ABSTRACT
Introduction and objectives: There are few data on the utility of drug-coated balloons (DCB) for the side branch treatment of bifurcated lesions. Our objective was to determine the long-term effectiveness of such device in this scenario.
Methods: Retrospective-prospective registry of all such lesions treated with DCB (paclitaxel coating) at our unit from 2018 until present day with clinical follow-up including a record of adverse events.
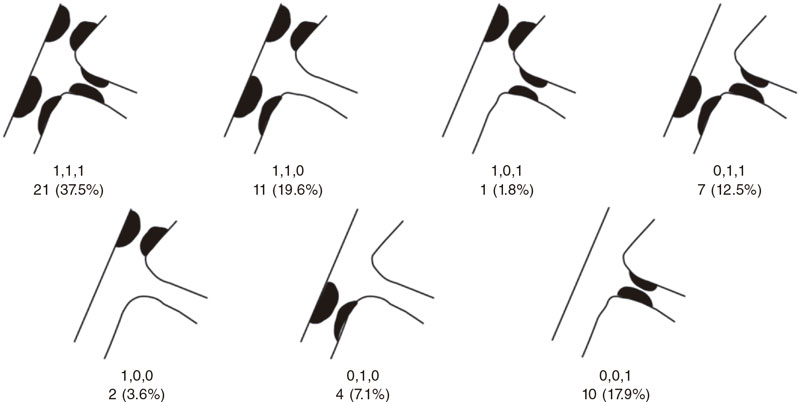
Results: A total of 56 lesions from 55 patients were included. The main demographic characteristics were mean age, 66.2 ± 11.3; and/or women, 27.3%; hypertension, 67.3%; dyslipidemia, 83.6%, and diabetes, 32.7%. The most common causes according to the coronary angiography were non-ST segment elevation acute coronary syndrome and stable angina. The main characteristics of the lesions were the location (circumflex-obtuse marginal, 19.6%; left anterior descending-diagonal, 64.3%; left main-circumflex, 8.9%; posterior descending-posterolateral trunk, 7.1%. The Medina classification was 1-1-1 37.5% of the times, and 1-1-0, 19.6% of the times. The rate of in-stent restenotic lesions was 32.1%. Procedural characteristics: radial access, 100%; side branch (SB) and main branch (MB) predilatation, 83.9% and 58.9%, respectively; MB stenting, 71.4%; POT technique, 35.7%; final kissing, 48.2%; optical coherence tomography/intravascular ultrasound, 7.1%. Procedural success was achieved in 98.2% of the cases. The median follow-up he all-cause mortality, myocardial infarction and lesion thrombosis, and target lesion revascularization rates were .7%, 0%, and 3.6%, respectively.
Conclusions: SB treatment with DCB in selected bifurcation lesions is safe and highly effective with a long-term success rate of 96.4%. Very large studies are still required to compare this strategy to SB conservative approach, and determine its optimal treatment.
Keywords: Drug-coated balloon. Bifurcation lesions. Follow-up study. Side branch.
RESUMEN
Introducción y objetivos: Hay pocos datos acerca de la utilidad del balón farmacoactivo (BFA) para el tratamiento de la rama lateral de las lesiones en bifurcación. El objetivo fue determinar la efectividad a largo plazo de dicho dispositivo en este escenario.
Métodos: Registro retrospectivo-prospectivo de todas las lesiones de este tipo tratadas con BFA recubierto de paclitaxel en nuestra unidad desde 2018 hasta la actualidad. Se realizó un seguimiento clínico con registro de eventos adversos.
Resultados: Se incluyeron 56 lesiones de 55 pacientes. Principales características demográficas: edad media 66,2 ± 11,3 años, 27,3% mujeres, 67,3% hipertensión arterial, 83,6% dislipemia y 32,7% diabetes. Las indicaciones más frecuentes para el cateterismo fueron síndrome coronario agudo sin elevación del ST y angina estable. Características de las lesiones tratadas: localización circunfleja-obtusa marginal 19,6%, descendente anterior-diagonal 64,3%, tronco común-circunfleja 8,9% y descendente posterior-tronco posterolateral 7,1%. Según la clasificación de Medina, el tipo más frecuente fue el 1,1,1 con el 37,3%, seguido del 1,1,0 con el 19,6%. Las lesiones tipo reestenosis en el interior del stent fueron del 32,1%. Características principales del procedimiento: acceso radial 100%, predilatación de rama lateral 83,9% y de rama principal 58,9%, stent en rama principal 71,4%, técnica POT 35,7%, kissing final 48,2% y tomografía de coherencia óptica/ecocardiografía intravascular 7,1%. Se logró el éxito del procedimiento en el 98,2%. Con un seguimiento medio de 12 meses, se registraron una incidencia de muerte por cualquier causa del 3,7%, trombosis lesional o infarto 0%, y revascularización de la lesión diana del 3,6%.
Conclusiones: El tratamiento con BFA de la rama lateral en lesiones bifurcadas seleccionadas es seguro y presenta una alta efectividad, con una tasa de éxito a largo plazo del 96,4%. Serían necesarios estudios muy amplios que permitieran comparar dicha estrategia con el abordaje conservador de la rama lateral y determinar cuál es su tratamiento óptimo.
