Abstract
Introduction and objectives: Complete revascularization is recommended for the management of ST-segment elevation myocardial infarctions (STEMI). Although physiological evaluation is recommended for the assessment of nonculprit lesions, in this context, the use of fractional flow reserve (FFR) is limited. The quantitative flow ratio (QFR) is a new angiography-based tool for the assessment of functional severity. We evaluated the functional changes occurring in nonculprit lesions after the acute phase and the QFR/FFR correlation in non-infarct-related arteries.
Methods: We recruited all patients with multivessel disease admitted to our institution due to STEMI from January 2016 through December 2017 who underwent staged interventions for the management of nonculprit lesions. We conducted a retrospective QFR assessment at both the index and the staged procedures and drew a comparison. Also, the QFR/FFR concordance and agreement were prospectively evaluated between January and May 2018 in a cohort of patients with STEMI and multivessel disease.
Results: We analyzed a total of 131 lesions in 88 patients. During the initial procedure, 93.1% of the lesions were considered significant based on the angiography compared to only 56.3% studied through QFR (P ≤ .001). The QFR reassessment during the staged intervention brought this percentage down to 32.1%. All patients with QFR values ≥ 0.82 during the index procedure remained nonsignificant at the staged assessment. Both the FFR and the QFR were compared in 12 patients showing good agreement and a mean difference of 0.015 ± 0.02 (P > .1).
Conclusions: The QFR-based physiological assessment of nonculprit lesions in STEMI patients led us to consider nonsignificant 40% of the lesions classified as significant by the angiography. Also, the QFR significantly increased from the acute phase to the staged procedure, indicative that in patients with QFR ≥ 0.82 in the acute phase a new coronary angiography procedure may be unnecessary.
Keywords: Fractional flow reserve. Quantitative flow ratio. Non-infarct-related artery. STEMI.
Resumen
Introducción y objetivos: En pacientes con infarto agudo de miocardio con elevación del segmento ST y enfermedad multivaso se recomienda la revascularización completa. La evaluación funcional con reserva fraccional de flujo (RFF) de las arterias no culpables del infarto es limitada. El quantitative flow ratio (QFR) es una herramienta basada en la angiografía para valorar la gravedad funcional de las lesiones. Se analizaron la evolución funcional de las arterias no culpables del infarto tras la fase aguda y la correlación QFR/RFF en este contexto.
Métodos: Se incluyeron pacientes ingresados con infarto agudo de miocardio con elevación del segmento ST entre enero de 2016 y diciembre de 2017, con enfermedad multivaso y revascularización diferida de lesiones no culpables. Se evaluaron retrospectivamente con QFR durante el procedimiento índice y el diferido, y se evaluó la concordancia QFR/RFF de manera prospectiva entre enero y mayo de 2018.
Resultados: Se incluyeron 131 lesiones de 88 pacientes. Durante el procedimiento índice, el 93,1% de las lesiones se consideraron significativas de acuerdo con la angiografía, pero solo el 56,3% cuando se evaluaron con QFR (p < 0,001). El QFR del procedimiento diferido demostró una mayor reducción, con solo el 32,1% de las lesiones significativas. Todos los pacientes con QFR ≥ 0,82 durante el procedimiento índice continuaron con estenosis no significativas en la evaluación diferida. La comparación del QFR y la RFF en este contexto demostró buen acuerdo, con una diferencia media de 0,015 ± 0,02 (p > 0,1).
Conclusiones: La evaluación fisiológica mediante QFR de las lesiones en arterias no culpables del infarto descartó la significación en el 40% de las consideradas significativas por angiografía. El valor de QFR se incrementó significativamente del procedimiento índice al diferido, lo que sugiere que en pacientes con QFR ≥ 0,82 en la fase aguda podrían evitarse procedimientos diferidos innecesarios.
Palabras clave: Reserva fraccional de flujo. Quantitative flow ratio. Arteria no culpable. IAMCEST.
Abbreviations: FFR: fractional flow reserve. IRA: infarct-related artery. PCI: percutaneous coronary intervention. QFR: quantitative flow ratio. STEMI: ST-segment elevation myocardial infarction.
Introduction
Up to 50% of the patients admitted with ST-elevated acute myocardial infarction (STEMI) show multivessel disease1. Currently, complete revascularization is recommended before hospital discharge but the benefits of non-infarct-related artery (non-IRA) revascularization during primary percutaneous coronary interventions (PCI) or subsequent procedures is still controversial1. As a matter of fact, the strategy for the management of non-IRA has widely varied across landmark studies2-4.
The lack of consensus can be partially explained by the inaccuracy of angiography when assessing the severity of stenosis in non-IRA, with less than 30% to 50% of the lesions initially considered eligible for revascularization finally confirmed when assessed using the fractional flow reserve (FFR) 3-4. In particular, the severity of non‐IRA stenosis is more frequently overestimated during primary PCIs due to the hemodynamic conditions5.However, also in this context, the FFR measurements are usually invalid due to altered micro and macrovascular tone or microvascular flow obstruction3,6.Also, little has been said on the variability of FFR results over time in non‐culprit lesions. All these factors probably explain why most interventional cardiologists still use angiography as the only tool when it comes to deciding whether or not to treat nonculprit lesions7. The quantitative flow ratio (QFR) is a new tool to assess the severity of coronary stenosis based on computational fluids dynamics and the three-dimensional reconstruction of coronary angiography without a wire or the need for inducing hyperemia, which favorably correlates with FFR in stable coronary disease8-10. On the other hand, and although good agreement between FFR and QFR has also been suggested in the acute phase of myocardial infarctions11 it is widely known that the presence of microvascular dysfunction is associated with a worse correlation12.
We conducted one pilot study to conduct physiological assessments of the severity of non-IRA lesions based on the QFR during primary PCIs and in staged angiographies. Also, the FFR and QFR correlation was explored in this context.
