Two decades of transcatheter aortic valve implantation (TAVI) changed the history of contemporary medicine and became a reference model in cardiovascular disease. Percutaneous structural heart disease (SHD) therapies emerged to treat the entire heart valve and vessel spectrum, as well as congenital or acquired wall and muscular defects.
(R)evolution happened back in 2002 with Alain Cribier’s human aortic valve disease percutaneous milestone treatment.1 A progressive and impressive range of therapeutic alternatives for patients grew parallel to the population’s longevity given the most prevalent etiology of aortic stenosis is degenerative. In fact, cardiovascular diseases remain the leading causes of death and hospitalization and represent an enormous clinical and public health burden, which disproportionately affects older adults. The World Health Organization expects octogenarians to quadruple up to 396 million by 2050. Although rheumatic heart disease has become rare in industrialized countries, its overall burden is still significant. It comes as no surprise that complex patients who can benefit from combined valvular procedures are increasingly common.
The TAVI impact on cardiology and cardiac surgery surpassed the clinical field and imposed a restructure as the path taken in aortic valve disease is transposed, progressively, to other structural clinical areas, namely mitral, tricuspid, and acute stroke prevention.
WHAT’S THE STORY?
Initially, safety and efficacy were the main requirements for TAVI, same as for any other cardiovascular technique. Mortality and complications were important from a clinical point of view resulting in prolonged admissions and increased hospital costs. Intensive use of imaging and general anesthesia were the default procedure for most. Patient selection became the concern and frailty assessment, risk stratification, futility, and the imponderables were the main issues. Bench simulation provided relevant information while studies and registries depicted the actual TAVI expression across countries.2-4
Progressively, innovative techniques and devices led to cautious simplified protocols that run parallel to image expertise replication in the non-aortic space, especially in the mitral valves. Patient subgroups were the main topic, namely the history of cardiac valve surgery –aortic, mitral, and tricuspid– as well as octogenarians. The economic burden of incremental cost on health economics emerged as a concern, as well as device selection, hybrid techniques, alternative access routes, and standardized approaches for complications. Concomitant medical therapy and longevity were also captured.5,6
Therefore, the field of aortic procedures expanded, grew, and consolidated. TAVI procedures became daily routine with hands-on training for fellows. The need for preparing interventional cardiologists for this area became clear, which was reflected in industry proctoring programs and by the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Core Curriculum. Simultaneously, expansion to other SHD areas like percutaneous mitral and tricuspid valve procedures, left atrial appendage and valve leak closures emerged from this maturity as a natural (r)evolution in the field of SHD.7-10
WHAT DID WE LEARN?
Aortic valve procedures reflect, first, contemporary longevity and modern medicine. Their expansion constitutes a role model in cardiology and cardiac surgery by inducing changes adopted in other SHD areas.
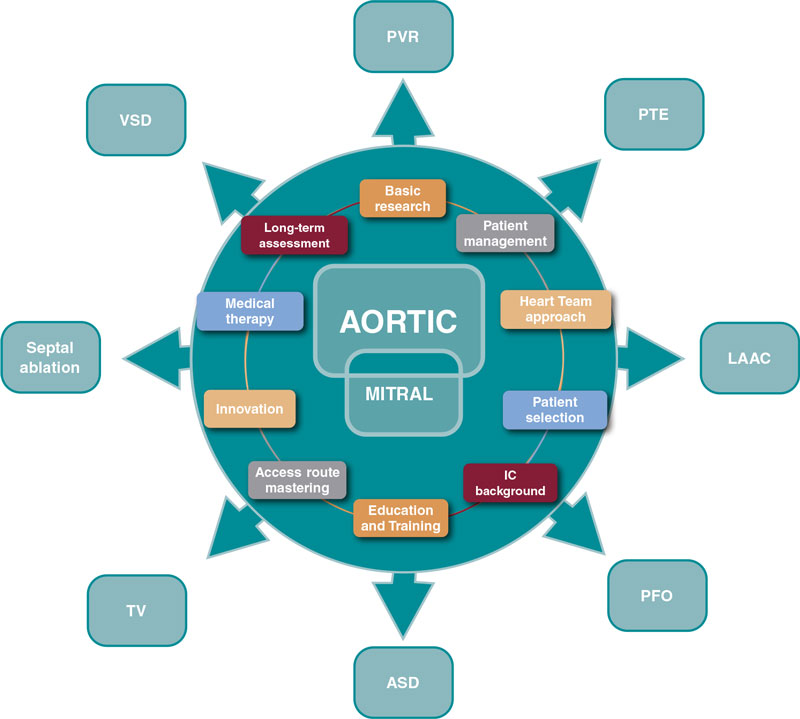
Several SHD procedures have the extraordinary ability to ameliorate heart failure, prevent and treat thromboembolic diseases, and improve survival.11 We should recognize and acknowledge the common features that bring their current prestige, success, and expansion. Among immense factors, the following may be considered the most relevant:
- – Basic research
- – Comprehensive patient management
- – Multidisciplinary approach
- – Patient and subset selection
- – Access route mastering
- – Interventional cardiology background
