QUESTION: What’s your interpretation of the REVIVED BCIS2 trial? Which, would you say, are its most positive and debatable features?
ANSWER: The REVIVED BCIS21 trial randomized stable patients with ischemic dilated cardiomyopathy to undergo percutaneous coronary intervention (PCI) along with optimal medical therapy (OMT) or OMT alone without revascularization. The trial included patients with left ventricular ejection fraction ≤ 35%, extensive coronary artery disease, and viability in 4 or more segments amenable to PCI. The results proved that the 2 strategies offered comparable outcomes regarding the primary composite endpoint of all-cause mortality or hospitalization-related heart failure (37.2% vs 38.0%; hazard ratio, 0.99; 95% confidence interval, 0.78-1.27; P = .96). There were no differences in the changes in left ventricular ejection fraction recorded at 6 months and at 1 year, with improvement confirmed in both groups.2 Previously, the STICH trial2,3 had demonstrated that surgical revascularization combined with OMT provided long-term overall survival benefits in patients with ischemic dilated cardiomyopathy, despite an initial increase in surgery-related mortality. Therefore, it was believed that the REVIVED BCIS2 trial, with the lower perioperative risk associated with PCI, could equal or even exceed these benefits. However, things have changed since the publication of the STICH trial, including improvements in pharmacological therapy, greater use of devices such as implantable cardioverter-defibrillators and cardiac resynchronization therapy, closer follow-up of patients with heart failure, and widespread use of cardiac rehabilitation programs. The REVIVED BCIS2 trial proves that current OMT with the use of these resources in patients with ischemic dilated cardiomyopathy provides certain benefits regarding mortality and heart failure-related hospitalizations that are not enhanced by revascularization, at least with the percutaneous approach.
The most positive feature of this study is that it addresses an open question on the need for the systematic use of PCI in these patients and it does so with a methodologically appropriate clinical trial. The most debatable aspects are the definition of ischemic dilated cardiomyopathy and the achievement of complete revascularization. To characterize cardiomyopathy as ischemic, a BCIS-Jeopardy score4 ≥ 6 was required, with 49% of the patients having 2-vessel disease, while the median number of lesions and vessels treated per patient in the PCI group was 2, and complete revascularization was achieved in 71% of the patients.1
Q.: The STICH trial2 showed benefits beyond the 5- to 10-year mark, but in the REVIVED BCIS2 trial, the median follow-up was 3 to 4 years, although the patients’ age in the 2 studies was very different. What do you make of this?
A.: In the STICH trial, the all-cause mortality curves (primary endpoint) began to separate at the 2-year follow-up, and the original publication of the study, with a median follow-up of 4.7 years, failed to show a significant reduction in the primary endpoint. What demonstrated the prognostic benefit of cardiac surgery in addition to OMT was extending the follow-up to 10 years (median, 9.8 years).3 This reveals several points: on the one hand, the increased perioperative morbidity and mortality and, on the other hand, the long-term benefits of alleviating myocardial ischemia, leading, among other things, to lower rates of reinfarction and ventricular arrhythmias5 This is especially relevant when treating younger patients, whose lower surgical risk and longer life expectancy allow us to actually see clinical benefits. Although PCI was not associated with higher perioperative mortality in the REVIVED BCIS2 trial, there were no significant separations of the primary endpoint curves during the study.
We need to obtain data from a longer follow-up to detect any potential benefits associated with PCI. Additionally, the mean age of the REVIVED trial population was 70 years (compared with the median of 60 years in the STICH trial), making it less likely to achieve the same long-term benefits associated with surgical revascularization.
Q.: What was the clinical profile of these patients, and to what extent was their medical therapy optimized during randomization? Do you think they could have progressed to advanced stages of cardiomyopathy, and if so, could that have impacted the outcomes?