Methods
Study design
Single-centre retrospective and observational study conducted in full compliance with the Declaration of Helsinki and after approval from the local ethics committee. All the patients included in this research provided informed consent for the anonymous use of their clinical and imaging data with scientific purposes only.
Study population
The study included consecutive patients of ≥ 18 years of age admitted to our institution due to STEMI between January 2016 and December 2017 with > 50% diameter coronary stenosis in nonculprit arteries after angiographic assessment. A two‐procedure strategy to achieve complete revascularization was decided in these patients during the index procedure. The staged procedure to treat the nonculprit lesions was conducted before hospital discharge as the standard care in this setting and according to the actual recommendations1. Consecutive patients with ≥ 18 years of age admitted to our institution due to STEMI between January 2018 and May 2018 with coronary stenosis after coronary angiographic assessment in non‐IRA lesions were prospectively included in our study to evaluate the concordance between the QFR and the FFR. The decision to conduct FFR assessments in these patients was made at operator’s discretion based on interventional and clinical criteria. The level of concordance and agreement between the FFR and the QFR were established here.
Exclusion criteria included inability to provide informed consent, lack of adequate coronary angiographic images for valid QFR analysis, presence of normal coronary arteries in the index procedure, surgical revascularization, and death or presence of other conditions precluding revascularization during the index procedure or contraindicating the staged procedure within the same admission.
Angiographic and physiological assessments
Standardized angiographic projections were performed in both procedures following the center acquisition protocol. The computation of the QFR was performed offline using specific software (QAngio XA 3D prototype, Medis Medical Imaging System, Leiden, the Netherlands). Details from the QFR assessment have been previously reported elsewhere13. In short, two projections > 25º apart recorded at 15 frames per second were used for the threedimensional reconstruction of the target non-IRA. The diameter stenosis, area stenosis, minimal luminal area, maximal, minimal and reference vessel diameters were estimated. The QFR values were obtained by applying computational principles of fluid dynamics to the aforementioned software. The modeled virtual hyperemic flow velocity derived from contrast flow (contrast QFR, cQFR) without adenosine was implemented. Two independent certified software users blinded to the visual assessment of the severity of stenosis and the QFR value obtained during the first or staged procedure, respectively, conducted the offline assessment in a core laboratory14. The inter- and intra-observer variability were examined in 20 lesions through repeated measurements conducted by both certified software users (10 lesions to determine the intra-observer variability and 10 lesions to asses the interobserver variability).
Finally, the correlation between the FFR and the QFR values was estimated in the prospective group of patients during the index or staged procedures. The FFR measurements were performed using the Aeris device (St. Jude Medical, St. Paul, MN, United States). Maximal hyperemia was induced through the continuous IV infusion of adenosine (140-μg/kg/min) that was maintained for 2 minutes or until symptom onset. The QFR analysis was conducted in a blind fashion with respect to the FFR values. Values ≤ 0.8 were considered significant stenosis for both the QFR and the FFR.
Statistical analysis
The qualitative variables are expressed as absolute frequencies and percentages. The quantitative ones as mean ± standard deviation. The normal distribution of the quantitative variables was determined using the Kolmogorov-Smirnov test and Q-Q plots. Data were analyzed on a per-patient basis for the clinical characteristics and on a per-vessel basis for the quantitative coronary angiography and QFR values. The agreement between the FFR and the QFR was determined using the Bland-Altman plot method and the intraclass correlation coefficient. The paired sample t-test was used to determine the evolution of measurements between the index and the staged procedures. The receiver operating characteristic curve was analyzed to assess the capacity of the QFR at the index procedure to predict the QFR at the staged procedure. Finally, both the intra- and inter-observer variability were determined using the intraclass correlation coefficient for these measurements with repeated analysis 1-month apart in 20% of the lesions. All analyses were conducted using the statistical package SPSS, version 24.0 (Armonk, NY: IBM Corp) and R 3.4.3.
Results
Study population
A total of 828 patients were admitted or transferred to our department with suspected STEMI between January 2016 and December 2017. The diagnosis was confirmed in 455 patients of which 196 (43.1%) showed multivessel disease. Among them, 31 patients (15.8%) underwent complete revascularization during the index procedure and in 165 patients (84.2%) the operation on the nonculprit lesions was postponed or never conducted. Finally, 46 patients with multivessel disease and staged procedure were excluded due to suboptimal angiographic images precluding an adequate QFR analysis during the primary (13 patients) or staged (33 patients) procedure. The study population included 88 patients with a total of 131 lesions in nonculprit arteries. The main characteristics of the overall population are shown on table 1. Most patients were males (86.4%) with inferior or anterior STEMI in 57.9% and 37.5%, respectively, and admitted due to primary PCI in 64.8% of the cases. The culprit artery Thrombolysis in Myocardial Infarction flow grade was 0-1 in 51.1%, and 4.5% were in shock. The left anterior descending artery was the most common non-IRA (50%). Following the index procedure, the staged revascularization of 1 (56.8%), 2 (38.7%), or more arteries (4.5%) was performed during the hospital stay for an average 5 days [interquartile range, 2-6]. Successful revascularization of the IRA and complete revascularization were achieved in 100% and 76% of the patients, respectively.
