG on the target vessel following ischemia-driven restenosis. Target vessel revascularization was defined as repeated PCI or CABG on any segments of the target vessel. Major adverse cardiovascular events (MACE) were defined as cardiovascular death, myocardial infarction or need for surgical or percutaneous target vessel revascularization. Stent thrombosis was defined according to the Academic Research Consortium criteria.
The angiographic characteristics expected to be predictive of procedural success were classified according to the recommendations proposed by the Euro-CTO club consensus document.6 The J-score was calculated for each lesion based on the length of the occlusion, morphology of the stump, calcification, tortuosity, and prior attempt to open the CTO.7
Continuous variables were expressed as mean ± standard deviation or median (interquartile range [IQR]), when appropriate. Categorical variables were expressed as percentages. The chi square test or Fisher’s exact test were used to compare the categorical variables. The Kolmogorov-Smirnov test was used to verify the normal distribution of continuous data. Continuous variables were compared according to their distributions using the Student t test or Mann-Whitney U test (success vs failed subgroups), and the ANOVA or Kruskal-Wallis test (comparison of 3 time periods). The estimates of cardiovascular death-and-MACE-free survival were shown by the Kaplan-Meier curves. Inter-groupt differences were assessed using the log-rank test. The logistic regression and Cox proportional hazard models were used to assess the independent contribution of variables to procedural success and mortality, respectively. Multivariate models included variables with P values < .2 in the univariate analysis. All statistical analyses were 2-tailed, and P values < .05 were considered statistically significant. The statistical analysis was performed using the statistical software package SPSS 15.0 (SPSS Inc., United States).
RESULTS
A total of 424 CTOs (408 patients) were included. In 339 patients (80%) procedural success was achieved. The number of procedures and the corresponding rate of success per period is shown on figure 1 .
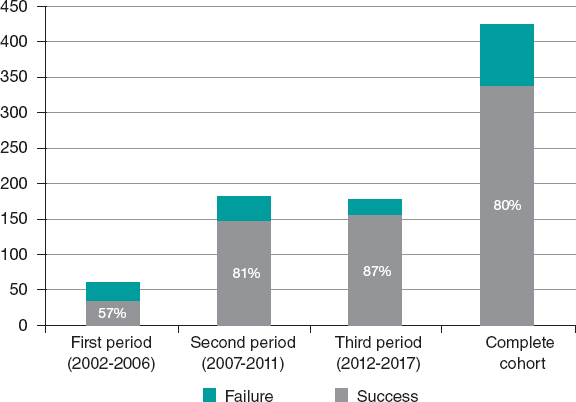
Figure 1. Number of procedures and corresponding rate of success per period.
The baseline characteristics regarding the success or failure of the CTO procedure are featured on table 1 and table 2. Previous CABG and the ACS setting were more common among failed cases. Patients with successful procedures were more prone to left anterior descending coronary artery (LAD) involvement, microchannels, and Rentrop grade 3 collateral blood flow. Procedural success was higher in the LAD compared to other target vessels (87% vs 77%; P = .02). Procedural success in the circumflex artery was the lowest of all (76%). The complexity of the CTO according to the J-score was higher in failed cases.