- – Device iteration and innovation
- – Structured education and training
- – Complementary medical therapy
- – Long-term assessment of care and outcomes
Progress is endless and these are valuable assets to guide the next steps (figure 1).
Figure 1. Influence of aortic and mitral procedures in structural heart disease. ASD, atrial septal defect; IC, interventional cardiology; LAAC, left atrial appendage closure; PFO, patent foramen ovale; PTE, pulmonary thromboembolism; PVR, paravalvular regurgitation; TV, tricuspid valve; VSD, ventricular septal defect.
WHAT DOES THE FUTURE LOOK LIKE?
Physicians, caretakers, industry, and policy makers conquered a huge responsibility in the field of SHD.
To match societal and patient’s expectations, the interventional cardiologist needs a holistic approach:
- – To define the role of SHD interventional cardiologists. As a medical cardiologist who manages patients from diagnosis to follow-up of SHD and performs percutaneous procedures in this domain. As members of heart teams that interact closely with other cardiologists, cardiac surgeons, and other medical specialties, nurses, paramedics, and other healthcare professionals.11 All these considerations are based on the EAPCI Core Curriculum of 2020 and on the upcoming EAPCI Core Curriculum on percutaneous SHD procedures (submitted for publication).10
- – To harmonize SHD interventional cardiology practice. Data from health surveys, administrative records, cohort studies, and registries show persisting geographic inequity across Europe. The EAPCI certification that includes a national mutual recognition system, attempts to validate a proper level of knowledge and practice to protect patients from undergoing interventional cardiology procedures performed by unqualified professionals and set up a European standard for competency and excellence in this field.10
- – To promote and assess quality of care by adopting standardized data definitions for the quantification of quality of care and outcomes. Recently, the EuroHeart methodology reached consensus on a set of variables, 93 categorized as mandatory (level 1) and 113 as additional (level 2) based on their clinical importance and feasibility.11 That facilitates quality improvement, observational research, registry-based randomized trials, benchmarking and post-marketing surveillance of devices, and pharmacotherapies.12
- – To perform TAVI in centers without permanent onsite cardiac surgery by establishing straight-forward protocols that provide patient safety and ensure that both operators and hospitals are committed to high quality outcomes. Though TAVI in centers without permanent onsite cardiac surgery is not endorsed at present, the dramatic growth of candidates outpaced the efforts, prompting increased waiting times with negative and severe clinical consequences. Models should include an optimal heart team around the patient from periodic visiting teams to an overall exchange partnership.13,14
- – To expand SHD procedures to low-risk and/or younger patients who present distinct challenges in their stratification, comorbidities, clinical presentation, anatomy, and potential longevity supported by recent trials. Also, by promoting responsible research and enhancing patient-centered solutions.14
- – To develop awareness regarding valvular heart disease since it is not commonly acknowledged by the population and because aortic, mitral, and tricuspid valves present overlapping functions, and differences regarding diagnostic and therapeutic methods. The EAPCI Valve for Life initiative detects barriers, identifies stakeholders, and implements strategic plans to overcome difficulties in different areas.15
- – To provide the referral network a simple, expeditious, and efficient articulation from the patient and the referring physician perspective by deploying and/or developing dedicated information technology solutions for treatment pathways and reshaping the future cardiovascular department (eg, by fusion or rotative leadership between cardiology and surgery).
