QUESTION: Do we have enough evidence to be able to say that the coronary recanalization of a chronic total coronary occlusion (CTO) improves the prognosis of patients?
ANSWER: I would say so. I believe it is hard to have well-designed, randomized clinical trials with large populations of patients and long follow-up periods on this issue comparing the 3 possible strategies of treatment (drugs, surgery, and percutaneous coronary interventions) which, by the way, are the prerequisites to show some mortality net benefit in this group of patients. Also, the results from the procedures performed in the different groups are not comparable whatsoever.
On the other hand, if we look at the registries already published and presented in congresses over the last few years (3-4 years), we will see that only those with long follow-up periods are positive. Usually, the revascularization of a CTO has no implications in the rate of infarction at follow-up, yet the overall and cardiac mortality rate of non-revascularized patients compared to revascularized patients (both percutaneously and using surgery) trebles compared to the population of patients with CTO who are on medical treatment.
The only 2 randomized clinical trials ever published that compare the clinical evolution of patients with a CTO based on the treatment received (medical vs interventional) are the EuroCTO1 and the DECISION-CTO trials.2 Unfortunately, both were interrupted before reaching the population for which they were designed due to their low patient inclusion rate. Their results are contradictory, unfavorable in the DECISION-CTO and favorable in the EuroCTO trial, but their designs are very different. In the DECISION-CTO trial, patients with multivessel disease received treatment in non-occluded vessels at the interventional cardiologist’s criterion; as a matter of fact, 50% of the patients in both groups received treatment with angioplasty of vessels without chronic occlusions. On the other hand, in the EuroCTO trial the non-occluded vessels of patients with multivessel disease were systematically revascularized and then randomized to receive medical treatment or undergo angioplasty for their CTO. Also, in the DECISION-CTO clinical trial there is a high rate of crossing between the different modalities of treatment: 3 days after randomization, 19.6% of patients form the medical treatment arm crossed to the revascularization arm vs 7.3% at 12 months in the EuroCTO trial. In the DECISION-CTO trial, at the 4-year follow-up, no differences were seen between the 2 arms in the following events: death, infarction, stroke, and revascularization (22.3% vs 22.4%; P = .86) or in the quality of life test results. Conversely, in the EuroCTO clinical trial the scores measuring the quality of life improved significantly in the invasive treatment arm, and the 12-month adverse events were similar in both arms.
Q.: In what subgroups of patients or situations should we expect to see greater prognostic benefits?
A.: We should focus on higher risk populations that are probably under-represented here.
Diabetics with CTO have a higher incidence of multivessel disease, more calcified blood vessels, and more risk factors compared to non-diabetic patients. Insulin-dependent diabetic patients with renal failure are the subpopulation with the most somber prognosis of all. In all the clinical trials conducted so far, the success rate of the angioplasty in the management of CTO is lower than that of non-diabetic patients. Also, to this day, from the prognostic point of view, surgery is superior to angioplasty, meaning that we should probably be very cautious when indicating an angioplasty for a CTO in these patients.
The subgroup of elderly patients (≥ 75 years) is a particularly frail population with worse left ventricular ejection fraction (LVEF), worse renal function, and a higher incidence of multivessel disease and left main coronary artery disease compared to patients < 75 years. The oldest patients are revascularized less frequently and with a lower success rate, but procedural complications are similar to the ones we find in younger patients. When selecting our patients, we should take into consideration that the age, creatinine, and ejection fraction (ACEF) score, high SYNTAX scores, and damage to the left main coronary artery are prognostic factors that we should take into consideration in this population of patients regardless of short-term mortality. We should not forget that, at the 4-year follow-up, the mortality rate of patients ≥ 75 years with CTO doubles that of patients < 75 years with CTO and that, in non-revascularized elderly patients, mortality doubles compared to revascularized patients. So maybe we should take a different approach towards this often-under-represented population.
Even though women with CTO have a higher incidence of risk factors compared to men with CTO and even though they amount to 15% of the studies population, the rates of success and complications between sexes are similar.
Another especially sensitive group is that of patients with CTO and a low LVEF. The angioplasty of the CTO is not accompanied by higher rates of complications or lower rates of success, and the improved prognosis is obvious because even though it is indicated it has proven to improve the LVEF.
Q.: And regarding symptom and functional improvement?
A.: The answer is affirmative in both cases. The studies conducted so far using magnetic resonance imaging allow us to say that the revascularization of a CTO in patients with preserved LVEF is accompanied by significant reductions in the amount of ischemic segments and the corresponding improvement of segmental contractility. There is a positive remodeling of the left ventricle with reduced end-diastolic volume. Also, if the necrotic mass is compared at baseline and at 6 months, we will see that it does not grow any bigger, which shows how safe the procedure of revascularization really is.