Table 1. Baseline characteristics
| All (n = 424) | Success (n = 339) | Failure (n = 85) | P | |
|---|---|---|---|---|
| Age | 63 ± 12 | 63 ± 12 | 64 ± 13 | .48 |
| Male sex | 350 (83%) | 277 (82%) | 73 (86%) | .37 |
| Hypertension | 279 (66%) | 217 (64%) | 62 (73%) | .15 |
| Diabetes Mellitus | 120 (28%) | 95 (28%) | 25 (29%) | .91 |
| Dyslipidemia | 275 (65%) | 222 (65%) | 53 (62%) | .45 |
| Past/current smoker | 292 (69%) | 236 (70%) | 56 (66%) | .48 |
| Previous infarction | 147 (35%) | 111 (33%) | 36 (42%) | .72 |
| Previous CABG | 31 (7%) | 18 (5%) | 13 (15%) | .002 |
| Multivessel disease | 297 (70%) | 234 (69%) | 63 (74%) | .38 |
| Left ventricular ejection fraction | 55 ± 13 | 55 ± 13 | 57 ± 13 | .17 |
| Serum creatinine (mg/dL) | 1.03 ± 0.53 | 1.02 ± 0.49 | 1.04 ± 0.64 | .76 |
| Acute coronary syndrome | 103 (24%) | 74 (22%) | 29 (34%) | .021 |
CABG, coronary artery bypass graft. | ||||
Table 2. Angiographic characteristics of occlusive lesions
| All (n = 424) | Success (n = 339) | Failure (n = 85) | P | |
|---|---|---|---|---|
| Left anterior descending coronary artery | 129 (30%) | 112 (33%) | 17 (20%) | .02 |
| Right coronary artery | 211 (50%) | 163 (48%) | 48 (56%) | .17 |
| Left circumflex artery | 81 (19%) | 62 (18%) | 19 (22%) | .39 |
| Diameter (mm) | 3.15 ± 0.45 | 3.15 ± 0.46 | 3.16 ± 0.58 | .97 |
| Length (mm) | 23 ± 16 | 21 ± 13 | 29 ± 21 | .001 |
| Moderate-to-severe calcification | 303 (74%) | 232 (72%) | 71 (84%) | .028 |
| Moderate-to-severe tortuosity | 150 (35%) | 95 (28%) | 55 (65%) | .001 |
| Severe distal disease | 122 (29%) | 91 (27%) | 31 (36%) | .14 |
| Tandem occlusions | 53 (13%) | 31 (9%) | 22 (26%) | .001 |
| Microchannels | 86 (20%) | 75 (22%) | 11 (13%) | .04 |
| Ostial/side branch location | 163 (38%) | 120 (35%) | 43 (51%) | .033 |
| Tapered stump | 208 (49%) | 171 (50%) | 37 (44%) | .12 |
| Rentrop grade 3 collateral flow | 206 (48%) | 171 (50%) | 35 (41%) | .09 |
| J score > 3 | 192 (45%) | 129 (38%) | 63 (74%) | .001 |
Data are expressed as no. (%) or mean ± standard deviation. | ||||
Procedural details are shown on table 3. The use of 8-Fr catheters and dual injections was significantly higher among successful cases with a strong trend towards retrograde approach and intravascular ultrasound guidance. Drug-eluting stents were deployed in most of cases and limus-eluting stents were the most widely used by far (79%). PCIs were performed on at least 1 additional vessel in about two-thirds of the patients from the 2 groups. Independent predictors of failure were previous CABG, moderate-to-severe lesion tortuosity, tandem occlusions, lack of dual injection, and CTOs diagnosed in the ACS setting (table 4).
Table 3. Procedural characteristics
| All (n = 424) | Success (n = 339) | Failure (n = 85) | P | |
|---|---|---|---|---|
| Femoral access | 265 (63%) | 215 (63%) | 50 (59%) | .39 |
| 8-Fr catheter | 207 (49%) | 175 (52%) | 32 (38%) | .03 |
| Dual injection | 367 (87%) | 302 (89%) | 65 (76%) | .02 |
| Intervention | ||||
| Drug-eluting stent | 294 (87%) | NA | ||
| Bare metal stent | 20 (6%) | NA | ||
| Drug-eluting and bare-metal stent | 15 (4%) | NA | ||
| Balloon | 10 (3%) | 1 (1.2%) | ||
| Retrograde approach | 94 (22%) | 69 (20%) | 25 (29%) | .07 |
| IVUS | 61 (14%) | 56 (17%) | 5 (6%) | .06 |
| Duration (min) | 105 ± 41 | 106 ± 42 | 102 ± 39 | .43 |
| Fluoroscopy dose (cGy/m²) | 26 037 ± 2066 | 26 403 ± 2222 | 24 867 ± 13 019 | .57 |
| Contrast volume (mL) | 367 ± 175 | 377 ± 177 | 327 ± 158 | .002 |
IVUS, intravascular ultrasound. | ||||
Table 4. Multivariate predictors
| Failed procedure | HR | HR | P |
|---|---|---|---|
| Previous CABG | 7.51 | 2.83-19.90 | .0001 |
| Moderate-to-severe tortuosity | 3.78 | 2.02-7.08 | .0001 |
| ACS setting | 2.42 | 1.26-4.61 | .008 |
| Tandem occlusion | 2.32 | 1.11-4.87 | .027 |
| Lack of dual injection | 2.43 | 1.14-5.55 | .027 |
| Cardiovascular mortality | HR | HR | P |
| Renal failure (< 60 mL/min) | 5.67 | 1.95-16.48 | .002 |
| LAD occlusion | 3.30 | 1.12-9.74 | .032 |
| Failed procedure | 7.14 | 2.44-20.0 | .0001 |
ACS, acute coronary syndrome; CABG, coronary artery bypass graft; LAD, left anterior descending coronary artery. | |||
Twenty-six coronary dissections (6.2%) and 21 femoral hematomas (5%) were the most common procedural complications of all. In the course of the attempts, perforations occurred in 5 successful cases (1.5%) and in 9 failed cases (10.8%). However, emergent pericardiocentesis due to cardiac tamponade was required in 1 patient only. Contrast-induced nephropathy occurred in 8 successful cases (2.5%) and in 1 failed case (3.1%). One patient died during hospitalization due to cardiogenic shock that occurred 24 hours after a failed CTO attempt.
