CASE PRESENTATION
This is the case of a 69-year-old man with a past medical history of sleep apnea syndrome, and chronic lower limb ischemia syndrome grade IIB. Smoking habit was among the patient’s cardiovascular risk factors reported until 2016, followed by arterial hypertension, type II diabetes mellitus, and dyslipidemia on medical therapy.
Back in January 2017, the patient was hospitalized due to second-degree atrioventricular block with implantation of a DDDR pacemaker. During hospitalization complete arrhythmia due to atrial fibrillation was confirmed that was eventually anticoagulated with rivaroxaban. In June 2017 the patient developed unstable angina with a diagnosis of severe aortic stenosis with left main coronary artery disease and 3-vessel disease. Surgical aortic valve replacement followed by revascularization with double left internal mammary artery bypass towards the left anterior descending coronary artery, and saphenous vein graft towards the second obtuse marginal branch was decided.
Currently, he complaints of angina-like symptoms during minimal exertion with a 5 to 6-month evolution, which is why cardiac catheterization was performed (prior to the procedure, the patient’s informed consent was obtained anticipating the possible publication of the case for teaching purposes). This study was performed via femoral access after discarding the arm that presented some issues. It showed the native bed with left main coronary artery disease and 3-vessel disease. The difference now was that the ostium of the native left circumflex artery was occluded, the bypass of the left internal mammary artery was patent, and the bypass of the saphenous vein towards the second obtuse marginal branch showed a highly severe lesion (figure 1, figure 2, and video 1 of the supplementary data).
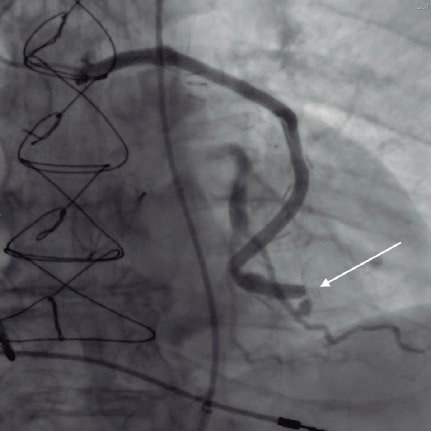
Figure 1. Focal lesion proximal to the termino-lateral anastomosis of the saphenous vein graft (white arrow).
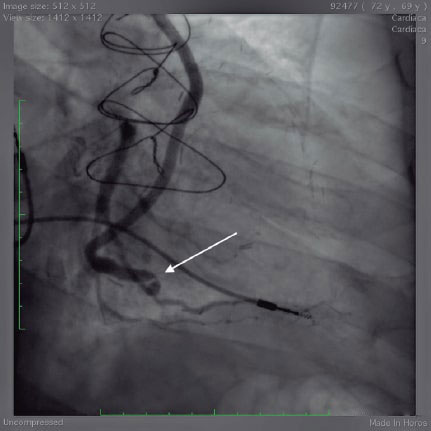
Figure 2. Focal angulated lesion of the saphenous vein graft towards the obtuse marginal branch (white arrow).
After studying the case and given the low chances of opening up the left circumflex artery native bed, it was decided to perform an interventional procedure on the saphenous vein culprit lesion. A 6-Fr AL2 guide catheter was accessed via right femoral access mounted on a SION blue Extra Support guidewire (Asahi Intecc, Japan). An attempt was made to advance a 2.5 mm x 12 mm balloon that proved unsuccessful because it never reached the lesion, which is why a 6-Fr guide extension catheter was inserted very close to the lesion (figure 3). Thanks to this support a balloon was advanced into the stenotic area and then predilated (figure 4 and video 2 of the supplementary data). However, a 3 mm × 8 mm Resolute Onyx zotarolimus-eluting stent was advanced unsuccessfully (figure 5 and video 3 of the supplementary data) even though that several maneuvers were tried including the buddy-wire technique.
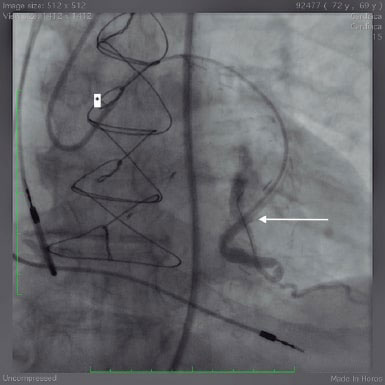
Figure 3. Note the tip of the guide extension catheter (white arrow) very close to the lesion, and the radiopaque distal part of the angioplasty guidewire inside the left circumflex artery (the asterisk corresponds to the tip of the guide catheter in the bypass ostium).
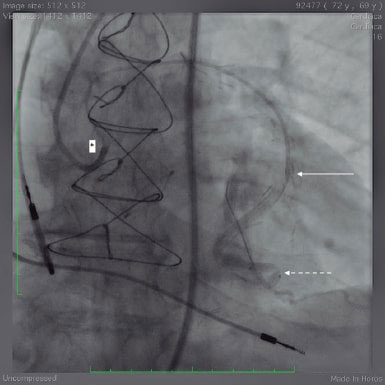
Figure 4. Note the radiopaque marks of the balloon placed in the lesion (dotted arrow). When trying to advance the device, the retreat of the radiopaque marks of the guide catheter (asterisk), and the guide extension catheter (white dotted arrow) becomes evident.
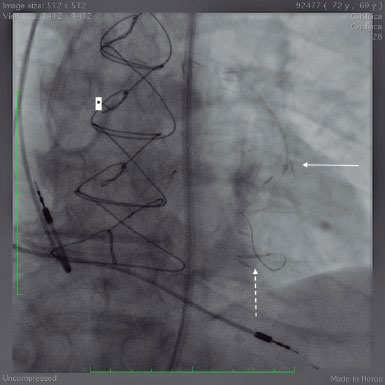
Figure 5. Inability of the Resolute Onyx zotarolimus-eluting stent (dotted arrow) to cross the lesion.
Taking into consideration that, in this case, support was optimal, how could the stent be implanted into the lesion?
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
J.R. Rumoroso Cuevas wrote, edited the text of this manuscript, and provided direct medical assistance to the patient. M. Sádaba Sagredo, and A. Subinas Elorriaga supervised the manuscript and contributed to its iconography
CONFLICTS OF INTEREST
None reported.
SUPPLEMENTARY DATA
Vídeo 1. Rumoroso Cuevas J.R. DOI: 10.24875/RECICE.M21000248
Vídeo 2. Rumoroso Cuevas J.R. DOI: 10.24875/RECICE.M21000248
Vídeo 3. Rumoroso Cuevas J.R. DOI: 10.24875/RECICE.M21000248
* Corresponding author: Barrio Labeaga s/n, 48960 Galdakao, Vizcaya, Spain.
E-mail address: rumo@secardiologia.es (J.R. Rumoroso Cuevas).












