The management of symptomatic coronary artery disease in older adults presents a conundrum. Depending on their residual life expectancy, treatment is focused more on quality of life and symptomatic relief than on the improvement of long-term prognosis. Consequently, coronary artery bypass grafting (CABG) often is not an option, not only because of an increased and sometimes prohibitive risk but also because of the slow or even incomplete recovery after major surgery in older adults. On the other hand, medical treatment alone is of limited efficacy and may result in polypharmacy, with associated problems of adherence and drug interaction. Thus, percutaneous coronary intervention (PCI) may remain the only reasonable option. Nevertheless, PCI in older adults is often technically challenging and carries a substantially increased risk compared with PCI in younger patients.1 The extent and location of coronary artery disease appear to be even more important in older adults than in younger patients. Specifically, the risk of PCI in older patients is increased by more than twofold, if it involves the left main coronary artery as compared with PCI in other territories.1
Thus, guidance on left main PCI in older adults is particularly needed. There is, however, a paucity of data to aid treatment decisions in this setting. Older age groups are scarcely represented in the randomized trials that inform current guidelines.2 As a first approach to this problem, it may be important to learn how the outcomes of left main PCI in older adults differ from those in the younger age groups included in pivotal trials.
The study by Gallo et al.,3 recently published in REC: Interventional Cardiology, is an important first step in this direction. This retrospective, single-center observational study investigated all older adult (≥ 75 years) patients undergoing left main PCI at the Cardiology Service of the Hospital Universitario Reina Sofía (Córdoba, Spain) between 2017 and 2021. Gallo et al. identified 140 patients with a median age of 80 years and a median SYNTAX score of 21, similar to those in published randomized studies. Highlighting the clinical relevance of the issue, these patients represented as much as 32% of their left main PCI cohort.
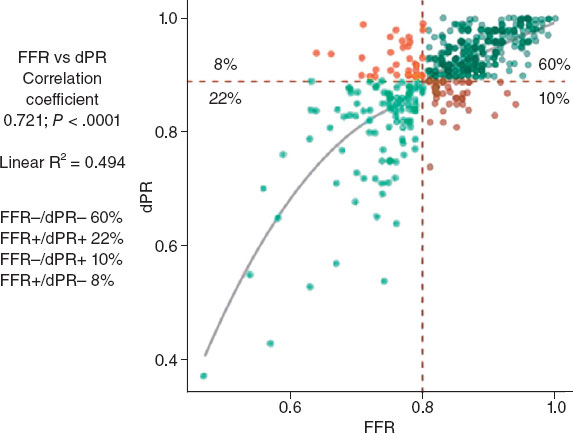
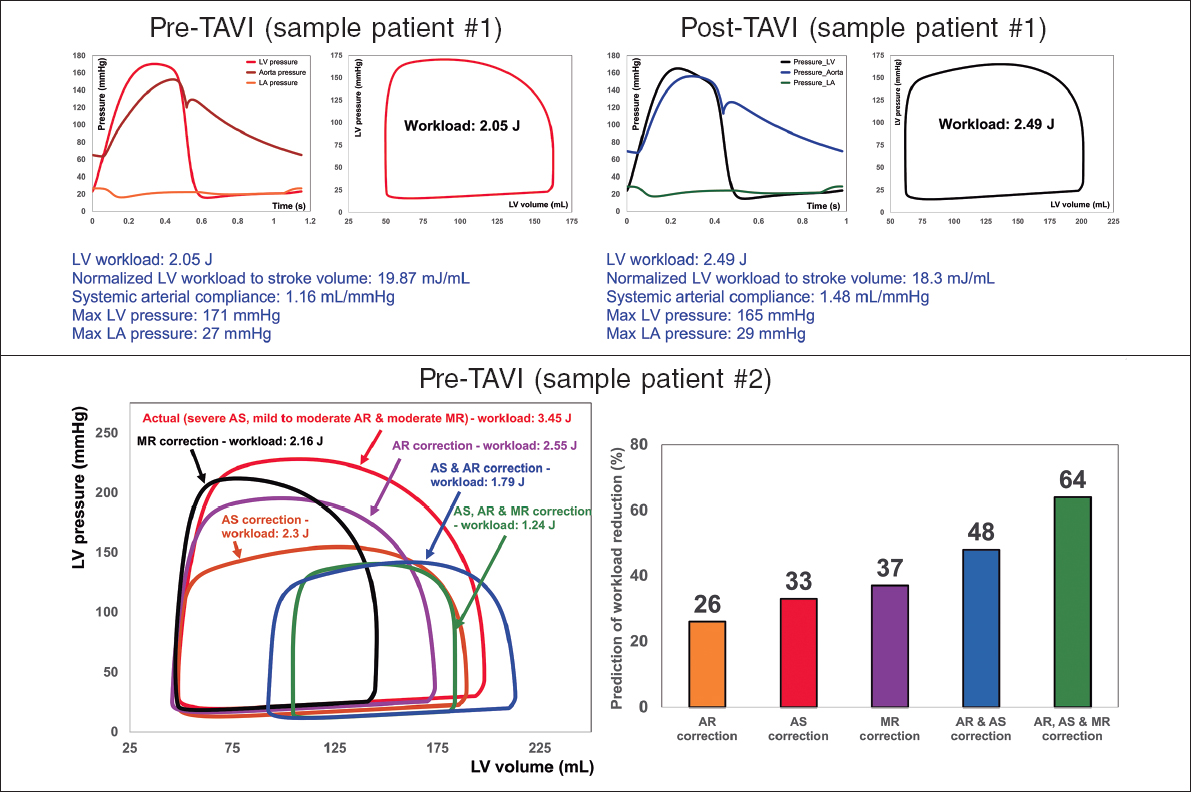