The differences seen among the 3 time periods led us to think that procedural technical advances, the operator’s increasing skills, and the improvements made in the assessment of the patients’ profile and selection of the lesions, contributed to the 87% rate of success reported at the final time frame. The temporal trends shown on table 5 describe the techniques developed in each corresponding period, not that all procedures were performed with that technique. Since June 2013 numerous cases have been successfully completed using the dissection/re-entry technique.The median follow-up was 39.7 months [22–102]. Follow-up information was available in 407 patients (99.8%). Clinical outcomes during follow-up are shown on table 6.
Table 5. Temporal trends in baseline angiographic characteristics, procedural data, and results
| 1st period (2002-2007) | 2nd period (2007-2011) | 3rd period (2011-2017) | Total | P | |
|---|---|---|---|---|---|
| Age | 62 ± 16 | 63 ± 11 | 64 ± 11 | 63 ± 12 | NS |
| Multivessel disease | 61.7% | 60.1% | 82% | 70% | .0001 |
| ACS setting | 36.1% | 21.8% | 23.6% | 24.3% | .025 |
| Previous CABG | 9.8% | 10.0% | 3.9% | 7.3% | .020 |
| LAD | 27.9% | 33.3% | 28.5% | 30.4% | NS |
| Length (mm) | 23 ± 14 | 22 ± 13 | 21 ± 18 | 23 ± 16 | NS |
| J score > 3 | 45.0% | 44.8% | 45.8% | 45.2% | NS |
| Rentrop grade 3 cc. | 44.8% | 62.8% | 39.4% | 48.6% | .0001 |
| Femoral access | 49.2% | 68.0% | 62.6% | 62.5% | .016 |
| 8-Fr catheter | 11.7% | 58.3% | 54.3% | 48.8% | .0001 |
| Dual injection | 65.0% | 90.1% | 92.1% | 86.5% | .0001 |
| Retrograde approach | 1.6% | 23.3% | 28.8% | 22.1% | .0001 |
| IVUS | 21.2% | 18.3% | 11.1% | 14.4% | .033 |
| Fluoroscopy time (cGy/m²) | 33245 | 30310 | 19830 | 26037 | .0001 |
| Contrast volume (mL) | 453 ± 208 | 434 ± 178 | 281 ± 127 | 367 ± 175 | .0001 |
| Success rate | 57% | 81% | 87% | 80% | .001 |
| More widely used wires | Polymer coated wires (Whisper ES or MS, Pilot 50, 150 or 200, Abbott Vascular, United States) and tapered, stiff wires (Confianza Pro 12, Asahi Intecc., Japan). Used in 58%. | Runthrough wire (Terumo, Japan) and nontapered, stiff wires (Miracle 3 or 6 and Ultimate Bross 3, Asahi Intecc., Japan). Used in 62%. | Runthrough and nontapered, stiff wires widely used (59%). Sion and Gaia wires (Asahi Intecc., Japan) were used in 21%. | ||
