CASE PRESENTATION
Hemoptysis is the subglottal expectoration of blood from the tracheobronchial tree. Most cases of massive hemoptysis originate at the bronchial arteries (90%) and often become complicated due to systemic arterial blood pressure. The mechanism of action is the rupture of hypervascularized reticulum and vascular dilatation as a response to the substances released in the inflammatory process. This clinical entity has elevated morbidity and mortality rates. Early diagnosis and the timely administration of therapy are of paramount importance.
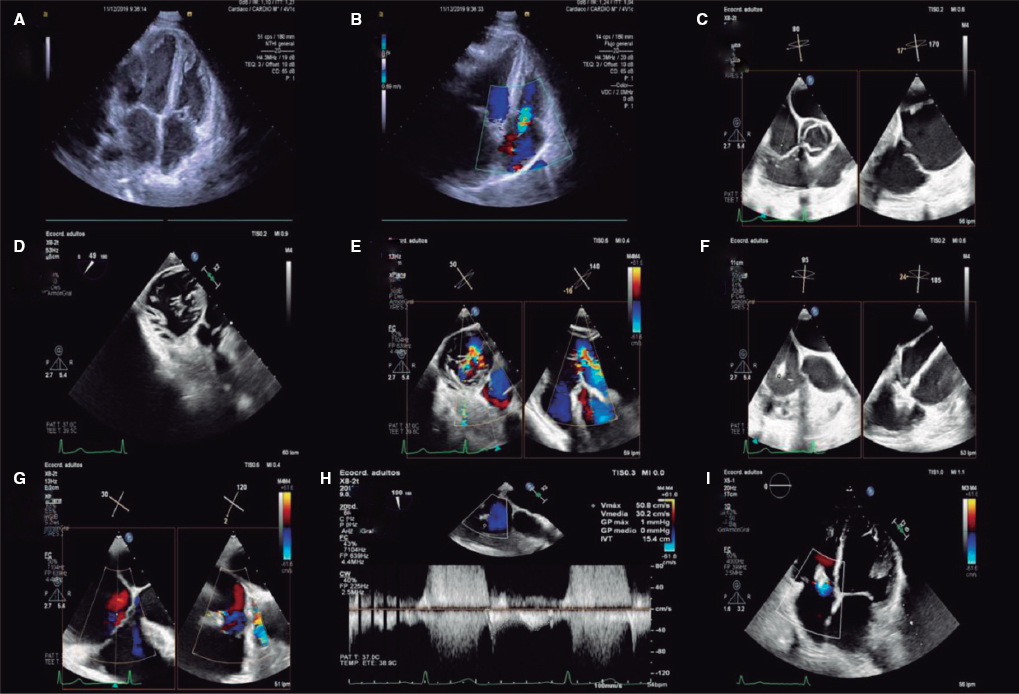
This is the case of a 73-year-old woman with a past medical history of breast cancer with ED presentation of early onset massive hemoptysis. She was admitted to the intensive care unit with a heart rate of 122 bpm, arterial blood pressure of 78/45 mmHg, and oxygen saturation of 82% with high-flow oxygen mask. Emergency orotracheal intubation and mechanical ventilation were decided. Given the patient’s hemodynamic instability, vasopressor drug infusion was started at increasing doses until a mean arterial blood pressure of 60 mmHg was reached with noradrenalin at 0.3 µg/kg/min. Lab test results showed hemoglobin levels of 7.5 g/dL, hematocrit of 21%, PaO2 of 62%, and hyperlactacidemia. A total of 2 bags of packed red blood cells were transfused, and the patient was transferred to the computed tomography scan room. The CT scan revealed the presence of a fistula from the left bronchial artery towards the upper branch of the left pulmonary artery with images consistent with alveolar hemorrhage compromising all lobes from both pulmonary fields (figure 1).
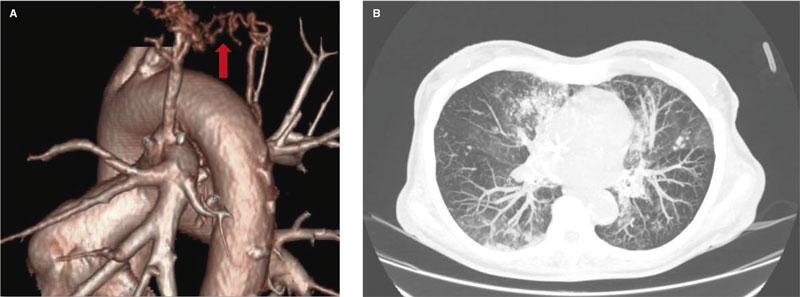
Figure 1. Computed tomography scan at admission. A: 3D reconstruction showing the arterio-arterial fistula from the pulmonary artery branch towards the bronchial artery. B: axial view showing an image consistent with bilateral alveolar bleeding.
