CASE RESOLUTION
The case was presented in the medical-surgical session and given the high risk involved the percutaneous closure of the pseudoaneurysm was decided.1-2
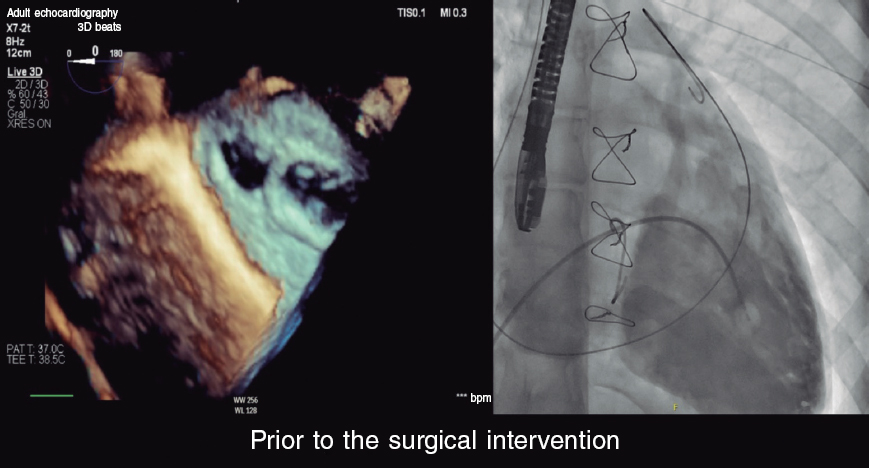
The procedure was performed under general anesthesia and guided by transesophageal echocardiography and fluoroscopic fusion imaging.
Since the patient carried a prosthetic mitral valve, a retrograde approach strategy was decided via right femoral arterial access (6-Fr).
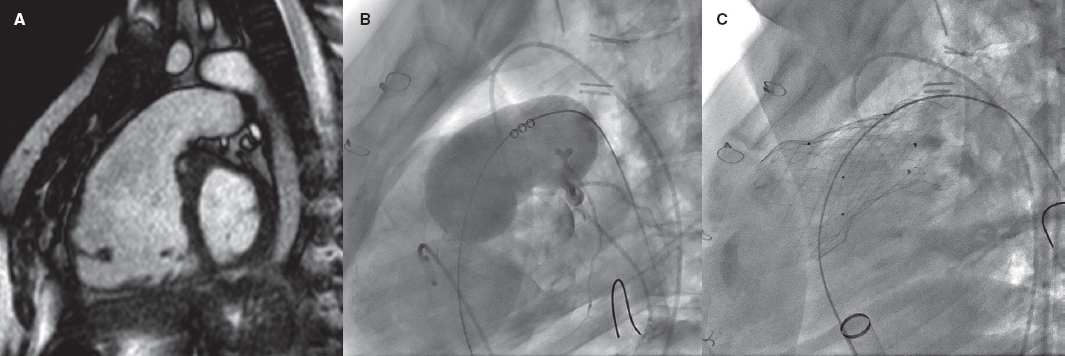
With help from an AL 1 catheter (Cordis Corporation, FL, United States) and a Terumo straight guidewire (Terumo Medical Corporation, NJ, United States), the native aortic valve was crossed, and the AL 1 catheter was advanced towards the left ventricle. A Pigtail catheter was used to perform a left ventriculography (Cordis Corporation, FL, United States) that revealed a cavity in relation to the left ventricle with the passing of contrast towards such cavity (video 1 of the supplementary data). After several attempts trying to place the catheter at the origin of the defect, the pseudoaneurysm cavity was finally crossed using a curved Terumo guidewire. At this point, the information provided by fluoroscopic fusion imaging was crucial because it revealed the origin of the defect and facilitated guidewire crossing towards the cavity (figure 1 and figure 2).

Figure 1. Location of the origin of pseudoaneurysm through fluoroscopic fusion imaging (red circumference).