| Specific devices and techniques | Antegrade approach only. Parallel and seesaw wiring techniques. | Retrograde approach, Corsair specific catheter (Asahi Intecc., Japan) and Guideliner (Vascular Solutions, United States). Kissing and reverse CART techniques. | Double lumen Nhancer catheter (Interventional Medical Device Solutions, The Netherlands). Hybrid techniques with the CrossBoss and Styngray catheters (Boston Scientific, United States). | ||
ACS, acute coronary syndrome; CABG, coronary artery bypass graft; ES, extra support; IVUS, intravascular ultrasound; LAD, left anterior descending coronary artery; MS, medium support. | |||||
Table 6. Clinical outcomes at follow-up
| All (n = 424) | Success (n = 339) | Failure (n = 85) | P | |
|---|---|---|---|---|
| Overall mortality | 64 (15.1%) | 40 (11.8%) | 24 (28.2%) | .001 |
| Cardiovascular mortality | 24 (5.7%) | 12 (3.6%) | 12 (14.1%) | .001 |
| Myocardial infarction | 10 (2.4%) | 8 (2.4%) | 2 (2.4%) | .99 |
| Target vessel revascularization | 45 (10.6%) | 34 (10.1%) | 11 (12.9%) | .44 |
| Target lesion revascularization | 40 (9.5%) | 31 (9.2%) | 9 (10.6%) | .69 |
| CTO stent thrombosis | ||||
| Definite | 5 (1.5%) | NA | ||
| Probable | 1 (0.3%) | NA | ||
| MACE | 68 (16.1%) | 47 (13.9%) | 21 (24.7%) | .0015 |
CTO, chronic total coronary occlusion; MACE, major adverse cardiovascular events (cardiovascular death, myocardial infarction or need for surgical or percutaneous target vessel revascularization). | ||||
In the success group, 33 restenosis (9.7%) were angiographically diagnosed, 42% of which ended up being occlusive. Target lesion revascularization was achieved in 31 of these restenotic lesions (9.2%). Four of the 5 cases of definite thrombosis corresponded to a successfully opened right coronary artery.
One case of severe radiodermatitis was identified and it was successfully treated with local surgery 6 years after the intervention.
A remarkable difference in MACE was observed in favor of the success group, mainly driven by a lower rate of cardiovascular mortality. The cumulative cardiac survival and MACE survival curves associated with the success or failure of the PCI are shown on figure 2 and figure 3.
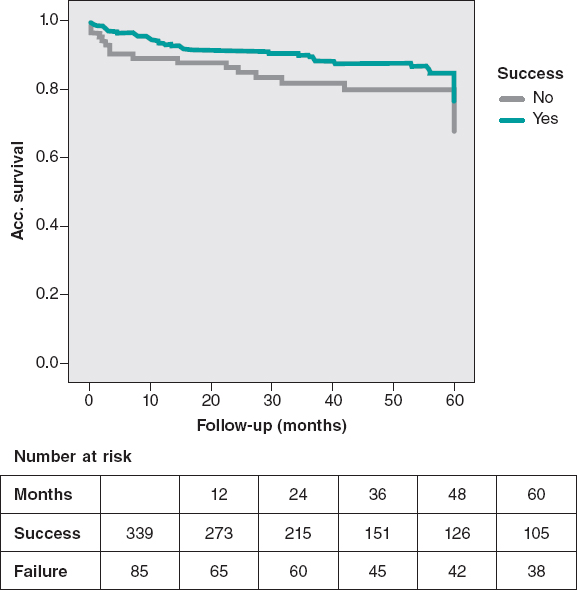
Figure 2. MACE-free at the 5-year follow-up. The rate of MACE (cardiovascular death, infarction, and surgical or percutaneous TVR) was lower in successful cases (P = .03).
MACE, major adverse cardiovascular events (cardiovascular death, myocardial infarction or need for surgical or percutaneous TVR); TVR, target vessel revascularization.
