CASE PRESENTATION
Premature baby born by emergency caesarian section after 27 + 5 weeks of pregnancy due to premature rupture of membranes and umbilical cord prolapse. The patient's body weight at birth was 990 grams. The prenatal ultrasounds performed all looked normal. The patient required intubation and mechanical ventilation on his 6th hour of life due to hyaline membrane disease.
After the 24th hour of life, the functional echocardiogram performed revealed the presence of a 2.4 mm ductus arteriosus with left-to-right shunt. It was decided to start an ibuprofen cycle for pharmacological closure. Pressure curve damping in the umbilical artery, arm-leg blood pressure gradient, and lack of femoral pulse palpation were seen after the first dose. After discussion with the heart team aortic the presence of coarctation was confirmed with distal arch hypoplasia, and a 1 mm ductus arteriosus. It was decided to start the IV infusion of prostaglandins. The patient was transferred to our center on his 59th hour of life.
Upon arrival, the patient showed an arm-leg blood pressure gradient of 40 mmHg, a pre- and post-ductal saturation of 11%, preserved diuresis, and low lactic acid levels. The echocardiography performed revealed the presence of a small aortic arch, isthmus with posterior indentation, and preductal coarctation images with a maximum gradient of 60 mmHg, and diastolic prolongation of forward flow (figure 1 and figure 2, video 1 of the supplementary data). Also, a large ductus arteriosus irrigating the downstream aorta with systolic right-to-left shunt and pulsatile flow in the abdominal aorta with dampened systolic component and abolished diastolic component.
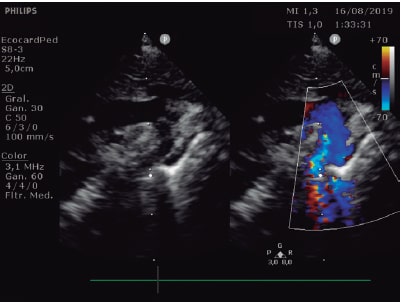
Figure 1. Small aortic arch and isthmus with posterior indentation.
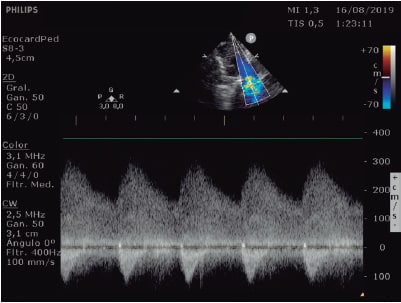
Figure 2. Continuous-wave Doppler echocardiography in the coarctation area with a maximum gradient of 60 mmHg and diastolic prolongation of forward flow.
During the first few days following admission, the patient remained hemodynamically stable with the infusion of prostaglandins at maintenance dose. Arterial hypertension progressively developed with systolic pressure numbers in the upper limbs in between 90 mmHg to 100 mmHg followed by dilatation, hypertrophy, and further left ventricular systolic dysfunction on the control echocardiograms, which required the infusion of urapidil and dobutamine on day 9.
The patient's clinical condition deteriorated on his 13th day of life and he required respiratory support with high-frequency ventilation and further support with dobutamine. The echocardiogram confirmed the progressive deterioration of the left ventricle (video 2 of the supplementary data) with severe systolic dysfunction, appearance of moderate mitral regurgitation, and accelerated flow through the foramen ovale, which facilitated the estimation of left atrial pressure somewhere around 23 mmHg.
Since the clinical situation is so serious, an emergency procedure is proposed, but the patient is a high-risk candidate for surgery due to his prematurity, low body weight (29 + 4 weeks of postmenstrual age and 1200 grams at that time), hemodynamic instability, and severe left ventricular dysfunction.
FUNDING
The work has been carried out without funding.
AUTHORS' CONTRIBUTIONS
D. Salas-Mera, and C. Abelleira Pardeiro have drafted and corrected the text of this article. Mr. Ortega Martínez, A. Hernández de Bonis, and F. Gómez Martín have participated in the patient' care and have supervised the text. F. Gutiérrez-Larraya Aguado has supervised the text and contributed to the bibliography.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Salas-Mera D. DOI: 10.24875/RECICE.M20000188
Vídeo 2. Salas-Mera D. DOI: 10.24875/RECICE.M20000188
Corresponding author: Servicio de Cardiología Pediátrica, Hospital Universitario La Paz, Paseo de la Castellana 261, 28046 Madrid, Spain.
E-mail address: diasalmer@gmail.com (D. Salas-Mera).