Table 1. Baseline characteristics of patients admitted due to ST-segment elevation myocardial infarction
| Variables | Retrospective sample N = 88 | Prospective sample N = 12 |
|---|---|---|
| Baseline characteristics | ||
| Age (y) | 67.8 ± 11.2 | 70.1 ± 9.3 |
| Gender (male) (%) | 86.4 | 75 |
| Hypertension (%) | 45.5 | 66.7 |
| Dyslipidemia (%) | 36.4 | 33.3 |
| Height (cm) | 167.8 ± 8.2 | 164.9 ± 7.8 |
| Weight (kg) | 79.5 ± 10.6 | 78.3 ± 8.9 |
| Obesity (%) | 29.5 | 33.3 |
| Chronic kidney disease (%) | 3.4 | 0 |
| STEMI main features | ||
| AMI Killip I (%) | 85.2 | 100.0 |
| AMI Killip II (%) | 10.4 | 0 |
| AMI Killip III (%) | 0 | 0 |
| AMI Killip IV (%) | 4.5 | 0 |
| Radial access (%) | 95.3 | 83.3 |
| Primary PCI (%) | 64.8 | 100.0 |
| Post thrombolysis routine PCI (%) | 25 | 0 |
| Rescue PCI (%) | 10.2 | 0 |
| IRA LAD (%) | 40.9 | 50.0 |
| IRA RCA (%) | 47.8 | 16.7 |
| IRA Cx (%) | 11.3 | 33.3 |
| TIMI grade-0 flow IRA (%) | 44.3 | 41.7 |
| TIMI grade-1 flow IRA (%) | 6.8 | 25.0 |
| TIMI grade-2 flow IRA (%) | 3.4 | 0.0 |
| TIMI grade-3 flow IRA (%) | 45.5 | 33.3 |
| Time to staged procedure (d) | 5.8 ± 3.6 | N/A |
|
Data are expressed as no. (%) or mean ± standard deviation. AMI, acute myocardial infarction; Cx, circumflex artery; IRA, infarct related artery; LAD, left anterior descending; PCI, percutaneous coronary intervention; RCA, right coronary artery; STEMI, ST-segment elevation myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction. |