Palabras clave: Balón farmacoactivo. Lesiones en bifurcación. Estudio de seguimiento. Rama lateral.
Abbreviations DCB: drug-coated balloon. ISR: in-stent restenosis. MB: main branch. SB: side branch.
INTRODUCTION
Coronary bifurcation lesions are still challenging for interventional cardiologists. The complexity surrounding such lesions regarding their anatomical, functional, and even clinical aspects truly complicates the management of this entity despite its high incidence rate that can be up to 20% of all the lesions that are treated at a cath lab on a routine basis. The relentless publication of articles on such lesions over the last few decades, the creation of specific study groups like the European Bifurcation Club, and the periodic publication of consensus documents for the management of this entity shows, without a doubt, that this scenario is in constant change and has not been solved today yet. One of the most controversial aspects is the importance of the side branch (SB) regarding the long-term prognosis of such lesions. Drug-coated balloon (DCB) is part of the therapeutic armamentarium of interventional cardiologists to treat coronary bifurcation lesions. Its utility for the management of certain anatomical settings like in-stent restenosis (ISR) type of lesions has already been demonstrated. However, its effectiveness to treat the SB is much less evident with scarce studies available in the medical literature. The theoretical advances posed by this device to treat the SB would be the administration of antiproliferative drugs into the ostium mainly, the lack of distortion of its original anatomy, and the minimization of strut deformation at carina level.1
This article presents a registry with the results obtained in our unit with the management of SB with DCB with a longer than usual clinical follow-up in this type of studies.
METHODS
This was a single-center, prospective-retrospective registry started back in 2019 of all coronary bifurcation lesions where the SB was treated with paclitaxel-coated DCB from October 2018 through March 2022. The device used was the SeQuent Please NEO (Braun, Germany), a paclitaxel-iopromide coated polymer-free balloon using Paccocath technology. Inclusion criteria were the presence of coronary bifurcation lesions with 1 compromised SB of, at least, 2 mm in diameter through visual angiographic estimate regardless of the aprioristic presence of a diseased SB or the appearance of carina displacement or slow flow after treating the main branch (MB). Also, the operator should consider the DCB approach of clinical and prognostic interest. Patient recruitment in the registry was on the rise: 4 patients in 2018, another 4 in 2019, 9 patients in 2020, 31 in 2021, and finally 7 within the first 3 months of 2022. No exclusion criteria were established. Approach strategy consisted of an early provisional stenting or DCB technique to treat the MB when damaged. Further management of SB with DCB was left to the operator’s criterion if, after treating the MB, significant damage done to the SB would require stenting in such branch. In that case, the patient would not be included, and the SB would not be eligible for treatment with a DCB. If, after preparing the lesion, the operator would actually consider using the DCB option, that would be the time to include the patient in the study. The rate of procedural failure—defined as the impossibility to cross the lesion with the DCB once it was used or unsatisfactory angiographic outcomes after balloon inflation involving SB stenting. The protocol for using the DCB—based on the recommendations established on the use of such devices—consisted of SB predilatation with non-compliant or scoring balloons in a 0.8-1 vessel/balloon diameter ratio, use of the device if an acceptable angiographic result with TIMI grade-3 flow was achieved, lack of significant dissection, and residual stenosis < 30%. If other lesions different from the one that triggered the inclusion in the registry needed revascularization, this was scheduled for a second surgical act. The study design followed a per protocol analysis to estimate the benefits of the technique described compared to the routine clinical practice including cases with successful DCB treatment at the follow-up and excluding those with acute device failure or impossibility to use the device once opened for being unable to cross the lesion. The lack of dissection after DCB that required stenting with residual stenosis < 50%, and final TIMI grade-3 flow was considered as procedural success. Device failure, on the other hand, was considered as an impossible DCB inflation once used or the need for stenting the SB with unsatisfactory DCB results. Different clinical variables from the patient were analyzed, as well as the lesion anatomy, and the procedural intervention per se. Retrospective clinical follow-up of patients successfully treated with the DCB was conducted. Follow-up went on for a maximum of 2 years after the procedure, and prospectively since the registry started back in 2019 until present time. This follow-up was conducted through phone calls or by checking the patients’ electronic health records. The ARC-2 definitions2 were used to collect the adverse clinical events including a composite endpoint of all-cause mortality, cardiac death, myocardial infarction, device thrombosis, clinically driven target lesion failure and revascularization, target vessel failure outside the target lesion, and revascularization of other lesions occurred at follow-up. All patients signed their written informed consent forms, and the study was approved by our center research ethics committee.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation. Categorical variables are expressed as frequency and percentage. Also, actuarial curves of adverse event-free survival using the Kaplan-Meier method were built, specifically target lesion failure-free and adverse event-free curves (all-cause mortality, target lesion revascularization, target vessel failure, and revascularization of other lesions).
