This is the case of a 68-year-old woman admitted due to polytrauma following a fall from a great height. While on mechanical ventilation she shows signs of self-limited hemoptysis without hemodynamic impairment. Several computed tomography (CT) scans reveal the presence of a 20 mm × 15 mm × 15 mm pseudoaneurysm at right upper lobe branch level without any data of active bleeding or erosion, but presence of progressive growth (5 mm) in 3 successive CT scans performed within 5 days (figure 1, arrows). Given the risk of rupture, percutaneous coronary intervention is attempted to seal the pseudoaneurysm. All the corresponding informed consents were obtained.
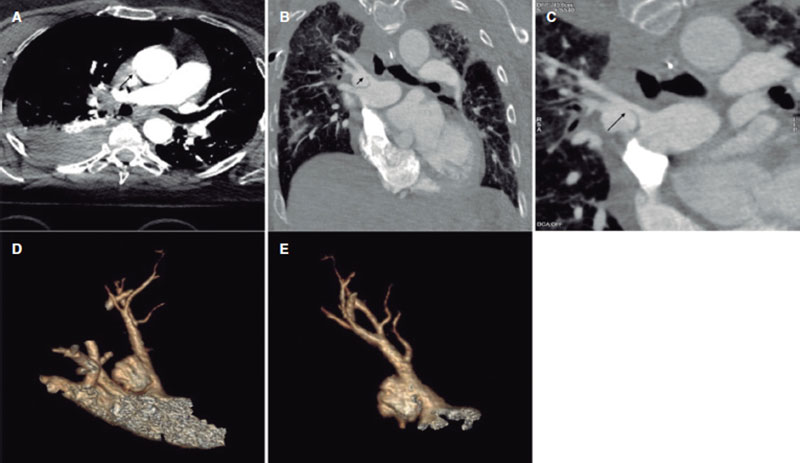
Figure 1.
The angiography confirms the presence of the pseudoaneurysm including the bifurcation of 2 lobar branches (figure 2A, arrow; video 1 of the supplementary data) unsuitable for sealing with coils or intravascular plug and without a clear proper landing zone for stenting, which is why it is decided to implant a covered stent towards the upper subdivision to isolate it. Using a Judkins right 4 catheter (Launcher, Medtronic, United States) selective catheterization is achieved by advancing a 0.035 in guidewire. Afterwards, a 7-Fr Destination sheath (Terumo, Japan) is advanced through which a 6 mm × 28 mm Begraft expanded polytetrafluoroethylene (ePTFE)-covered stent (Bentley InnoMed, Germany) is implanted. The stent proximal region is postdilated with a 10 mm × 30 mm semicompliant Crystal Balloon (Balt, France). The pseudoaneurysm total exclusion is confirmed on the angiographic follow-up (figure 2B-F, arrow; video 2 of the supplementary data). The patient’s clinical progression is good, and she currently remains asymptomatic without clinical or radiographic data of pulmonary infarction at 6-month follow-up.
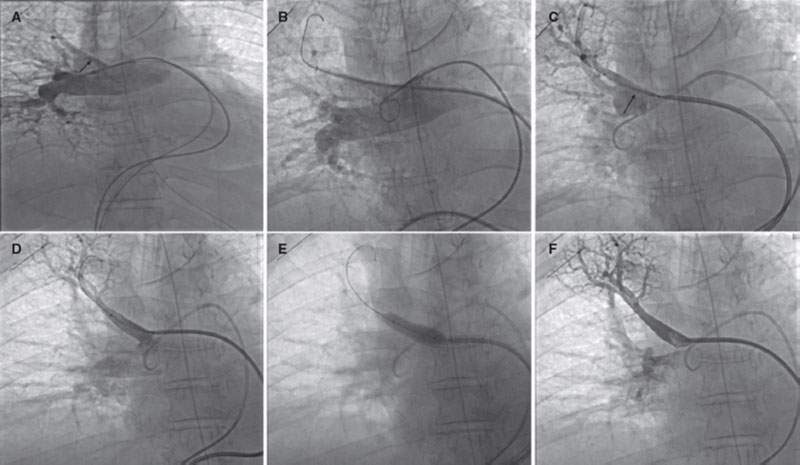
Figure 2.
FUNDING
None reported.
AUTHORS’ CONTRIBUTIONS
All the authors contributed equally to the drafting of this manuscript.
CONFLICTS OF INTEREST
None whatsoever.
SUPPLEMENTARY DATA
Vídeo 1. Fernández González L. DOI: 10.24875/RECICE.M22000350
Vídeo 2. Fernández González L. DOI: 10.24875/RECICE.M22000350
* Corresponding author.
E-mail address: luisfg82@hotmail.com (L. Fernández González).