||
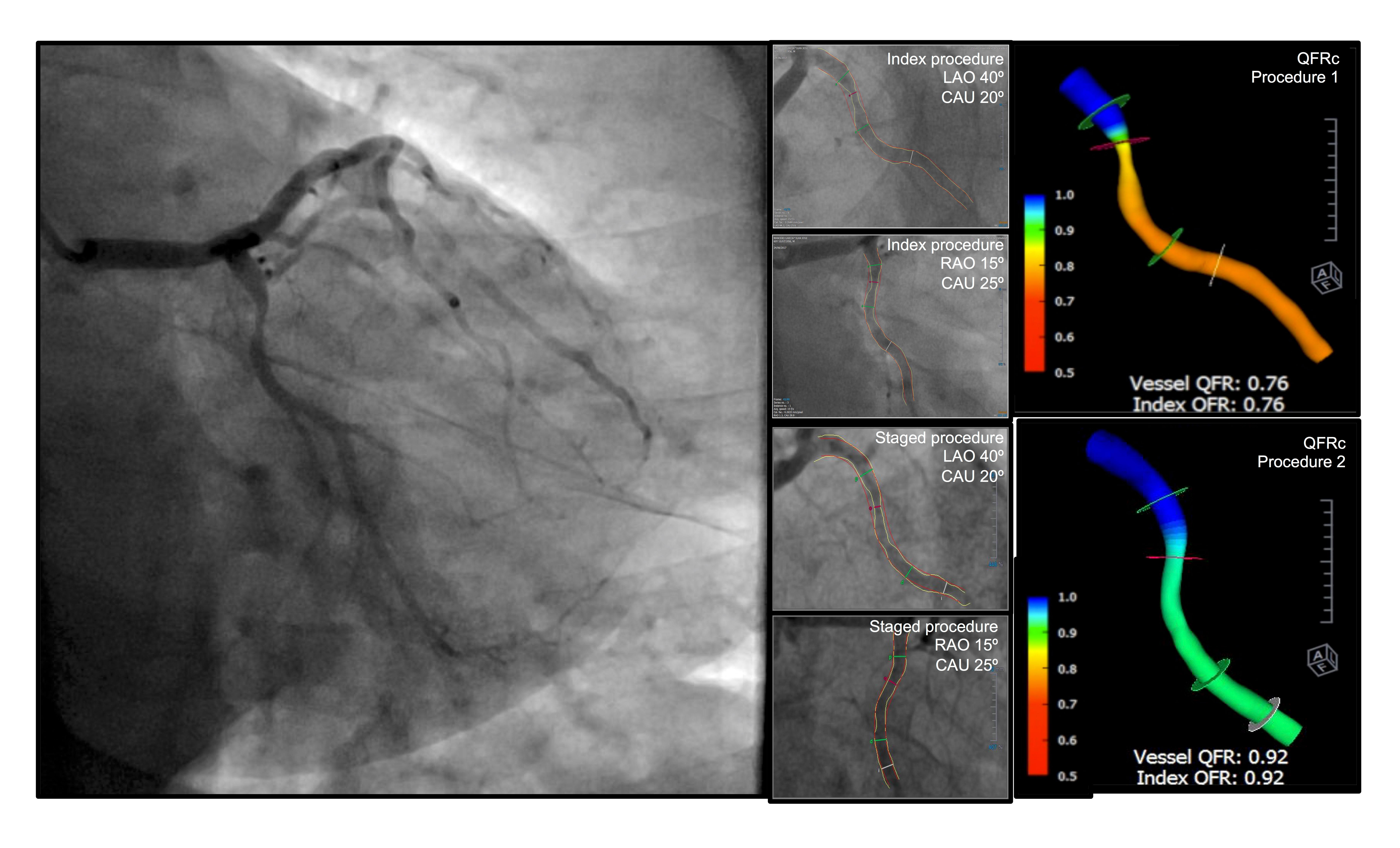
Validation of QFR assessment in nonculprit lesions
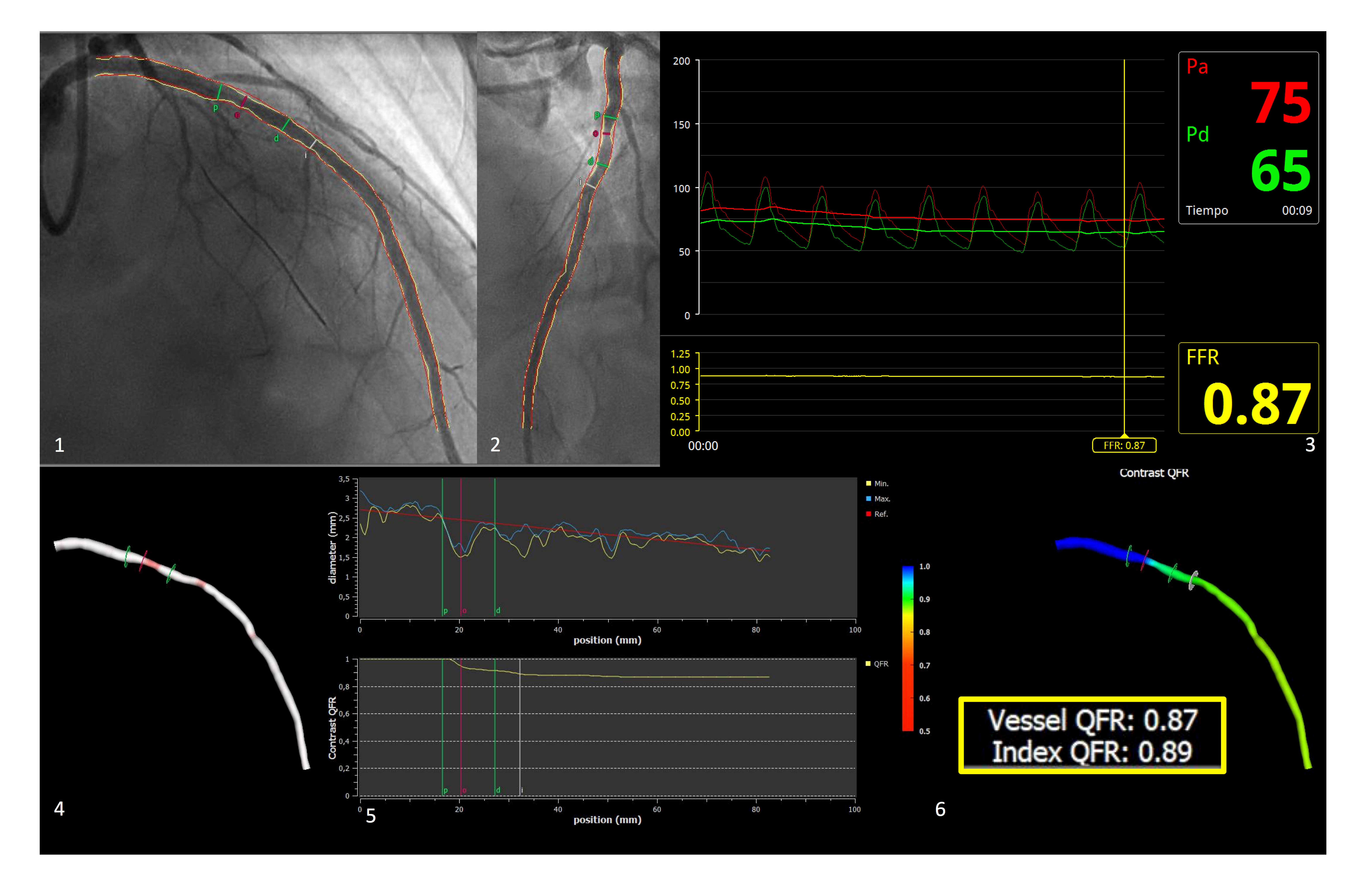
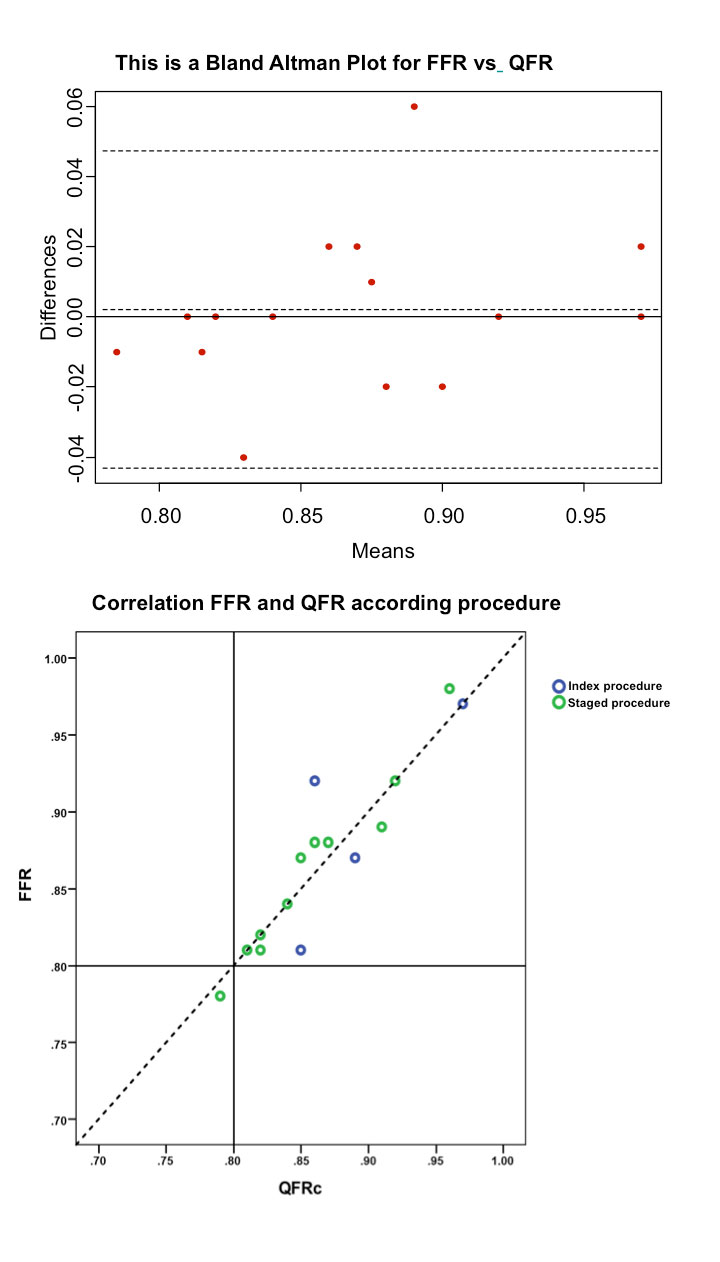
The prospective assessment of the correlation between the QFR and the FFR was conducted in 12 patients (15 lesions) of the study population following the protocol described elsewhere11. The main characteristics of this validation sample were similar to those of the QFR cohort as shown on table 1. No complications followed the use of pressure wires. The mean FFR value was 0.87 ± 0.06 and the mean difference compared to the QFR was0.017 ± 0.02. One paradigmatic example of a lesion assessed through FFR and QFR is showed on figure 1. The intraclass correlation coefficient was 0.959 (95% confidence interval, 0.882- 0.986). In 4 lesions (26.7%) the FFR was performed during the first procedure after the revascularization of the culprit lesion. No difference was found on the diagnostic accuracy of the QFR between the first and the staged procedures in this sample (relative mean difference 0.0346 ± 0.29 and 0.114 ± 0.10, P = .214); The Bland Altman plot used to see the degree of agreement between these measures and the correlation according to the procedure is shown on figure 2.