RESULTS
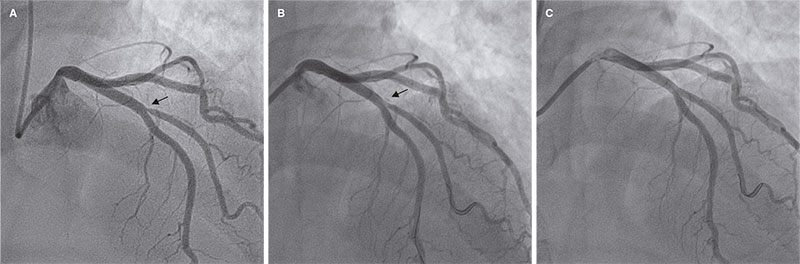
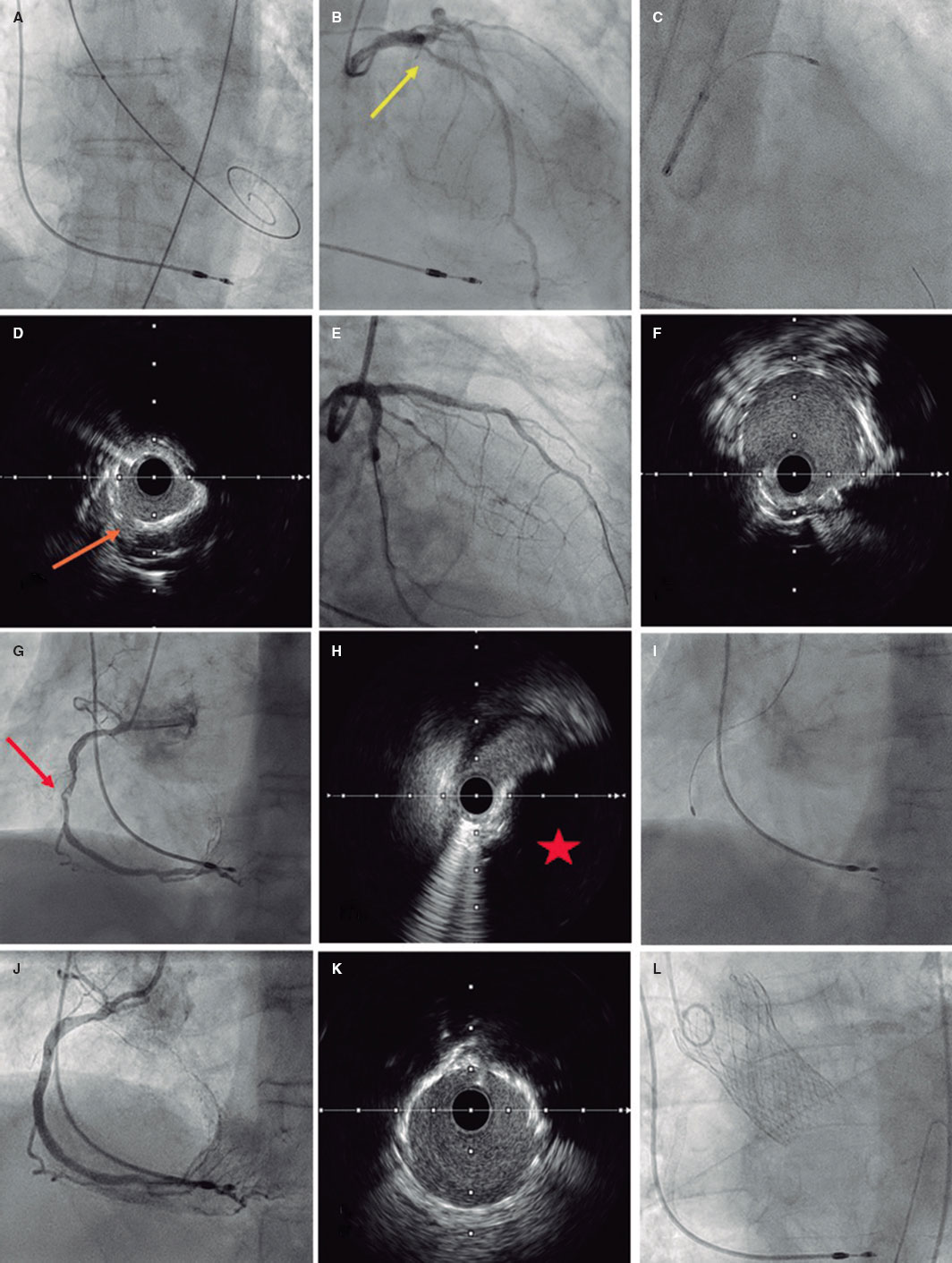
A total of 55 patients and 56 lesions were included since 2 different bifurcations found in 1 of the patients were treated in the same procedure. The patient/lesion flowchart included in the study is shown on figure 1. The patients’ clinical characteristics are shown on table 1. Vascular access was radial in 100% of the cases using a 6-Fr introducer sheath also in all of them. Table 2 shows the anatomical characteristics of target lesions. Figure 2 shows a schematic representation of the type of lesion according to the Medina classification. Table 3 shows the variables associated with the procedure. We should mention that all the clinical and anatomical data shown here, the patients’ high-risk profile with high prevalence of cardiovascular risk factors, and the large number of ISR-type of lesions reached 32.1% of the sample. The rate of lesions included with damage to 2 or 3 different bifurcation segments was 71.4% (40 out of 56). Regarding procedural factors the high rate of procedural success was significant (low rate of acute device failure with only 1 case of a type A dissection image after DCB inflation without damage to the distal flow and > 30% residual stenosis). Therefore, because of lesion location at ostium level, and possible damage to the MB (the left anterior descending coronary artery in this case), the operator decided to perform drug-eluting stent implantation for sealing purposes (figure 3). In all the remaining procedures, the acute result of the DCB was successful. In our series, the scarce use of intracoronary imaging modalities (only 7.1%) was also remarkable.