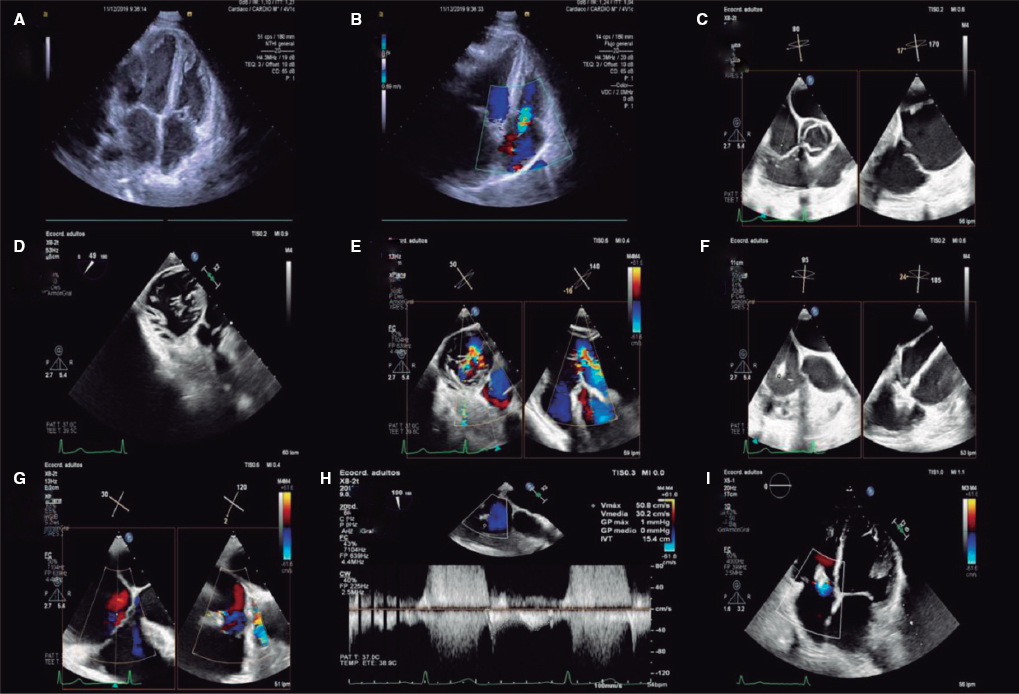
If we focus on the most fragile patients of all with the highest possible benefits such as patients with CTO and a LVEF < 40%, the results are more noticeable. Our group published the results of the 6-month follow-up of a group of 29 patients in whom we also found less ischemic segments, better contractility, and a 6 percentage-point improved LVEF (31.3% ± 7.4% vs 37.7 ± 8; P < .001) with significant functional repercussion, reduced brain natriuretic peptide levels (323 ± 657 pg/mL [95% confidence interval (95%CI), 60.4-238.2] vs 123 ± 151 pg/dL [95%CI, 40.6 ± 154.5]; P = .004), improved heart failure functional classification (New York Heart Association baseline functional class I and II: 72% vs 100%; P = .004), and improved angina pectoris (34.4% in baseline situation vs 3.1% at follow-up; P = .002).3
The greatest contribution of the EuroCTO trial after the 12-month follow-up is showing that there is a significant improvement in the scores used to measure quality of life (Seattle Angina Questionnaire) with a lower frequency of angina (5.23; 95%CI, 1.75-8.71; P = .003), better quality of life (6.62; 95%CI, 1.78-11.46; P = .007), fewer limitations to do physical activity (81.1; 95%CI, 77.6-100 with angioplasty vs 75.9; 95%CI, 71.3-80.5 with medical treatment; P = .02), and a larger number of patients completely asymptomatic in the group treated with angioplasty compared to the group that received medical treatment (71.6% vs 5.8%; P = .008).
Q.: What clinical indications does the percutaneous revascularization of a CTO have?
A.: If we follow the recommendations established by the European Society of Cardiology,4 the revascularization of CTO has a grade IIa indication with a B-level of evidence as long as patients have medical treatment-resistant angina or a well-documented wide ischemic region. As far as I know, these recommendations are not consistent with the routine daily practice.
The requirements to revascularize a CTO should be the same as for the revascularization of significant stenosis, that is, confirmed ischemia, current feasibility, and symptoms. However, regarding the symptoms, at least in my own experience, most patients with CTO also have anginal equivalents, and often complain that they get tired easily and unjustifiably for their age or LVEF; and when they have progressive angina pectoris, most of the times it is due to a developing stenosis in the donor vessel of collateral circulation.
We know that if the underlying myocardium is viable, a CTO behaves functionally like a 99% stenosis. So, I believe that the revascularization of CTO should have the same indications as the revascularization of any other lesion, as long as the procedure is performed with guarantees and by experienced interventional cardiologists.
Q.: What practical recommendations can you share with us to approach the interventional management of CTO with higher levels of success?
A.: The field of CTO is really something special because it requires not only particular skills but also a special attitude. In my personal opinion, all interventional cardiologists who want to deal with CTO should have 2 basic characteristics: patience and perseverance.