Figure 1. Representative example of agreement between the FFR and the QFR in non-IRA lesion. A: RAO, 30º; CRA, 30º; B: LAO, 40º; CRA, 20º; C: FFR; D: 3D angiographic reconstruction; E: lumen diameter and QFR pullback; F: QFR value. CRA, cranial; FFR, fractional flow reserve; IRA, infarct related artery; LAO, left anterior oblique; QFR, quantitative flow ratio; RAO, right anterior oblique.
Figure 2. Correlation and agreement between the QFR and the FFR in non-IRA stenosis based on index or staged procedure. FFR, fractional flow reserve; QFR, quantitative flow ratio.
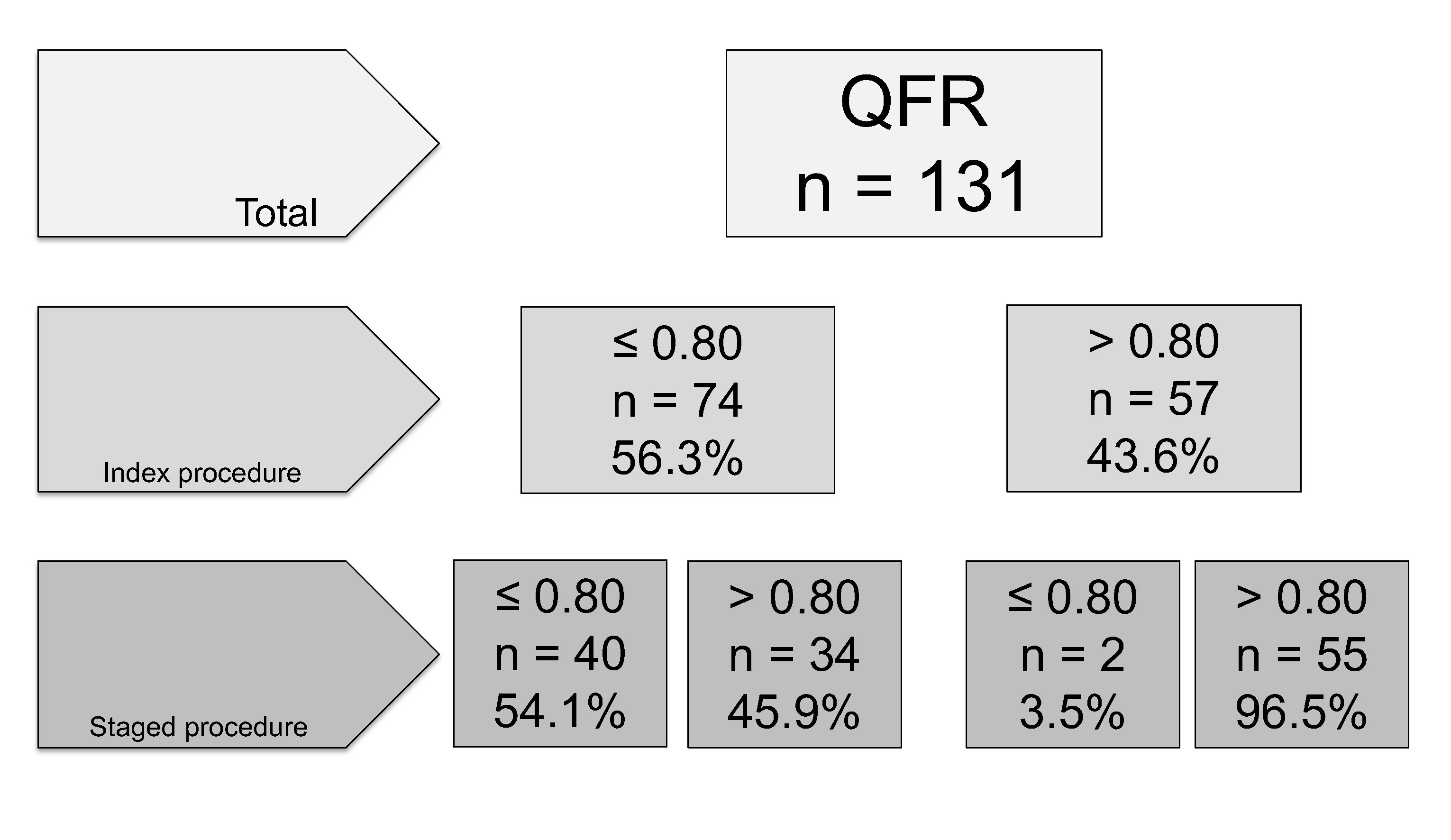
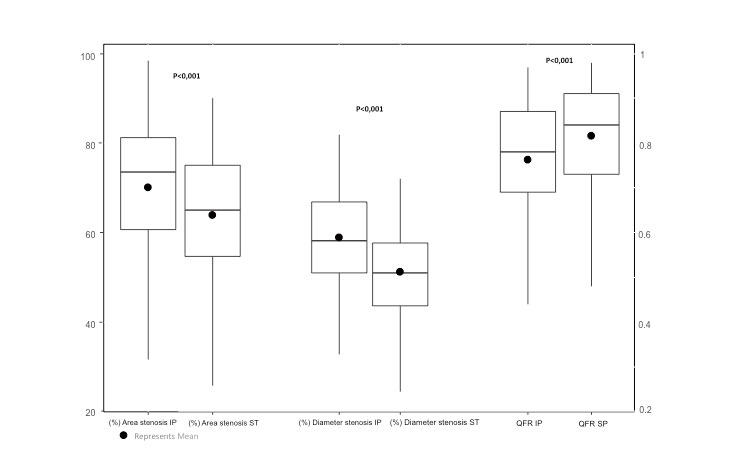
QFR changes across index and staged procedures
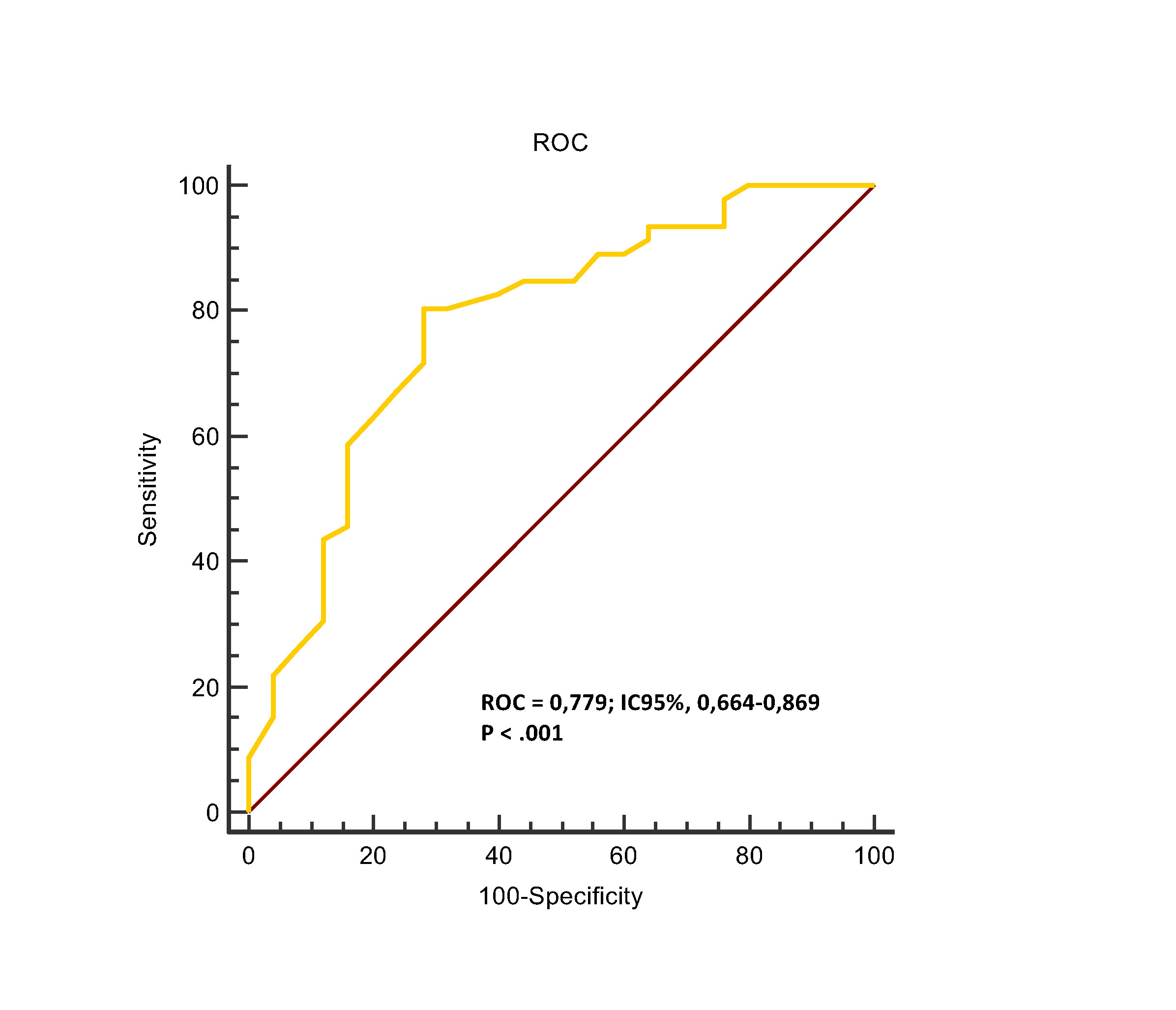
One hundred and twenty-two (93.1%) of the 131 lesions in non- culprit vessels were considered eligible for scheduled percutaneous revascularizations according to the angiography visual assessment. Among them, only 56.3% showed QFR values ≤ 0.80 in the index procedure when assessed retrospectively(figure 3). A statistically nonsignificant decrease of the QFR values was confirmed between the index and the staged procedure in patients with initial QFR values > 0.80; however, 2 patients with initial nonsignificant QFR values showed a drop < 0.80 in the staged angiography assess-ment. All patients with initial values > 0.82 showed non-significant stenosis in the second procedure. On the other hand, 45.9% of the lesions with significant QFR values were considered non-significant when assessed during the second procedure, with larger mean diame-ters and stenotic areas (P < .001 for both) as shown on table 2. The main changes seen between both proceedures are shown on figure 4 and one paradigmatic example is shown on figure 5. The sensitivity and specificity of QFRs > 0.82 during the index procedure to predict significant stenosis (QFR < 0.80) during the staged procedure were 84% and 58.7%, respectively, with a positive predictive value of 52.5% and a neg-ative predictive value of 87% (figure 6). The therapeutic strategy was implemented regardless of the findings from the QFR assess-ment since it was estimated retrospectively. This allowed us to compare the strategy based on the angiography visual assessment interpretation and posterior QRF findings leading to a total of 46 lesions treated with stents despite showing nonsignificant QFRs.