Figure 1. Flowchart of patients/lesions included in the study.
Figure 2. Number of lesions based on the type of bifurcation damage according to the Medina classification.
Figure 3. Only case of acute device failure. A: diagonal branch ostial lesion prior to the intervention (arrow); B: suboptimal outcome after drug-coated balloon (arrow); C: final outcome after stenting the side branch.
Table 1. Patients’ clinical characteristics
| N | 55 |
| Age | 66.2 ± 11.3 years [range, 45-91] |
| Sex | |
| Men | 40 (72.7%) |
| Women | 15 (27.3%) |
| Hypertension | 37 (67.3%) |
| Dyslipidemia | 46 (83.6%) |
| Smoking | 17 (30.9%) |
| Diabetes | 18 (32.7%) |
| Previous PTA | 28 (50.9%) |
| Previous coronary artery bypass graft | 1 (1.8%) |
| Indication for coronary angiography | |
| NSTEACS | 20 (36.4%) |
| STEACS | 9 (16.4%) |
| Stable angina | 20 (36.4%) |
| Other | 6 (10.9%) |
|
NSTEACS, non-ST-segment elevation acute coronary syndrome; PTA, percutaneous transluminal angioplasty; STEACS, ST-segment elevation acute coronary syndrome. |
|
Table 2. Anatomical characteristics of the lesions
| N | 56 |
| Diseased vessel | |
| LMCA-LCx | 5 (8.9%) |
| LAD-diagonal | 36 (64.3%) |
| LCx-OMA | 11 (19.6%) |
| PDA-PLT | 4 (7.1%) |
| ISR-type of lesion | 18 (32.1%) |
|
ISR, in-stent restenosis; LAD, left anterior descending coronary artery; LCx, left circumflex artery; LMCA, left main coronary artery; OMA, obtuse marginal artery; PDA, posterior descending artery; PLT, posterolateral trunk. |
|
Table 3. Procedural characteristics
| N | 56 |
| Predilatation | |
| SB | 47 (83.9%) |
| MB | 33 (58.9%) |
| MB treatment | |
| Stent | 40 (71.4%) |
| DCB | 4 (7.1%) |
| DCB diameter for the SB (mm) | |
| 2 | 20 (35.7%) |
| 2.25 | 4 (7.1%) |
| 2.5 | 23 (41.1%) |
| 3 | 8 (14.3%) |
| 3.5 | 1 (1.8%) |
| Postdilatation | |
| MB | 36 (64.3%) |
| POT | 20 (35.7%) |
| SB | 17 (30.4%) |
| Final kissing balloon | 27 (48.2%) |
| OCT/IVUS | 4 (7.1%) |
| Procedural success | 55 (98.2%) |
|