With a median follow-up of 19 months (interquartile range, 5-35 months), Gallo et al. found substantial differences in outcomes for their left main PCI cohort of older adults compared with published outcomes in pivotal randomized trials comparing left main PCI with CABG (figure 1). In these trials, patients had to be eligible for CABG and were approximately 14 years younger.4 As shown by a recent individual patient data meta-analysis, outcomes in the pivotal trials were driven by nonfatal cardiac events rather than mortality.4 In the current cohort of Gallo et al., however, only 2.1% had a spontaneous nonfatal myocardial infarction during the 2-year follow-up and reintervention was indicated in only 4.3%, whereas 2-year mortality was 27.1%.3
Figure 1. Two-year outcomes of left main percutaneous coronary intervention (PCI) in older adults in the study by Gallo et al.3 compared with younger patients included in randomized studies comparing PCI with coronary artery bypass grafting.4 Percentages were derived from numbers of events divided by total number of patients for older adults and from Kaplan-Meier estimates for younger patients. The incidence of noncardiovascular death in younger patients was imputed based on the reported proportion of 44% for noncardiovascular death at 5 years. MI, myocardial infarction.
The younger patients in the randomized trials had a substantially better prognosis with a 2-year mortality of only 4.5%. In these patients, outcomes were dominated by spontaneous myocardial infarction and reintervention, with 2-year incidences of 3.0% and 9.6%, respectively.4 According to the individual patient data meta-analysis, CABG substantially reduced these latter events—to 1.6% and 3.4%, respectively—but did not significantly improve survival.
In this context, the results of the study by Gallo et al. are important. They show that the contribution of those events where CABG clearly outperforms PCI (ie, spontaneous myocardial infarction and reintervention) is less relevant in older adults than in the younger patients of the randomized trials.
In the population of older adults in the study by Gallo et al., deaths that could be clearly attributed to noncardiac causes were more frequent than in younger patients. The incidence of noncardiac death was 7.1% at the 2-year follow-up after left main PCI in older adults, while it ranged around 2% in the younger patients of randomized studies on left main PCI (figure 1). This indicates a higher number of deaths not amenable to any cardiovascular treatment in older patients compared with younger patients.
Although higher in absolute numbers, the proportion of deaths that could be attributed unequivocally to noncardiac causes was lower in older adults than in younger patients (figure 1). This finding is, however, difficult to interpret. In line with common practice, deaths of unknown cause were counted as cardiac deaths. Thus, we do not know how many of these deaths were from true cardiac causes, let alone what proportion of deaths were due to treatment failure of left main PCI.