Figure 3. QFR changes across index and staged procedures in patients with angiography-confirmed significant stenosis in nonculprit vessels. QFR, quantitative flow ratio.
Table 2. Quantitative coronary angiography measures and quantitative flow ratio analysis according to procedure .
| Total: 131 no-ARI | Procedimiento índice | Segundo procedimiento | p* |
| Diámetro de estenosis (%) | 58,9 ± 12,0 | 51,15 ± 10,6 | < 0,001 |
| Área estenótica (%) | 70,1 ± 15,1 | 63,9 ± 15,1 | < 0,001 |
| Diámetro máximo del vaso proximal (mm) | 2,7 ± 0,6 | 2,8 ± 0,6 | 0,182 |
| Diámetro mínimo del vaso proximal (mm) | 2,4 ± 0,5 | 2,5 ± 0,6 | 0,231 |
| Diámetro máximo del vaso distal (mm) | 2,6 ± 0,7 | 2,6 ± 0,6 | 0,850 |
| Diámetro mínimo del vaso distal (mm) | 2,3 ± 0,6 | 2,3 ± 0,5 | 0,751 |
| Diámetro del vaso de referencia (mm) | 2,5 ± 0,7 | 2,5 ± 0,6 | 0,295 |
| Diámetro luminal mínimo (mm) | 1,0 ± 0,3 | 1,2 ± 0,4 | < 0,001 |
| Ratio de flujo cuantitativo | 0,76 ± 0,14 | 0,82 ± 0,12 | < 0,001 |
|
ARI: arteria responsable del infarto. |
|||
Figure 4. QFR changes in nonculprit lesions across index and staged procedures in patients with angiography-confirmed significant stenosis. IP, index procedure; QFR, quantitative flow ratio; ST, staged procedure.
Figure 5. Changes in QFR value for the circumflex artery during index and staged procedures in one patient with inferior STEMI due to right coronary artery occlusion. QFR, quantitative flow ratio; STEMI, ST-segment elevation myocardial infarction.
Figure 6. ROC curve analysis showing the sensitivity and specificity of QFR > 0.82 during the index procedure to predict significant stenosis during the staged procedure based on repeated QFR measurements. 95%CI, 95% confidence interval; QFR, quantitative flow ratio; ROC, receiver operating characteristic.
Intra- and inter-observer variability
Also, the optimal intra- and interobserver variability for measur-ing the QFR were confirmed by intraclass correlation coefficients of 0.958 (95% confidence interval, 0.877-0.984) and 0.991 (95% confidence interval, 0.960-0.997), respectively.
Discussion
It is well known that the visual assessment of coronary stenosis usually overestimates its severity5, but operators are often reluc-tant to conduct functional assessments of nonculprit lesions inthis context due to potential risks associated with the FFR and the altered physiology of this condition. The QFR value for the assessment of nonculprit lesions in STEMI patients was already investigated in a small pilot study8 and offers potential advantages mainly based on its quick application and no need for wiring coronary arteries or administering adenosine. The main findings of our study are: a) The QFR has a good correlation with both the FFR and the optimal intra- and inter-observer variability in trained operators in the assessment of functional severity in coronary lesions, suggestive that this may be an excellent tool also in STEMis; b) The severity of stenosis in nonculprit lesions is higher in the acute phase of STEMis, which is mainly confirmed by the angiography but also by the QFR; c) The functional assessment of nonculprit lesions through the QFR may be useful in the acute phase of STEMis. On the one hand, stenoses with QFR values > 0.82 remained nonsignificant in the follow-up in all cases, which may lead to avoiding staged procedures and stenting in up to 1/3 of these patients; on the other hand, significant QFR values during the index procedure should not lead to treating the lesion in the same intervention since, according to the QFR, 45.9% of significant lesions became nonsignificant during the staged assessment.
Differences in anatomical and physiological assessments
The growing evidence that places physiology above anatomy in the field of coronary disease deserves its own research when it comes to STEMI patients in order to reduce the rates of overtreatment. Overestimation when decisions are made based on angiographies5 and underestimation when based on FFR have been reported in this context6. In the COMPARE-ACUTE trial, the physiological assessment of non-IRA was conducted during the index procedure and showed that only half of the lesions angiographically considered significant were confirmed through the FFR3. On the contrary, in the DANAMI-3-PRIMULTI trial, the assessment of nonculprit lesions was conducted during staged procedures rising the percentage of lesions with FFR < 0.80 to almost 70%4. The changes in the macrovascular tone or the obstruction of microvascular flow during the acute phase of myocardial infarctions may partially explain these findings in large trials. This difference when estimating severity between both procedures both through quantitative coronary angiography and QFR should be taken into consideration to avoid treating non-IRA lesions during primary PCIs. This is especially important even when only the angiographic assess-ment is taken into account since the need for complete revascu-larization is under discussion and still not recommended by the actual guidelines.