DCB, drug-coated balloon; IVUS, intravascular ultrasound; MB, main branch; OCT, optical coherence tomography; POT, proximal optimization technique; SB, side branch. |
|
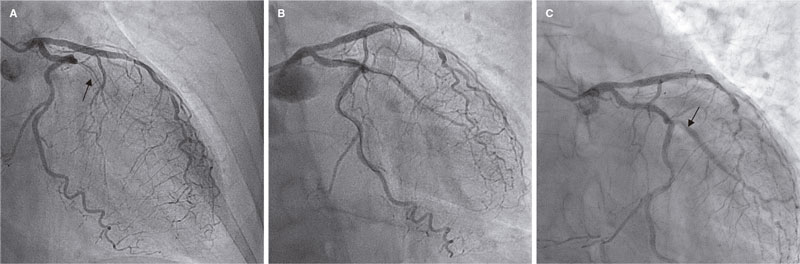
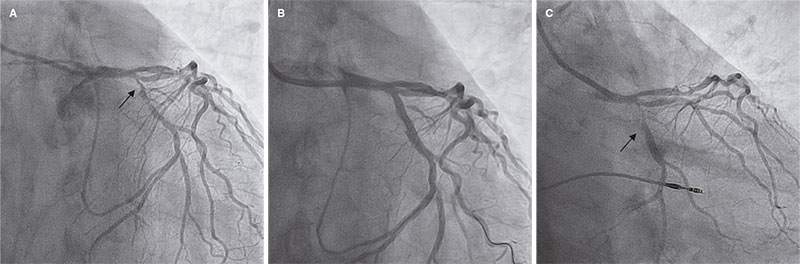
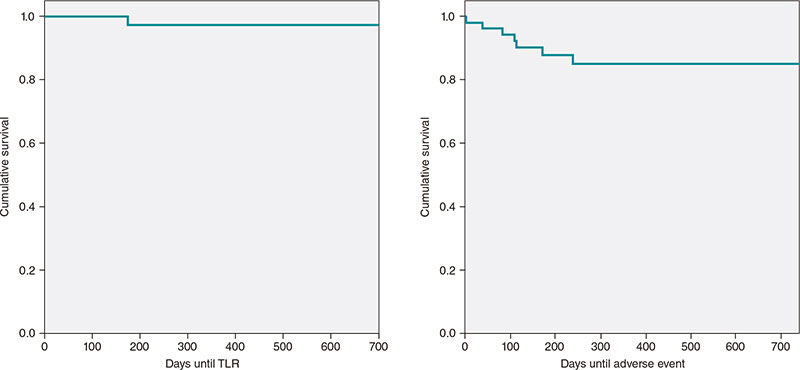
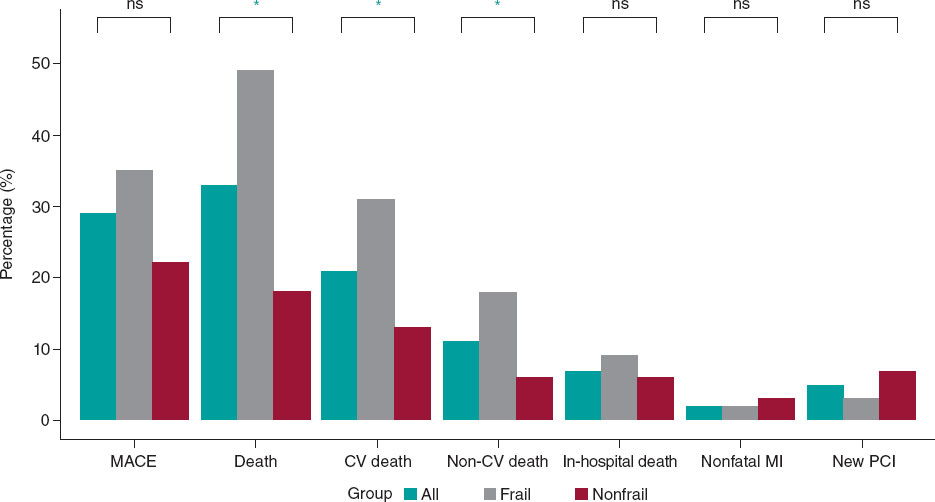
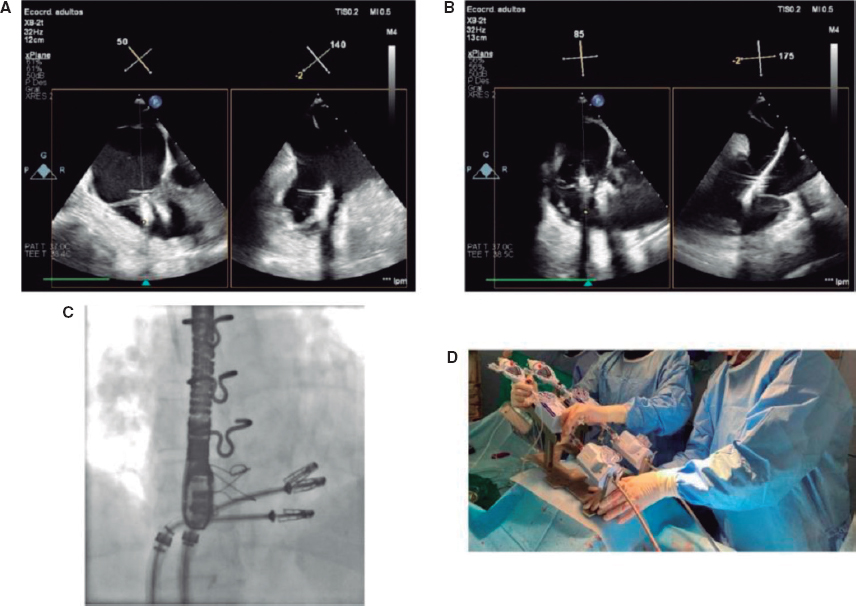
The rate of adverse events at follow-up is shown on table 4. After a median follow-up of 12 months (377 ± 244 days; range, 64-734 days) only 2 clinically driven target lesion revascularizations (3.6%) were reported. Both were performed due to in-stent lesions that did not reach the target lesion proximal or distal borders. The first one was performed in a case of ISR of the SB in a very small vessel without acute ischemia whose new revascularization was performed late, more specifically, 23 months after the index procedure (figure 4). The second one was performed 6 months after the procedure—also without acute ischemic signs—but with ISR in the main vessel while the SB remained patent without significant restenosis (figure 5). Both cases were treated with drug-eluting stent implantation. Two deaths were reported: 1 cardiac death due to advanced left ventricular dysfunction in an 80-year-old woman who, after percutaneous coronary intervention, was implanted with a transfemoral aortic valve and a definitive pacemaker, with poor disease progression that eventually led to her death. The other death was septic shock related. No admissions due to acute myocardial infarction or episodes of target lesion thrombosis (both probable and definitive) were reported. No cases of target vessel failure outside the target lesion were reported either. A total of 5 revascularizations of other lesions (9.3%) were performed—all of them scheduled—but none due to acute coronary syndrome. The Kaplan-Meier curves showing target lesion revascularization-free and adverse event-free survival are shown on figure 6.