A.: The participants’ clinical profile was typical of this kind of disease. Most were men (88%), and 56% of them had a history of hypertension, 41% had diabetes, and 53% had previous myocardial infarction: 67% were angina-free, 20% had a history of previous PCI, and 5% had undergone surgical revascularization. They were in a favorable functional class (74% were in NYHA class I or II), while only 33% had been hospitalized due to heart failure in the previous 2 years, and the median N-terminal pro-brain natriuretic peptide (NT-proBNP) was 1400 pg/mL. Therefore, their baseline characteristics do not support the assumption that they were in an advanced stage of the disease.6 Although mortality during follow-up was high (32%), it was consistent with what we would expect of patients with ischemic dilated cardiomyopathy,7,8 while the rate of heart failure-related hospitalizations was relatively low (15%). Based on their clinical profile, these patients would have been eligible for improvement with percutaneous revascularization. When the participants were randomized, 89% were on an angiotensin-converting enzyme inhibitor, combined with an angiotensin II receptor antagonist or sacubitril-valsartan, 91% were on beta-blockers, and 49% were on mineralocorticoid receptor antagonists. Although this is a well-optimized regimen, there is still room for improvement, because only 5% of the participants were on sacubitril-valsartan, half of them were not on aldosterone antagonists, and sodium-glucose co-transporter-2 inhibitors were not yet considered part of the foundational treatment of heart failure. Indeed, at the 2-year follow-up, only 20% were on sacubitril-valsartan and 55% were on mineralocorticoid receptor antagonists. Additionally, a low percentage of participants (23%) had a defibrillator or a cardiac resynchronizer.1
Q.: Do you agree that the trial questions the validity of viability tests? Although a 25% cutoff value for late gadolinium enhancement was established in cardiac magnetic resonance, in cases with 25% to 50% enhancement it was left to the local investigators’ discretion to use another imaging modality, such as dobutamine echocardiography. Do you think places doubt on the criteria applied to the trial?
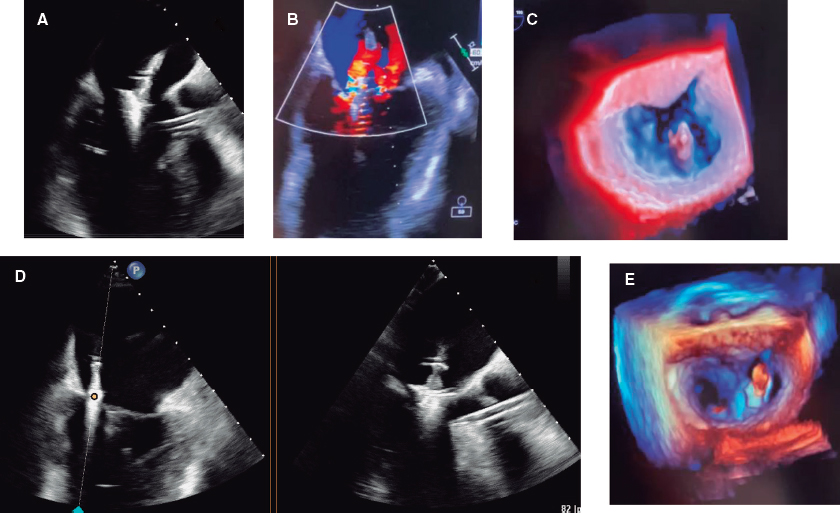
A.: The STICH trial viability subanalysis already cast doubt on the utility of detecting a viable myocardium through single-photon emission computed tomography or dobutamine echocardiography to predict favorable outcomes after revascularization.9 The REVIVED BCIS2 also failed to demonstrate that viability-guided revascularization is able to reduce mortality or improve cardiac remodeling. In this trial, a larger number of dysfunctional—yet viable—myocardial segments were not associated with prognosis or with the possibility of improved ventricular function, whereas less myocardial scarring did predict a more favorable prognosis and a higher likelihood of reverse remodeling. This was independent of the baseline ejection fraction and extent of coronary artery disease.10 The results should prompt us to revisit the notion of hibernating myocardium and avoid basing the coronary revascularization strategy solely on viability tests.11 In this trial, cardiac magnetic resonance was the preferred imaging modality to assess viability (used in 71% of the patients). Considering segments with a maximum late enhancement of 25% as viable was a positive aspect, because participants with higher theoretical probabilities of improving after PCI were selected. Although another additional imaging modality could be used in patients with late enhancement between 26% and 50%, in practice, only 8 patients1 received more than 1 viability test, so this does not seem to be an important point.