Despite these uncertainties, the study by Gallo et al. shows that in older adults with left main PCI, the causes of death not related to myocardial revascularization were more frequent than in younger patients undergoing left main PCI.
Mortality was driven less by calendar age and more by frailty. Gallo et al. stratified their cohort into nonfrail and frail groups, as defined by a frailty score of 3 or higher. As many as 57% of the frail patients had died at the 3-year follow-up compared with 23% of the nonfrail patients (P = .001) (for 2-year mortality, see figure 1). After inverse probability of treatment weighting with a number of variables including age, this difference in all-cause mortality remained substantial and statistically significant (23 % vs 44%; P = .046). Thus, frailty, but not age or SYNTAX score, was a significant independent predictor of mortality (multivariable hazard ratio = 2.4; 95% confidence interval, 1.2-5.0; P = .018).These findings are in line with a recently published study on PCI in older adults that identified frailty, but not calendar age, as a strong predictor of mortality.5
The high mortality of older adults with left main coronary disease despite PCI poses the question of futility, particularly in frail patients. While PCI may indeed be futile in terms of prolonging life, it may still alleviate symptoms. In this regard, it is important to note that PCI in the study by Gallo et al. could be accomplished without complications in 94% of the patients (92% of frail patients and 97% of nonfrail patients), and 91% of the patients left the hospital alive, even though 50% of them had presented with acute myocardial infarction. Thus, there is no prohibitive complication rate that justifies withholding left main PCI in older adults as an attempt to improve symptoms. Moreover, the randomized After Eighty study found that myocardial revascularization reduced the risk of myocardial infarction and urgent revascularization in older patients with acute coronary syndromes.6 Thus, PCI in older adults, particularly for the left main, may offer more than just relief from angina or angina equivalents. The low incidences of spontaneous myocardial infarction and reintervention found by Gallo et al. after left main PCI may thus reflect the positive effects of the procedure. However, in the absence of a control group such interpretation remains speculative. Moreover, the number of patients in this retrospective observational study is limited. Together, with the single-center design of the study, this weakens the generalisability of the current findings.
Nevertheless, 3 important messages of the study by Gallo et al. prevail: a) left main PCI in older adults is a reasonable option with a fair procedural success rate; b) the clinical course after left main PCI differs substantially from that in younger patients with death being far more common than nonfatal cardiovascular events; c) frailty is more relevant to prognosis than calendar age, being a central determinant of mortality after left main PCI. Further studies are needed to determine how best to integrate these findings into individualized treatment decisions in older adults presenting with symptomatic left main disease.
FUNDING
None.
CONFLICTS OF INTEREST
F-J. Neumann has received consultancy honoraria from Novartis and Meril, speaker honoraria from Boston, Amgen, Daiichi-Sankyo and Meril and reports speaker honoraria paid to his institution from BMS/Pfizer as well as research grants paid to his institution from Boston and Abbott.
REFERENCES
1. Jalali A, Hassanzadeh A, Najafi MS, et al. Predictors of major adverse cardiac and cerebrovascular events after percutaneous coronary intervention in older adults:a systematic review and meta-analysis. BMC Geriatrics. 2024;24:337-349.
2. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
3. Gallo I, Hidalgo F, González-Manzanares R, et al. Percutaneous treatment of the left main coronary artery in older adults. Impact of frailty on med-term results. REC Interv Cardiol. 2024. https://doi.org/10.24875/RECICE.M24000460.
4. Sabatine MS, Bergmark BA, Murphy SA, et al. Percutaneous coronary intervention with drug-eluting stents versus coronary artery bypass grafting in left main coronary artery disease:an individual patient data meta-analysis. Lancet. 2021;398:2247-2257.
5. Shimono H, Tokushige A, Kanda D, et al. Association of preoperative clinical frailty and clinical outcomes in elderly patients with stable coronary artery disease after percutaneous coronary intervention. Heart Vessels. 2023;38:1205-1217.
6. Tegn N, Abdelnoor M, Aaaberge L, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study):an open-label randomised controlled trial. Lancet 2016;387:1057-1065.