Table 4. Rate of adverse cardiovascular events at follow-up
| N | 54/55 |
| Follow-up days | 377 ± 244 [range, 79-734] |
| All-cause mortality | 2/54 (3,7%) |
| Cardiac death | 1/54 (1,8%) |
| Myocardial infarction/target lesion device thrombosis | 0/55 (0%) |
| Target lesion revascularization | 2/55 (3,6%) |
| Target vessel failure outside the target lesion | 0/55 (0%) |
| Revascularization of other lesions outside the target vessel | 5/54 (9.3%) |
Figure 1. First case of target lesion failure due to late restenosis. A: early in-stent restenosis type of lesion in obtuse marginal artery (arrow); B: final outcomes after drug-coated balloon; C: new in-stent restenosis in the side branch at 23 months (arrow).
Figure 5. Second case of target lesion failure. A: early obtuse marginal artery bifurcation lesion with distal left circumflex artery (arrow); B: outcomes after stenting the main branch, and drug-coated balloon implantation into the side branch; C: 6-month follow-up with restenosis at main branch level (arrow).
Figure 6. Kaplan-Meier curve of actuarial target lesion revascularization (TLR)-free survival and composite adverse events-free survival (all-cause mortality, TLR, revascularization of other lesions).
DISCUSSION
The latest document of the European Bifurcation Club on the utility of DCBs to treat SBs in coronary bifurcation lesions pays little attention to it due to the lack of large enough clinical trials to be conclusive.3 Despite the huge amount of medical literature available on the management of coronary bifurcation lesions, the actual significance of the SB and its involvement in target lesion failure has not been properly explained to this date. A study conducted by Oh et al.4 conclude that treating the SB in 1089 patients with bifurcation lesions at left anterior descending coronary artery-diagonal branch level was associated with a lower—yet not statistically significant—rate of target vessel failure. However, this difference was statistically significant when the subgroup studied included low-risk patients. On the other hand, a different clinical trial that studied factors associated with failed revascularizations of the left main coronary artery bifurcation found that the presence of MB stent struts inside the SB ostium was one of them5 suggestive that the use of intracoronary imaging modalities like intracoronary ultrasound or optical coherence tomography could improve results, at least, on such location, by telling us what patients would benefit from specifically treating the SB.
The strongest evidence available to this date leans towards the utility of DCB to treat ISR-type of lesions without a word dedicated to the SB. Very few studies have focused on the effectiveness of DCB to treat the SB. Such document advocates for treating coronary bifurcation lesions with the provisional stenting strategy according to the latest clinical practice guidelines drafted by the European Cardiology Society followed by treating the SB with a DCB. The first clinical trials on this regard were published back in 2011 like the DEBIUT,6 BABILON,7 DEBSIDE,8 the study conducted by Herrador et al.,9 the PEPCAD V,10 and the PEPCAD-BIF11 clinical trials. These studies showed contradictory—yet overall satisfactory—data regarding the effectiveness of DCB. These studies presented better quantitative angiographic parameters regarding restenosis or late lumen loss. However, not in every one of them this was associated with a lower rate of revascularization. As a matter of fact, there were doubts around the possibility of a higher rate of late thrombosis suggested by some of these trials. The recently published BEYOND clinical trial conducted by Jing et al.12 compared the use of a conventional balloon vs DCB to treat the SB with a 9-month angiographic follow-up. This trial found that the DCB was associated with better results regarding less late lumen loss. However, such an improvement did not translate into a lower rate of clinical adverse events since surprisingly enough no new revascularizations were reported in any of the 2 groups. A recent meta-analysis13 that included 10 studies on the effect of DCB on the SB concluded that such technique improved the angiographic outcomes significantly. However, this did not translate either into statistically significant clinical outcomes (target lesion failure mainly) basically due, according to the authors, to the low rate of this adverse event reported, and the fact that the study was statistically underpowered due to its small sample size. In a different study published in 2022,14 the management of coronary bifurcation lesions of left main coronary artery using 2 strategies was compared: double stenting for the MB and the SB vs 1 stent into the MB, and 1 DCB into the SB. They found controversial results at follow-up between both groups in different angiographic parameters with similar rates of restenosis and adverse events. However, the group treated with DCB significantly improved all the parameters associated with the SB (left circumflex artery, in this study)—as opposed to those associated with the MB (left main coronary artery-left anterior descending coronary artery)—with less late lumen loss (0.43 vs -0.17; P < .001), less luminal narrowing (16.7 vs 32.1; P = .002), and greater minimal lumen diameter (2.4 vs 1.8; P = .0031). Still, the rate of restenosis in the left circumflex artery (SB in this study) was 4 times higher in the double stenting group compared to the DCB group (30.4% vs 7.7%) although this difference was not statistically significant (P = .09). This could be indicative of greater superiority of the DCB if studies with larger samples would be conducted. Another recent study published in 202115 randomized 219 true de novo coronary bifurcation lesions where the SB was treated with conventional balloon vs DCB. At 12-month clinical and angiographic follow-up, significant improvements were reported in both the angiographic (less late lumen loss and greater minimal lumen diameter) and clinical parameters with a lower rate of major adverse cardiovascular events being reported. This improvement, however, did not translate into significant reductions regarding new revascularizations or target vessel failure.