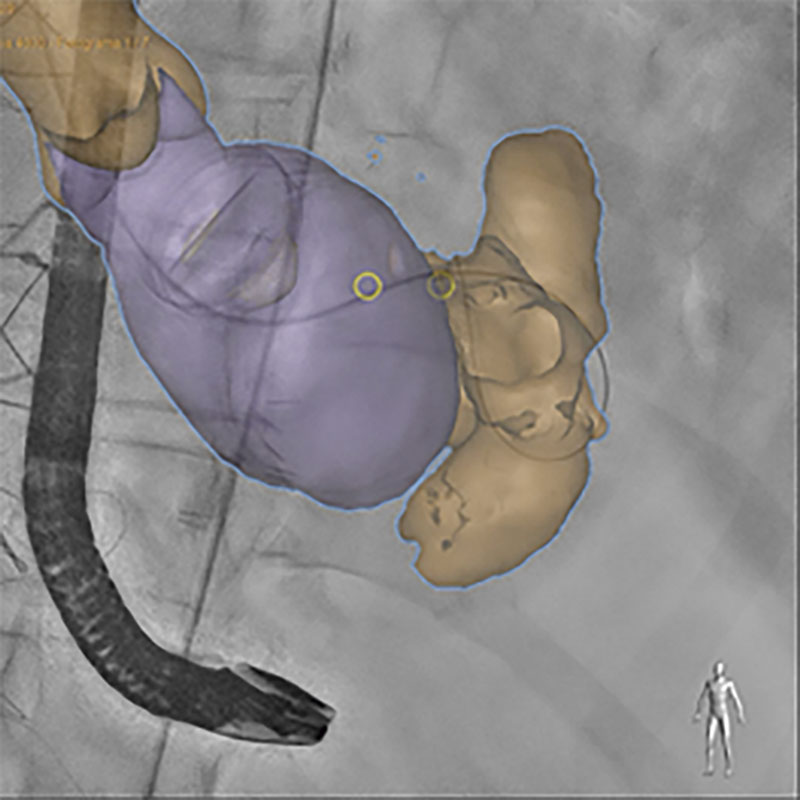
Figure 2. Fusion imaging (fluoroscopy, transesophageal echocardiography, and computed tomography) facilitating the location of the origin of the defect (yellow circumference).
The AL 1 catheter was exchanged for a 4-Fr straight tip catheter (Teleflex interventional, United States), and then for a XtraStiff guidewire (Cook Medical IN, United States) on which a 6-Fr delivery sheath was advanced (figure 3).

Figure 3. Delivery sheath. The Amplazter device can be seen in the distal border.
Selecting the right device was key for the procedure. Considering the anatomical characteristics of the defect and the risk of interference from the devices commonly used (Amplatzer Vascular Plug III or Amplatzer perimembranous ventricular septal defect occluder, AGA Medical Corporation, MN, United States) associated with the closure of this type of defects with the discs of the prosthetic mitral valve (due to the proximity of the defect to the prosthetic valve) a 12 mm Amplatzer Vascular Plug II device (AGA Medical Corporation, MN, United States) was used. Its proper positioning was confirmed with the distal disc of the device body inside the cavity while the proximal disc seals off the defect entry on the left ventricular lateral wall.2
After confirmation of proper stability, the device was released (figure 3). Control venticulography showed little passage of contrast towards the pseudoaneurysm cavity with significant reduction compared to the baseline ventriculography, and appearance of spontaneous echocardiographic contrast inside the cavity (figure 4) (video 2 of the supplementary data).
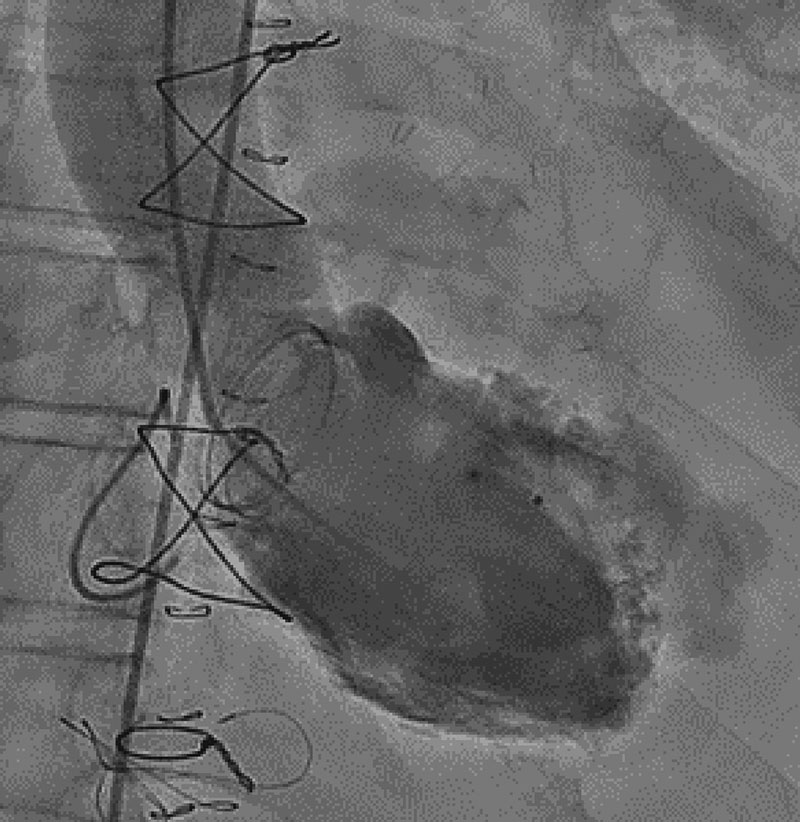
Figure 4. Left ventriculography showing the Amplatzer device in the left ventricular lateral wall with little passage of contrast towards the pseudoaneurysm (video 4 of the supplementary data).