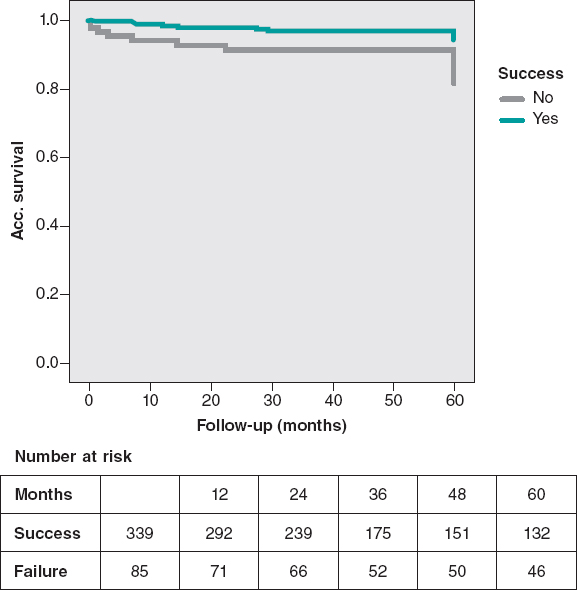
Figure 3. Cardiovascular mortality-free at the 5-year follow-up. Significant lower cardiovascular mortality in the success group (P = .005).
The multivariate analysis confirmed that a past medical history of chronic kidney disease with creatinine clearance < 60 mL/min, LAD occlusions, and procedural failure were independent predictors of cardiovascular mortality (table 4). Actually, increased mortality-related success rates were only seen in cases of failed LAD-CTO recanalization attempts compared to failed non-LAD CTO attempts (35% vs 9% P = .012).
DISCUSSION
These are the main results of this registry: a) the higher rates of success seen over the last 15 years confirm the improvements made in CTO recanalization devices and in the operator’s skills; b) the recanalization of CTOs shows high rates of success (80.0%) and low rates of complications; c) the rates of success were significantly lower in patients with previous CABG, moderate-to-severe lesion tortuosity, tandem occlusions, lack of dual injection, and patients with CTO treated in the ACS setting; d) successful procedures, especially in LAD occlusions, were associated with lower rates of cardiovascular mortality and MACE at the long-term follow-up.
The recanalization of the CTO is still uncertain and is not yet supported by randomized clinical trials. Several retrospective observational studies8-10 provide evidence that support this strategy. The results found in this analysis are consistent with previously published data, but disagree with others.11,12. In this sense, the more recent registries show better results regarding cardiovascular and overall mortality.13,14
Regarding randomized clinical trials, the EUROCTO trial revealed that the PCI of a CTO improves health status with improvements in angina frequency in patients with stable angina.15 However, the EXPLORE trial did not reveal any differences in the left ventricular function of patients with ST-segment elevation myocardial infarction. The DECISION-CTO showed similar inter-group rates of death, MI, stroke or TLR in patients with ACS or stable angina at the 3-year follow-up.16,17 The most recent clinical trial (REVASC) did not show an improved regional myocardial function. Although it was underpowered to measure clinical outcomes, it showed the advantage of performing the PCI of a CTO for clinically-driven repeat revascularization.18
Several characteristics of the current study should be emphasized to put the results into perspective. We believe this series of CTOs to be the big picture of interventional cardiology regarding CTOs since the start of the drug-eluting stent era until the arrival of contemporary new technologies. The study is based on a large cohort of consecutive patients from a single center. Most of them had multivessel disease and were treated in different time frames according to a specific dedicated CTO program.
Among the procedural characteristics that could explain the lower rates of success obtained with CTOs in the ACS setting we found the lowest use of retrograde approach and 8-Fr catheters in non-adequately staged procedures.
Regarding procedural features, the use of IVUS was limited to cases that required assessment of the distal vessel diameter and to optimize procedures with severe calcifications. It is very likely that more IVUS-guided procedures should have been performed.
Regarding variables related to procedural outcomes in the multivariable analysis, previous CABGs and more complicated CTOs were associated with failure as shown by other registries.13 However, intralesional tortuosity seems to us like the most consistent multivariable predictor with greater contribution to the model due to its narrow confidence interval. It might be possible that the inclusion of several angiographic variables in the regression model is responsible for the J-score not becoming an independent predictor. The high rate of retrograde procedures reveals the complexity of the CTOs in our series with J score > 3 in 45% of cases.
After dividing the series into 3 different periods of time, significant improvements in the rates of success were emphasized. As a result, we saw some interesting changes over time, such as the contribution of the retrograde approach to success. Considering that 73% of retrograde procedures were successful, it can be said that this technique led to a 19% increase in the rates of success in absolute terms. The rate of complications was quite similar to that from other studies.2-4,8-14
Our data provide additional evidence on the lower rate of cardiovascular mortality reported in patients with successful CTO recanalization in the long-term follow-up. As a matter of fact, the success of the PCI was a strong independent predictor of survival as several observational studies and 1 meta-analysis have consistently suggested.13,14,19
Possible explanations of the survival benefit from revascularizing a CTO may include a better left ventricular function and more tolerance for future acute coronary occlusive events.20 However, this cannot be confirmed as we didn’t measure the left ventricular ejection fraction systematically during follow-up. However, the trend showing a worst clinical profile in failed CTOs would validate this statement.