The rate of target lesion failure requiring new revascularization was 3.6%, a figure that is consistent with most former studies. However, the range found goes from a surprising 0% up to a whopping 22%. However, we should mention the truly unfavorable clinical and anatomical profile of our sample since in most clinical trials, ISR-type of lesions, left main coronary artery disease or ST-segment elevation acute coronary syndrome—all allowed in our registry—were considered exclusion criteria regarding.
Out of the only 2 cases reported of target lesion failure requiring new revascularization, 1 occurred in a patient with an ISR-type of lesion. This occurred precisely in the SB while in former studies7—as already explained—the main incidence rate of failure occurred in the MB, not in the SB. The exclusion of patients with ISR would account for this difference. In our sample this type of lesions were 32.7% of all the lesions included. This added to the high rate (30.6%) of Medina 1,1,1 coronary bifurcation lesions (the one with the greatest complexity of all bifurcations) demonstrates the truly unfavorable profile of our sample. As a matter of fact, the rate of lesions included with damage to, at least, 2 segments of 1 bifurcation according to the Medina classification reached 71.4%. Very few studies have been conducted on this subgroup of patients. One of the most significant ones is the one conducted by Harada et al.16 that included 177 patients with ISR-type of lesions both in the MB and the SB treated with DCB. The latter was used in 80.6% of the SBs. The rate of binary restenosis was 24% at 6-to-8-month angiographic follow-up while the 1-year rate of new target lesion revascularization was 22%.
Limitations
Our study main limitation is the lack of a control group with lesions of similar characteristics, which would have allowed us to compare both groups and determine exactly the impact DCB has on the prognosis of patients. Similarly, the lack of angiographic follow-up does not discard the possibility of device failure. However, this would probably occur in the SB, not the MB, since it is in the latter where target lesion failure occurs according to the BABILON clinical trial.7 Another study limitation we should take into consideration is the elevated presence of small SB with a rate of use, in our sample, of DCB sizes < 2.25 mm of 43.7%. This would make target lesion failure go clinically inadvertently in some of these cases. Finally, we should mention that this study is limited by the relatively small number of patients included. Also, because due to its observational nature, no selection biases can be excluded.
CONCLUSIONS
The findings presented here show the experience of a single center with a very low rate of acute procedural complications, and a low rate of long-term adverse events despite dealing very high-risk profile lesions and patients with a 3.6% rate of target lesion failure reported. It is crucial to select the right type of lesions that can benefit from such therapy (basically the lack of a large plaque burden in the SB), a very refined technique of lesion preparation, and a greater use of tools to guide the angioplasty like intracoronary ultrasound or optical coherence tomography, preferably in ISR-type of lesions whose clinical progression is more unfavorable compared to that of de novo lesions. Despite the low rate of adverse events reported since no comparison with a control group was made, no definitive conclusions can be drawn on the advantages of DCBs in this clinical setting. We can only say that both in the «real-world» and the routine clinical practice described here, such strategy yields good long-term results without prejudice to other strategies may have given better or worse results regarding effectiveness. Randomized clinical trials are needed with enough statistical power and large enough samples to corroborate the promising data obtained from former studies to confirm or discard the superiority of DCB in the management of the SB in coronary bifurcation lesions. Until that time, the DCB can be considered a therapeutic tool that can be tremendously useful to improve the long-term results obtained in this type of complex lesions.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
J. Valencia drafted the manuscript. J. Valencia, F. Torrez-Mezcua, and M. Herrero-Brocal participated in data curation, and in the clinical follow-up of the patients. J. Valencia, J. Pineda, P. Bordes, F. Torres-Saura, and J.M. Ruiz-Nodar participated in patient recruitment and in the manuscript critical review process. All the authors gave their final approval to the manuscript.
CONFLICTS OF INTEREST
None reported.
WHAT IS KNOWN ABOUT THE TOPIC?
- To this date, there is a limited number of studies that have analyzed the role of DCB to treat the SB of coronary bifurcation lesions. Although such role seems beneficial regarding the improvement of the parameters analyzed, this still has not translated into a clear significant improvement of clinical parameters like target lesion/vessel failure or need for new revascularizations. On the other hand, the exact relevance of the SB and the role it plays in the short- and long-term prognosis of coronary bifurcation lesions remains unknown.