CONCLUSION
In conclusion, percutaneous SHD procedures are highly demanding and rewarding. Lessons from the past are precious and interventional cardiology must use them wisely as access and volume are increasing significantly. A comprehensive approach is warranted to face this surge.
FUNDING
None whatsoever.
CONFLICTS OF INTEREST
R. Campante Teles declared no conflicts of interest associated with this manuscript.
REFERENCES
1. Cribier A. Development of transcatheter aortic valve implantation (TAVI): a 20-year odyssey. Arch Cardiovasc Dis. 2012;105:146-152.
2. López-Otero D, Teles R, Gómez-Hospital JA, et al. Transcatheter aortic valve implantation: Safety and effectiveness of the treatment of degenerated aortic homograft. Rev Esp Cardiol. 2012;65:350-355.
3. Simonato M, Azadani AN, Webb J, et al. In vitro evaluation of implantation depth in valve-in-valve using different transcatheter heart valves. EuroIntervention. 2016;12:909-17.
4. Mylotte D, Osnabrugge RLJ, Windecker S, et al. Transcatheter aortic valve replacement in Europe: Adoption trends and factors influencing device utilization. J Am Coll Cardiol. 2013;62:210-219.
5. Ruggeri M, Donatella M, Federica C, et al. The transcatheter aortic valve implantation: an assessment of the generalizability of the economic evidences following a systematic review. Int J Technol Assess Health Care. 2022;38:e27.
6. Van Gils L, Tchetche D, Latib A, et al. TAVI with current CE-marked devices: Strategies for optimal sizing and valve delivery. EuroIntervention. 2016;12:Y22-Y27.
7. Simonato M, Whisenant B, Ribeiro HB, et al. Transcatheter mitral valve replacement after surgical repair or replacement comprehensive midterm evaluation of valve-in-valve and valve-in-ring implantation from the VIVID registry. Circulation. 2021:104-116.
8. Gandaglia A, Bagno A, Naso F, Spina M, Gerosa G. Cells, scaffolds and bioreactors for tissue-engineered heart valves: A journey from basic concepts to contemporary developmental innovations. Eur J Cardio-thoracic Surg. 2011;39:523-531.
9. Agricola E, Ancona F, Brochet E, et al. The structural heart disease interventional imager rationale, skills and training: a position paper of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2021;22:471-479.
10. Van Belle E, Teles RC, Pyxaras SA, et al. EAPCI Core Curriculum for Percutaneous Cardiovascular Interventions (2020): Committee for Education and Training European Association of Percutaneous Cardiovascular Interventions (EAPCI). A branch of the European Society of Cardiology. EuroIntervention. 2021;17:23-31.
11. Aktaa S, Batra G, James SK, et al. Data standards for transcatheter aortic valve implantation: the European Unified Registries for Heart Care Evaluation and Randomised Trials (EuroHeart). Eur Hear J Qual Care Clin Outcomes. 2022;qcac063.
12. Guerreiro C, Ferreira PC, Teles RC, et al. Short and long-term clinical impact of transcatheter aortic valve implantation in Portugal according to different access routes: Data from the Portuguese National Registry of TAVI. Rev Port Cardiol. 2020;39:705–717.
13. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2021:1-72.
14. Foglietta M, Radico F, Appignani M, Aquilani R, Di Fulvio M, Zimarino M. On site cardiac surgery for structural heart interventions: a fence to mend? Eur Heart J Suppl. 2022;24(Supplement_I):I201-I205.
15. Windecker S, Haude M, Baumbach A. Introducing a new EAPCI programme: The Valve for Life initiative. EuroIntervention. 2016;11:977-979.