CASE PRESENTATION
Anomalous pulmonary venous connection is a rare condition that occurs when 1 or more pulmonary veins abnormally return to the right atrium or systemic venous circulation. The most common type in adults is drainage of the left upper pulmonary vein (LUPV) into the left innominate vein. Anecdotally, an anomalous LUPV may have dual drainage into the left innominate vein and the left atrium (LA). In the absence of other congenital heart defects, partial anomalous pulmonary venous connection is often an incidental finding and individuals are usually asymptomatic.
In this article, we’ll be reporting on a case of dual drainage partial anomalous pulmonary venous connection where the LUPV is both connected to the left innominate vein and the LA in a patient with coronary heart disease and left ventricular systolic dysfunction.
This is the case of 56 year-old man with a past medical history of diabetes and dyslipidemia referred to the cardiac center due to an incidental finding on a thoracic computed tomography scan requested by the pulmonologist as part of a dyspnea diagnostic work-up. At the visit the patient presented with exertional dyspnea with NYHA functional class III and complained of angina on moderate exertion. The physical examination revealed normal auscultation and peripheral edema. The mentioned thoracic computed tomography scan revealed the presence of a LUPV connected to the LA and the left innominate vein trough a vertical vein (VV), as well as pulmonary artery dilation, cardiomegaly, and right pleural effusion (figure 1). Transthoracic echocardiography showed a moderate left ventricular dysfunction (ejection fraction, 35%) with global hypokinesis, LA and right atrium enlargement, right ventricular dilation and dysfunction (a 14 cm tricuspid annular plane systolic excursion) and elevated pulmonary artery systolic pressure (63 mmHg) (video 1 of the supplementary data). Right heart catheterization confirmed the presence of pulmonary hypertension (figure 2). Coronary angiography revealed severe and diffuse 3-vessel coronary artery disease.
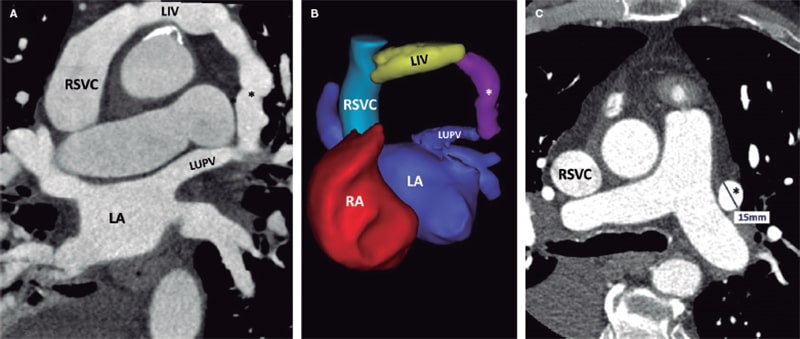
Figure 1. Preoperative thoracic computed tomography scan. Multiplanar reformatted (A) and 3D reconstructed (B) images reveal the presence of a left upper pulmonary vein (LUPV) with dual drainage into the left innominate vein through a vertical vein (*) and the left atrium (LA). The vertical vein (*) runs anteriorly to the left pulmonary artery (C). LIV, left innominate vein; RA, right atrium; RSVC, right superior vena cava.
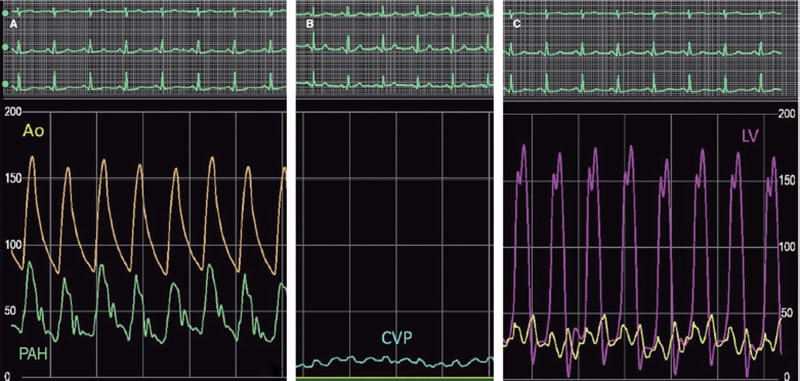
Figure 2. Baseline hemodynamic measurements showing pulmonary arterial hypertension (PAH) (A) and elevated left ventricular (LV) end-diastolic and left atrial pressures (C) exceeding central venous pressure (CVP) significantly (B). Ao, aorta.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
R. González-Manzanares, and G. Flores-Vergara drafted the manuscript, and completed the critical reviews. S. Ojeda, J. Suárez de Lezo, S. Espejo, and M. Pan reviewed and revised the manuscript and approved its final version before submission. All authors gave their final approval to the version that would eventually be published.
CONFLICTS OF INTEREST
S. Ojeda is an associate editor of REC: Interventional Cardiology. The journal’s editorial procedure to ensure impartial handling of the manuscript has been followed. The remaining authors declared no conflicts of interest relevant to the content of this article.
SUPPLEMENTARY DATA
Vídeo 1. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000302
* Corresponding author:
E-mail address: rafaelglezm@gmail.com (R. González-Manzanares).