WHAT DOES THIS STUDY ADD?
- Our registry provides the experience of a single large volume center treating this type of lesions with a long follow-up. Also, it represents the «real-world» setting, that has been considered cut off from large randomized clinical trials too many times. The favorable results obtained in our study in a very unfavorable clinical and anatomical setting can situate the DCB as an extremely useful tool to improve the long-term results of percutaneous coronary interventions performed on coronary bifurcation lesions at our cath labs.
REFERENCES
1. Sawaya FJ, Lefèvre T, Chevalier B, et al. Contemporary Approach to Coronary Bifurcation Lesion Treatment. JACC Cardiovasc Interv. 2016;9:1861-1878.
2. Spitzer A, McFadden E, Vranckx P, et al. Critical Appraisal of Contemporary Clinical Endpoint Definitions in Coronary Intervention Trials: A Guidance Document. JACC: Cardiovasc Interv. 2019;12:805-819.
3. Jeger RV, Eccleshall S, Wan Ahmad WA, et al. Drug-Coated Balloons for Coronary Artery Disease: Third Report of the International DCB Consensus Group. JACC Cardiovasc Interv. 2020;13:1391-1402.
4. Oh GC, Park KW, Kang J, et al. Association of Side-Branch Treatment and Patient Factors in Left Anterior Descending Artery True Bifurcation Lesions: Analysis from the GRAND-DES Pooled Registry. J Interv Cardiol. 2020. https://doi.org/10.1155/2020/8858642.
5. Mori H, Torii S, Harari E, et al. Pathological mechanisms of left main stent failure. Int J Cardiol. 2018;263:9-16.
6. Stella PR, Belkacemi A, Dubois C, et al. A multicenter randomized comparison of drug-eluting balloon plus bare-metal stent versus bare-metal stent versus drug-eluting stent in bifurcation lesions treated with a single-stenting technique: six-month angiographic and 12-month clinical results of the drug-eluting balloon in bifurcations trial. Catheter Cardiovasc Interv. 2012;80:1138-1146.
7. López Mínguez JR, Nogales Asensio JM, Doncel Vecino LJ, et al. A prospective randomised study of the paclitaxel-coated balloon catheter in bifurcated coronary lesions (BABILON trial): 24-month clinical and angiographic results. EuroIntervention. 2014;10:50-7.
8. Berland J, Lefèvre T, Brenot P, et al. DANUBIO — a new drug-eluting balloon for the treatment of side branches in bifurcation lesions: six-month angiographic follow-up results of the DEBSIDE trial. EuroIntervention. 2015;11:868-876.
9. Herrador JA, Fernandez JC, Guzman M, Aragon V. Drug-eluting vs. conventional balloon for side branch dilation in coronary bifurcations treated by provisional T stenting. J Interv Cardiol. 2013;26:454-462.
10. Mathey DG, Wendig I, Boxberger M, Bonaventura K, Kleber FX. Treatment of bifurcation lesions with a drug-eluting balloon: the PEPCAD V (Paclitaxel Eluting PTCA Balloon in Coronary Artery Disease) trial. EuroIntervention. 2011;7 Suppl K:K61-65.
11. Kleber FX, Rittger H, Ludwig J, et al. Drug eluting balloons as stand alone procedure for coronary bifurcational lesions: results of the randomized multicenter PEPCAD-BIF trial. Clin Res Cardiol. 2016;105:613-621.
12. Jing QM, Zhao X, Han YL, et al. A drug-eluting Balloon for the trEatment of coronarY bifurcatiON lesions in the side branch: a prospective multicenter ranDomized (BEYOND) clinical trial in China. Chin Med J. 2020;133:899-908.
13. Zheng Y, Li J, Wang L, et al. Effect of Drug-Coated Balloon in Side Branch Protection for de novo Coronary Bifurcation Lesions: A Systematic Review and Meta-Analysis. Front Cardiovasc Med. 2021;8:758560.
14. Liu H, Tao H, Han X, et al. Improved Outcomes of Combined Main Branch Stenting and Side Branch Drug-Coated Balloon versus Two-Stent Strategy in Patients with Left Main Bifurcation Lesions. J Interv Cardiol. 2022. https://doi.org/10.1155/2022/8250057.
15. Li Y, Mao Q, Liu H, Zhou D, Zhao J. Effect of Paclitaxel-Coated Balloon Angioplasty on Side Branch Lesion and Cardiovascular Outcomes in Patients with De Novo True Coronary Bifurcation Lesions Undergoing Percutaneous Coronary Intervention. Cardiovasc Drugs Ther. 2021. https://doi.org/10.1007/s10557-021-07225-8.
16. Harada Y, Colleran R, Pinieck S, et al. Angiographic and clinical outcomes of patients treated with drug-coated balloon angioplasty for in-stent restenosis after coronary bifurcation stenting with a two-stent technique. EuroIntervention. 2017;12:2132-2139.
* Corresponding author.
E-mail address: jvalenciam@hotmail.com (J. Valencia).