Perseverance is key because, even if we are pretty good interventional cardiologists for all other types of lesions, the management of CTO requires a very specific and prolonged learning curve, estimated at around 50 annual cases for a minimum of 3 years to be able to reach an acceptable rate of success. Therefore, it is advisable that not all interventional cardiologists of the same center specialize in the management of CTO because nobody would reach the level of expertise required. A reasonable idea would be to estimate the number of interventional cardiologists based on the number of actual patients who would be treated based on the volume of cases handled by each center.
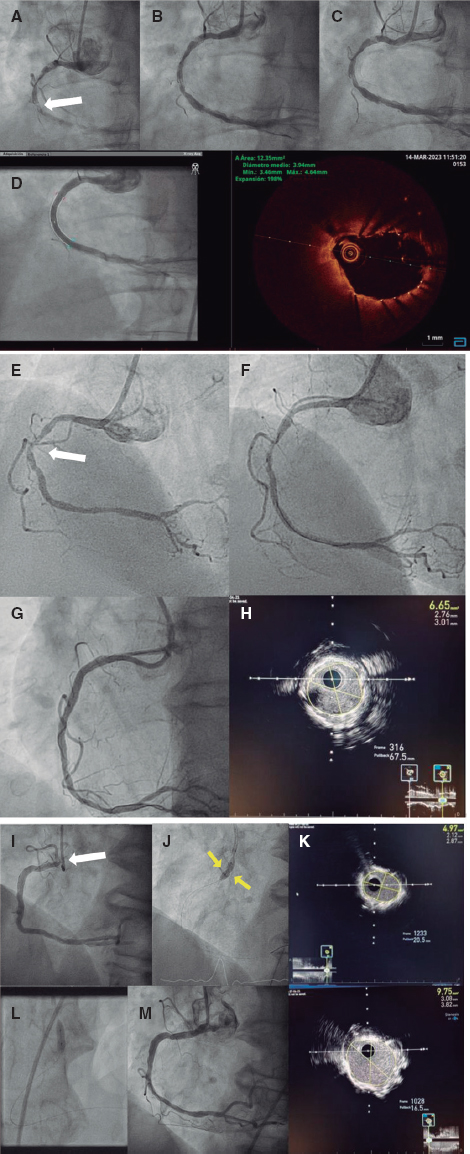
One can never stress enough something so simple as preparing the cases properly. It is essential to have deep knowledge of the coronary anatomy, that is, carry out a careful frame-by-frame review of the diagnostic coronary angiography to be able to characterize the plaque and the collaterals. Also, it is imperative to think of the material and the possible techniques that will be used. Added to the coronary anatomy, we also need good in-depth information on the patient, in particular his renal function, risk of bleeding, therapeutic adherence, capacity of collaboration, osteoarticular situation, and frailty.
We also consider the possibility of asking for help from other colleagues more experienced than us both at the beginning of the activity, and in second attempts in patients in whom we have already failed.
Another important issue is the material we plan to use because this is a field in continuous evolution. Although it is not possible to know every piece of equipment currently available, once we have made our choice, we need to know its characteristics, how it has been built, what it is designed to do, and how it should be used. Ongoing training is also important, so periodically attending specialized congresses are a good resource if we want to keep up to date.
It is essential to guarantee the patient’s safety; we should not forget that success means achieving TIMI (Thrombolysis in Myocardial Infarction) grade III flow without significant residual stenosis, loss of branches (a prognostic factor already confirmed long ago) and without any associated complications. The implementation of simple resources within our routine cath lab practice may help; here are a few examples: stop the procedure if losing collateral circulation and resume it if we think we can introduce some changes in the technique that we still have not used or have used incorrectly; ask the heart team to signal us whenever we have passed 3.7 times the volume of contrast administered in relation to the patient’s creatinine clearance levels to avoid contrast-induced nephropathy; and avoid high doses of radiation by asking the heart team to signal whenever we have reached the 3 Gy mark, and consider stopping the procedure whenever we come close to the 5 Gy mark if we have not made very significant advances, basically if we have not crossed the lesion with the guidewire.
CONFLICTS OF INTEREST
V. Martin-Yuste declared no conflicts of interest whatsoever regarding the writing of this manuscript.
REFERENCES
1. Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39:2484-2493.
2. Lee SW, Lee PH, Ahn JM, et al. Randomized Trial Evaluating Percutaneous Coronary Intervention for the Treatment of Chronic Total Occlusion. Circulation. 2019;139:1674-1683.
3. Cardona M, Martín V, Prat-Gonzalez S, et al. Benefits of chronic total coronary occlusion percutaneous intervention in patients with heart failure and reduced ejection fraction:insights from a cardiovascular magnetic resonance study. J Cardiovasc Magn Reson. 2016;18:78.
4. Neumann F-J, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
Corresponding author: 2 rue de Bastion, 17100 Saintes, France.
E-mail address: v.martin@ch-saintonge.fr (V. Martin-Yuste).