The control transesophageal echocardiography revealed the presence of residual cranial leak with less systolic-diastolic flow compared to baseline levels, and appearance of spontaneous echocardiographic contrast inside the cavity (videos 3 and 4 of the supplementary data).
After the procedure, a control cardiac computed tomography confirmed that the Amplatzer device had been perfectly anchored to the left ventricular lateral wall and properly sealed off without any passage of contrast through it or cavity filling (figure 5).1
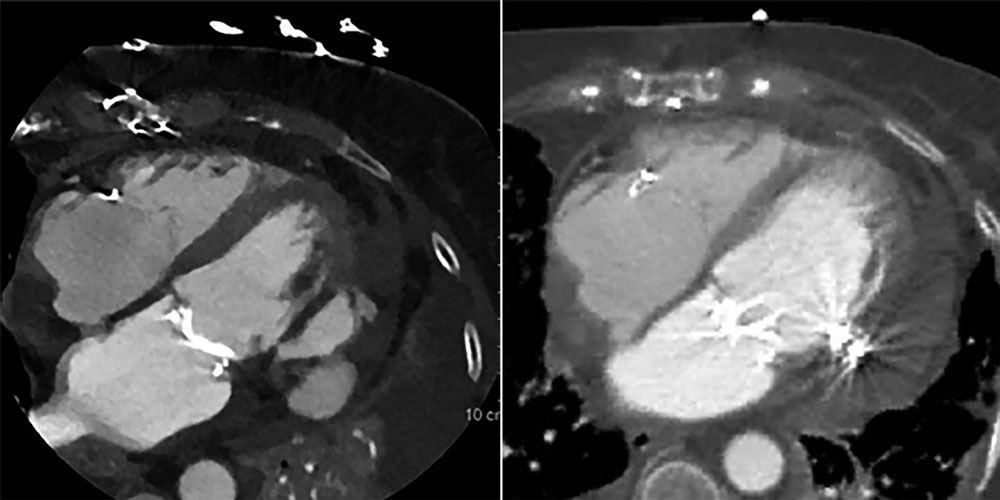
Figure 5. Left: image before the procedure (unsealed defect). Right: computed tomography imaging after Amplatzer device implantation.
However, 10 days after the percutaneous procedure, the patient died of multiorgan failure in a context of a septic shock.
The percutaneous closure of ventricular pseudoaneurysm can be a therapeutic option for patients ineligible for surgical correction.3 Fluoroscopic fusion imaging, and the 3D reconstruction of the defect were key to plan the procedure and select the most appropriate occluder device.
The patient’s written and verbal informed consents were obtained before publishing this case report.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
L. Gutiérrez Alonso drafted the manuscript and was directly involved in patient care. D. Arzamendi, X. Millán, L. Asmarats, and M. Torres were directly involved in patient care. D. Arzamendi supervised the draft of the manuscript. Chi Hion Li was directly involved in the case and provided the images.
CONFLICTS OF INTEREST
None whatsoever.
SUPPLEMENTARY DATA
Vídeo 1. Gutiérrez Alonso L. DOI: 10.24875/RECICE.M22000285
Vídeo 2. Gutiérrez Alonso L. DOI: 10.24875/RECICE.M22000285
Vídeo 3. Gutiérrez Alonso L. DOI: 10.24875/RECICE.M22000285
Vídeo 4. Gutiérrez Alonso L. DOI: 10.24875/RECICE.M22000285
REFERENCES
1. Vignati G, Bruschi G, Mauri L, et al. Percutaneous device closure of iatrogenic left ventricular wall pseudoaneurysm. Ann Thorac Surg. 2009;88:e31-33.
2. Dundon BK, Yeend RA, Worthley SG. Percutaneous closure of a large periprosthetic left ventricular pseudoaneurysm in a high-risk surgical candidate. Heart. 2008;94:1043.
3. Graham EM, Bandiso de VM, Atz AM, Kline CH, Taylor MH, Ikonomidis JS. Percutaneous occlusion of a pseudoaneurysm evolving after homograft aortic valve and root replacement with the Amplatzer muscular ventricular septal defect occluder. J Thorac Cardiovasc Surg. 2006;131:914-916.
* Corresponding author:
E-mail address: lolagutialonso@gmail.com (L. Gutiérrez Alonso).