The role of LAD occlusions is decisive, as it seems an independent predictor of mortality. It should be mentioned that this effect of LAD occlusions on cardiovascular mortality was basically due to the higher mortality rate of failed cases compared to LAD recanalization attempts. The fact that LAD CTOs are much easier to open than CTOs located in other vessels makes LAD attempts not only feasible but also mandatory.
In conclusion, we think that this study —performed in a contemporary single cardiac catheterization laboratory for a long period of time practice in the drug eluting stent era— features new information on procedural results and long-term outcomes on CTO recanalizations.
This study was a prospective analysis and is subject to the limitations inherent to this type of research. The study does not allow us to draw any comparisons with other therapeutic strategies like medical therapy or CABG. Patients with failed procedures had different clinical and angiographic characteristics, which may have impacted prognosis.
Angiographic characteristics were not analyzed in a core lab but provided by a local investigator. There was no adjudication of clinical outcomes by a clinical events committee.
CONCLUSIONS
The implementation of a specific PCI program for CTOs has been associated with higher rates of success over time thanks to growing expertise and new technical advances. The rate of procedural success was lower when there was a history of previous CABG, moderate-to-severe lesion tortuosity, tandem occlusions, lack of dual injection, and in CTOs diagnosed in the ACS setting. Preserved renal function and successful recanalization —especially of the LAD— were associated with a lower rate of cardiovascular mortality in the long-term follow-up.
CONFLICTS OF INTEREST
J.M. de la Torre is the Editor-in-chief of REC: Interventional Cardiology; the editorial procedure established by REC: Publications was followed to guarantee the fair and unbiased handling of the manuscript.
WHAT IS KNOWN ABOUT THE TOPIC?
- CTOs are the most complex lesions to treat, and the prognostic benefit associated with their recanalization has not been properly established and if so, it could be selective.
- Most registries are limited in size and feature results in restricted time frames, often focused on specific devices, and not on long-term outcomes.
- The results of specific CTO programs in the long run have not been reported.
WHAT DOES THIS STUDY ADD?
- Our study describes the very long-term evolution of a PCI program for CTOs including the management and outcomes of PCI attempts on CTOs from 2002-2017.
- Our data, collected since the start of the drug-eluting stent era, confirm that implementing a program leads to higher rates of success over time. Independent predictors of PCI failure were identified in this large cohort.
- Lower rates of cardiovascular mortality were found in patients with successful recanalizations in the long-term follow-up.
- Also, the study provided new insights on the role played by LAD-CTO recanalizations on better outcomes.
REFERENCES
1. Anderson HV, Shaw RE, Brindis RG, et al. A contemporary overview of percutaneous coronary interventions. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). J Am Coll Cardiol. 2002;39:1096-1103.
2. Suero JA, Marso SP, Jones PJ, et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of chronic total occlusion in native coronary arteries:a 20-year experience. J Am Coll Cardiol. 2001;38:409-414.
3. Hoye A, van Domburg RT, Sonnenschein K, et al. Percutaneous coronary intervention for chronic total occlusions:the Thoraxcenter experience 1992-2002. Eur Heart J. 2005;26:2630-2636.
4. Noguchi T, Miyazaki S, Morii I, et al. Percutaneous transluminal coronary angioplasty of chronic total occlusions. Determinants of primary success and long-term clinical outcome.Cathet Cardiovasc Interv.2000;49:258-264.
5. Di Mario C, Sorini Dini C MD, Werner GS. Thousand Registries Are Not Worth a Randomized Trial. Also True for Chronic Total Occlusions?J Am Coll Cardiol Intv. 2017;10:1535-1537.
6. Di Mario C, Werner GS, Sianos G, et al. European perspective in the recanalisation of Chronic Total Occlusions:consensus document from the EuroCTO Club. Eurointervention. 2007;3:30-43.