Potential new contributions of QFR in STEMI patients
The QFR can be safely conducted during primary percutaneous coronary interventions. A cut-off value of 0.82 helped to identify the patients who were not eligible for sequential revascularization. The QFR assessment in the staged procedure showed no significant differences compared to the acute phase probably due to the limited sample size. However, a trend towards higher QFR values in the staged procedure–similar to that of FFR–was ob-served. This may be explained by the presence of microvascular dysfunction in the acute phase12, though the quality of coronary angiography may have had an influence here. Nevertheless, the potential of QFR in non-IRAs to identify lesions that should not be treated and, therefore, avoid unnecessary staged procedures is very interesting. From this perspective, the QFR may be that long-awaited tool to help determine what the best strategy is when making the complex decision of treating multivessel disease in STEMI patients. Ongoing studies that are putting this hypothesis to the test while assessing the need for urgent revascularization during follow-up with this new strategy will determine the clini-cal relevance of QFR.
Limitations
The main limitations of this study are its retrospective nature and limited sample size. The QFR assessment requires good quality from the angiographic assessment and, although a standard protocol was routinely performed for coronary angiographies, several studies had to be excluded due to their inadequate quality, which may be a bias that should be analyzed by future prospective studies. Also, the limited sample size may have associated limited power in the diagnostic accuracy of the QFR in certain subgroups of patients and in terms of validating the QFR compared to the FFR.
Conclusions
In sum, coronary functional assessments based on the QFR of non-culprit lesions after an acute myocardial infarction showed a high percentage of angiographic overestimation in the severity of stenoses (> 40%). QFRs > 0.82 during the index procedure accurately identified those nonculprit lesions that are no flow-limiting and nonculprit lesions and QFR values below this threshold triggered re-assessments before recommending the angioplasty procedure. The prospective validation of this hypothesis is totally justified.
Funding
This project, code: GRS1728/A/18, has been financed by the Gerencia Regional de Salud de la Junta de Castilla y León, Spain.
Conflicts of interests
There is no conflict of interest to declare.
Whait is known about the topic?
- Over half of the patients admitted due to STEMI show multivessel disease, which is why complete revascularization is recommended.
- The functional assessment of nonculprit lesions after STEMI has proven useful when establishing the revascularization strategy to be followed; how-ever, most interventional cardiologists base their decision on the angiography because of the challen-ges and limitations of FFR in this context.
- The QFR is a new functional index based on the three-dimensional reconstruction of the coronary anatomy and computational fluid dynamics while keeping a good correlation with the FFR and without having to wire the coronary arteries.
What does this study add?
- Good degree of agreement between the QFR and the FFR confirmed for nonculprit lesions in STEMI patients.
- The QFR values in the acute phase of STEMI suggested greater severity compared to deferred assessments. QFR thresholds = 0.82 in the acute phase better identified patients threshold who may not need deferred procedures for new functional assessments or angioplasties in nonculprit lesions, thus reducing risks and unnecessary costs.
References
1. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177.
2. Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: The CvLPRIT trial. J Am Coll Cardiol. 2015;65:963-972.
3. Smits PC, Abdel-Wahab M, Neumann FJ, et al. Fractional Flow Reserve–Guided Multivessel Angioplasty in Myocardial Infarction. N Engl J Med. 2017;376:1234-1244.
4. Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015;386:665-671.
5. Hanratty CG, Koyama Y, Rasmussen HH, et al. Exaggeration of Nonculprit Stenosis Severity During Acute Myocardial Infarction: Implications for Immediate Multivessel Revascularization. J Am Coll Cardiol. 2002;40:911-916.
6. Cuculi F, Maria L de, Meier P, et al. Impact of Microvascular Obstruction on the Assessment of Coronary Flow Reserve, Index of Microcirculatory Resistance, and Fractional Flow Reserve After ST-Segment Elevation Myocardial Infarction. J Am Coll Cardiol. 2014;64:1894-1904.
7. Toth GG, Toth B, Johnson NP, et al. Revascularization decisions in patients with stable angina and intermediate lesions: Results of the international survey on interventional strategy. Circ Cardiovasc Interv. 2014;7:751-759.
8. Tu S, Westra J, Yang J, et al. Diagnostic Accuracy of Fast Computational Approaches to Derive Fractional Flow Reserve From Diagnostic Coronary Angiography. JACC Cardiovasc Interv. 2016;9:2024-2035.
9. Yazaki K, Otsuka M, Kataoka S, et al. Applicability of 3-Dimensional Quantitative Coronary Angiography-Derived Computed Fractional Flow Reserve for Intermediate Coronary Stenosis. Circ J. 2017;81:988-992.
10. Westra J, Tu S, Nissen L, et al. Evaluation of Coronary Artery Stenosis by Quantitative Flow Ratio During Invasive Coronary Angiography. Circ Cardiovasc Imaing. 2018;11:1-8.
11. Spitaleri G, Tebaldi M, Biscaglia S, et al. Quantitative Flow Ratio Identifies Nonculprit Coronary Lesions Requiring Revascularization in Patients With ST-Segment-Elevation Myocardial Infarction and Multivessel Disease. Circ Cardiovasc Interv. 2018;11:e006023.
12. Mejía-Rentería H, Lee JM, Lauri F, et al. Influence of Microcirculatory Dysfunction on Angiography-Based Functional Assessment of Coronary Stenoses. JACC Cardiovasc Interv. 2018;11:741-753.
13. Tu S, Barbato E, Yang J, Li Y, Rusinaru D, Reiber JHC. Fractional Flow Reserve Calculation From 3-Dimensional Quantitative Coronary Angiography and TIMI Frame Count. JACC Cardiovasc Interv. 2014;7:768-777.
14. Instituto de Ciencias del Corazón. Disponible en: http://icicorelab.es. Consultado 14 Jul 2018.
E-mail address: ijamat@gmail.com (I.J. Amat-Santos).