Innovation in interventional cardiology
High-definition intravascular ultrasound
30/04/2019
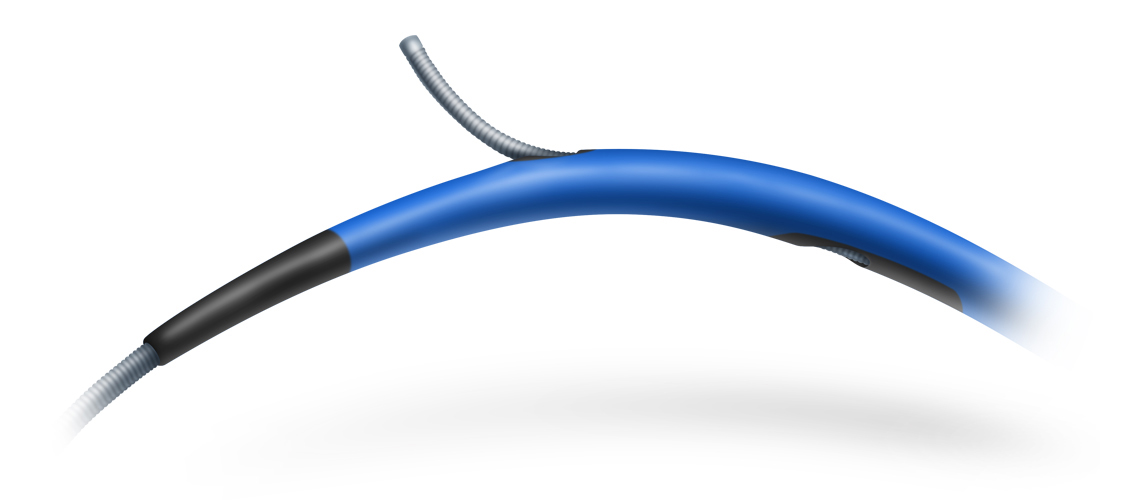
For a while now, several models of dual-lumen microcatheters have been available to interventional cardiology units to address common problems that occur in everyday practice. These devices can be used in certain bifurcations to access difficult-to-reach side branches with unfavorable angles, in complex coronary dissections, and, above all, in interventions for chronic total occlusion to facilitate the LAST (limited antegrade subintimal tracking) technique1. The dual lumen microcatheters that are currently available are characterised by a rapid exchange monorail lumen that runs to the tip of the catheter and a coaxial lumen with lateral exit port.
A different microcatheter is available, with two coaxial lumens (RECROSS; IMDS); one of these runs to the tip of the microcatheter and the other runs to two lateral exit ports at 8 and 12 mm from the tip, positioned 180° from each other. This modification solves one of the problems of conventional microcatheters when the lateral port is not directed toward the area of interest: the ostium of the side branch, the true lumen in a dissection, or intraplaque in an occluded segment. Having a second port facing the opposite direction allows the user to withdraw the coronary guidewire via the opposite side while still looking at the area of interest.
This microcatheter has a 1.5 Fr tip, hydrophilic coating and a stylet for increased support and access to more difficult areas.
Nonetheless, whenever using these devices, it is essential to have a good three-dimensional orientation of the architecture of the vessel we are working in, to obtain the maximum efficiency from the microcatheter.
References
1 . Michael TT, Papayannis AC, Banerjee S, Brilakis ES. Subintimal Dissection/Re-entry Strategies in Coronary Chronic Total Occlusion Interventions. Circ Cardiovasc Interv. 2012;5:729–738.
Keywords Chronic total occlusions, microcatheter, dual-lumen microcatheter, rre-entry
Recently, data were published on a device for the treatment of New York Heart Association (NYHA) class III-IV/IV heart failure in patients with impaired or preserved ventricular function1,2.
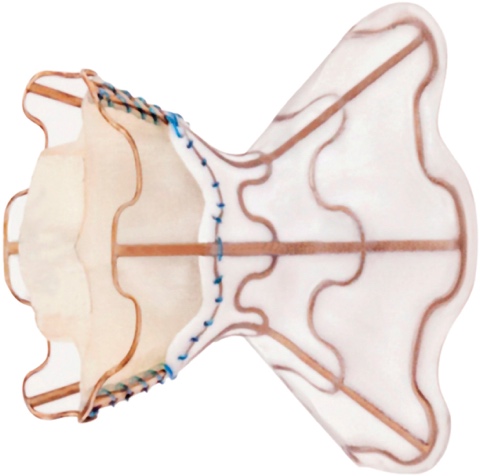
The medical treatment of heart failure can be complemented with cardiac resynchronization devices, ventricular assistance, and transplantation. It is now possible to add a new device: a one-way, hourglass-shaped bioprosthesis that is implanted in the interatrial septum via transseptal puncture. The aim of this treatment is to create a left-to-right shunt in patients with a high left atrial pressure or very restrictive left atrium. This decongestion reduces the pulmonary capillary pressure at rest and during exercise, with a small reduction in cardiac output. The created shunt is small, with a Qp/Qs of approximately 1.27. The volume overload on the right ventricle is low, so the probability of causing pulmonary hypertension is low.
The risk of complications from the procedure is very low: there is a risk of cardiac tamponade, essentially due to the transseptal access (2.6%). However, the improvement in functional class and exercise capacity is significant, as is the reduction in hospitalization, transplantation, ventricular assistance and pulmonary capillary pressure. Nonetheless, some complications have been reported at 12 months’ follow-up, including valve closure in 14% of patients and valve stenosis in 36%.
The technological innovation in this field is promising for the improvement of symptoms in patients with heart failure; in the coming years we will see advances to avoid stenosis in these devices with new randomized trials.
References
1 . Rodés-Cabau J, Bernier M, Amat-Santos IJ, et al. Interatrial shunting for heart failure: early and late results from the first-in-human experience with the V-Wave system. J Am Coll Cardiol Intv. 2018; 11, 2300-2310. Epub ahead of print.
2 . Sorajja P, Samara M, Eckman P. Atrial shunting for heart failure: where do we need to go? J Am Coll Cardiol Intv. 2018;11,2311-2313. Epub ahead of print.
Keywords: interatrial shunt, heart failure