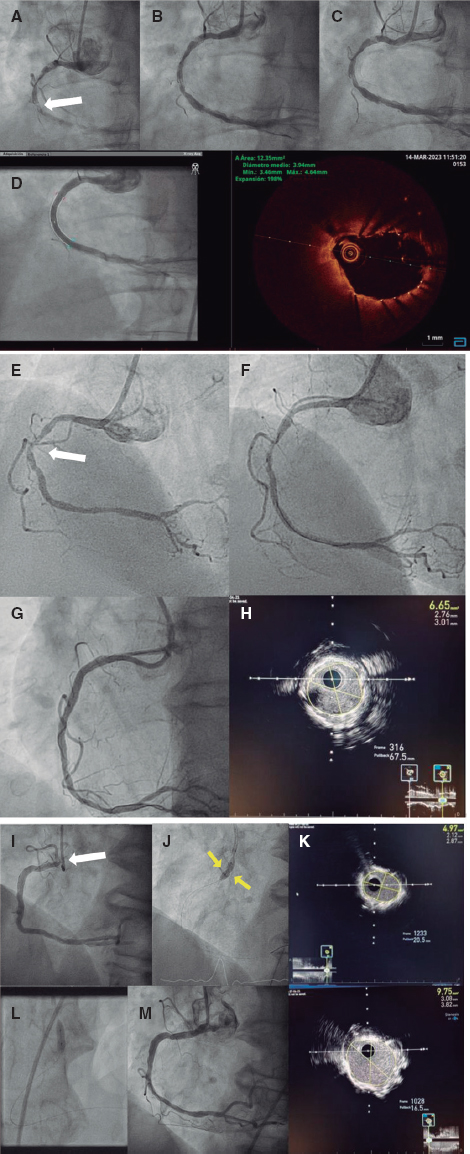
It also revealed the occupation of the left main bronchus and the lower and upper lobe branches with dense material suggestive of blood clots due to its high spontaneous density (figure 2). Given this clinical presentation and the features revealed by the CT scan, right bronchial selective intubation was decided. Afterwards, the patient was immediately transferred to the cath lab for endovascular embolization.
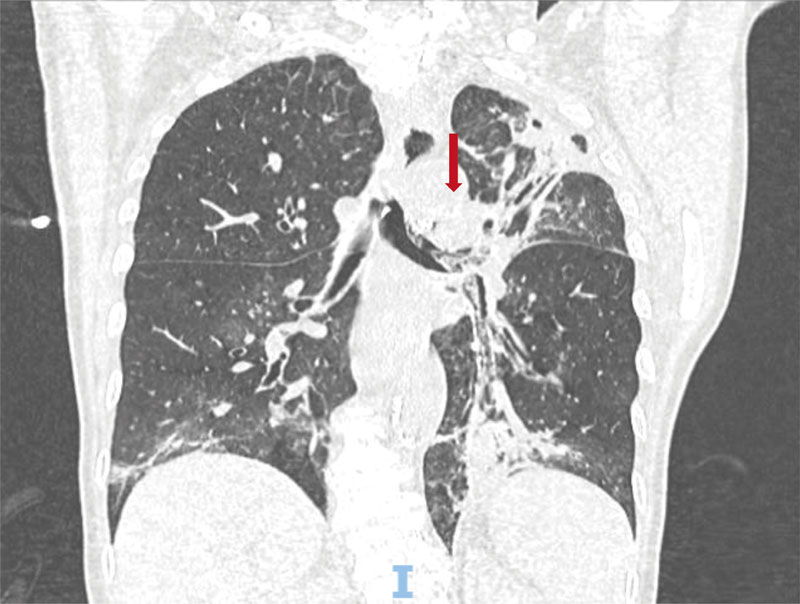
Figure 2. Computed tomography scan at admission. Coronal view showing the left main bronchus occupied by the blood clots.
The patient gave her informed consent for publication purposes.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
F. Liberman drafted and reviewed the manuscript. N. Zaderenko, J.P. Casas, and G. Pacheco treated the patient themselves, drafted and supervised the manuscript. J. Lugones also supervised the manuscript and provided the images.
CONFLICTS OF INTEREST
None reported.
* Corresponding author.
E-mail address: libermanfederico@gmail.com (F. Liberman).