7. Morino Y, Kimura T, Hayashi Y, et al. In-hospital outcomes of contemporary percutaneous coronary intervention in patients with chronic total occlusion insights from the J-CTO Registry (Multicenter CTO Registry in Japan). J Am Coll Cardiol Intv. 2010;3:143-151.
8. Olivari Z, Rubartelli P, Piscione F, et al.;TOAST-GISE Investigators. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions:data from a multicenter, prospective, observational study (TOAST-GISE). J Am Coll Cardiol. 2003;41:1672-1678.
9. Aziz S, Stables RH, Grayson AD, et al. Percutaneous coronary intervention for chronic total occlusions:improved survival for patients with successful revascularization compared to a failed procedure. Catheter Cardiovasc Interv. 2007;70:15-20.
10. Valenti R, Migliorini A, Signorini U, et al. Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur Heart J. 2008;29:2336-2342.
11. Prasad A, Rihal CS, Lennon RJ, et al. Trends in outcomes after percutaneous coronary intervention for chronic total occlusions. A 25-year experience from the Mayo Clinic. J Am Coll Cardiol. 2007;49:1611-1618.
12. Labriolle A, Bonello B, Roy P, et al. Comparison of Safety, Efficacy, and Outcome of Successful Versus Unsuccessful Percutaneous Coronary Intervention in “True“Chronic Total Occlusions. Am J Cardiol.2008;102:1175-1181.
13. Borgia F,Viceconte N, Ali O, et al. Improved cardiac survival, freedom from MACE and angina-related quality of life after successful percutaneous recanalization of coronary artery chronic total occlusions. Int J Cardiol. 2012;161:31-38.
14. Tsai TT, Stanislawski MA, Shunk KA, et al. Contemporary Incidence, Management, and Long-Term Outcomes of Percutaneous Coronary Interventions for Chronic Coronary Artery Total Occlusions Insights From the VA CART Program. J Am Coll Cardiol Intv. 2017;10:866-875.
15. Werner GS. A Randomized Multicentre Trial to Evaluate the Utilization of Revascularization or Optimal Medical Therapy for the Treatment of Chronic Total Coronary Occlusions (EuroCTO) trial. Presented at;the PCR Congress Scientific Session 2017:Paris. Available online:https://www.pcronline.com/Cases-resources-images/Resources/Course-videos-slides/2017/Late-breaking-trials-and-trial-updates2?auth =true. Accessed 19 Dec 2019.
16. Park SJ. Drug-Eluting Stent Implantation Versus Optimal Medical Treatment in Patients With Chronic Total Occlusion (DECISION-CTO) trial. Presented at:the American College of Cardiology (ACC) 2017 Scientific Session. Washington, DC. Available online: http://www.acc.org/latest-in-cardiology/clinical-trials/2017/03/17/08/40/decision-cto. Accessed 19 Dec 2019.
17. Henriques JP, Hoebers LP, Råmunddal T, et al. :EXPLORE Trial Investigators. Percutaneous Intervention for Concurrent Chronic Total Occlusions in Patients With STEMI:The EXPLORE Trial. J Am Coll Cardiol.2016;68:1622-1632.
18. Mashayekhi K. REVASC:a randomized trial to assess recovery of left ventricular function after PCI of coronary artery chronic total occlusions. Presented at;TCT 2017. October 31, 2017:Denver, CO). Available online: https://www.tctmd.com/news/revasc-cto-pci-does-not-improve-lv-function-seems-provide-symptom-relief. Accessed 19 Dec 2019.
19. Khan MF, Wendel CS, Thai HM, et al. Effects of percutaneous revascularization of chronic total occlusions on clinical outcomes:a meta-analysis comparing successful versus failed percutaneous intervention for chronic total occlusion. Catheter Cardiovasc Interv. 2013;82:95-107.
20. Silva JC, Rochitte CE, Junior JS, et al. Late coronary artery recanalization effect on left ventricular remodelling and contractility by magnetic resonance imaging. Eur Heart J. 2005;26:36-43.
Corresponding author: Servicio de Cardiología, Hospital Galdakao-Usansolo, Labeaga Auzoa, 48960 Galdakao, Vizcaya, Spain
E-mail address: al.subinas@gmail.com (A. Subinas).