Q.: Considering the possibility that coronary artery disease can be concurrent with cardiomyopathy, without it necessarily being the main cause, do you think there is a specific patient profile that could benefit from PCI or, at the very least, could be worth further study?
A.: The subgroup analysis did not show any significant treatment interaction in the prespecified subgroups of interest.1 However, data from the study allow us to speculate on which participants might benefit more from PCI. The trial included few patients with limiting angina, thus making the findings less applicable to these patients. The study showed differences in favor of PCI regarding quality of life at the 6- and 12-month follow-up (becoming equal at 2 years in the 2 groups), suggesting that PCI might be crucial for patients with angina.5 Additionally, PCI-treated patients showed a trend toward fewer appropriate implantable cardioverter-defibrillator therapies,1 indicating that revascularization could be more beneficial in individuals in whom ventricular arrhythmias are an issue. Other subgroups of interest would be patients with more extensive coronary artery disease, those with complete revascularization, and those with greater ventricular dysfunction. Future publication of these patients’ outcomes could help in the decision-making process.6
Finally, while surgical revascularization should be the preferred strategy for patients with ischemic dilated cardiomyopathy,7 PCI should still play a role in the management of young patients with significant coronary artery disease and high surgical risk or poor distal beds. With the current evidence available and contemporary OMT, a clinical trial should be conducted comparing 3 therapeutic strategies: isolated OMT, OMT along with surgical revascularization, and OMT alongside PCI in patients with ischemic dilated cardiomyopathy. The selection criteria should not consist of viability but rather the feasibility of achieving complete myocardial revascularization in regions at-risk, and follow-up should be long-term.
FUNDING
None reported.
CONFLICTS OF INTEREST
None.
REFERENCES
1. Perera D, Clayton T, O'Kane PD, et al. Percutaneous revascularization for ischemic left ventricular dysfunction. N Engl J Med. 2022;387:1351-1360.
2. Velazquez EJ, Lee KL, Deja MA, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364:1607-1616.
3. Velazquez EJ, Lee KL, Jones RH, et al. Coronary-Artery Bypass Surgery in Patients with Ischemic Cardiomyopathy. N Engl J Med. 2016;374:1511-1520.
4. Morgan H, Ryan M, Briceno N, et al. Coronary Jeopardy Score Predicts Ischemic Etiology in Patients With Left Ventricular Systolic Dysfunction. J Invasive Cardiol.2022;34:E683-E685.
5. Ezad SM, Ryan M, Perera D. Can Percutaneous Coronary Intervention Revive a Failing Heart?Heart Int. 2022;16:72-74.
6. Vergallo R, Liuzzo G. The REVIVED BCIS2 trial:percutaneous coronary intervention vs. optimal medical therapy for stable patients with severe ischaemic cardiomyopathy. Eur Heart J. 2022;43:4775-4776.
7. Liga R, Colli A, Taggart DP, Boden WE, De Caterina R. Myocardial Revascularization in Patients With Ischemic Cardiomyopathy:For Whom and How. J Am Heart Assoc. 2023;12:e026943.
8. Perera D, Clayton T, Petrie MC, et al. Percutaneous Revascularization for Ischemic Ventricular Dysfunction:Rationale and Design of the REVIVED BCIS2 Trial:Percutaneous Coronary Intervention for Ischemic Cardiomyopathy. JACC Heart Fail. 2018;6:517-526.
9. Bonow RO, Maurer G, Lee KL, et al. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med. 2011;364:1617-1625.
10. Perera D. Effect of Myocardial Viability, Functional Recovery and ICP on Clinical Outcomes in the REVIVED BCIS2 Trial. En:American College of Cardiology 2023 Scientific Session;2023 March 4-6;New Orleans, LA, USA. Available at: https://accanywhere.acc.org/media/c2f4157c-0bef-4d69-87b4-ac6ab6224e07. Accessed 9 Jul 2023.
11. Ryan M, Morgan H, Chiribiri A, Nagel E, Cleland J, Perera D. Myocardial viability testing:all STICHed up, or about to be REVIVED?Eur Heart J. 2022;43:118-126.RECIC_23_064
* Corresponding author.
E-mail address: a.m.iniesta84@gmail.com (A.M. Iniesta Manjavacas).