To the Editor,
Aorto-atrial fistulas are an extremely rare condition where an abnormal connection forms between the aortic structures and the cardiac atria. Among them, fistulas between the aorta and the left atrium (Ao-LA) are particularly uncommon, and mainly associated with complications like infectious endocarditis, paravalvular abscesses, aortic dissections, and cardiac surgery often damaging the aortic valve or root.1 This is the case of a patient with a iatrogenic Ao-LA fistula successfully treated with a percutaneous Amplatzer device.
This is the case of an 82-year-old man admitted to the hospital due to acute heart failure. Three weeks earlier, he had undergone cardiac surgery with mitral and tricuspid valve repair through double annuloplasty plus left anterior descending coronary artery bypass with internal mammary artery graft.
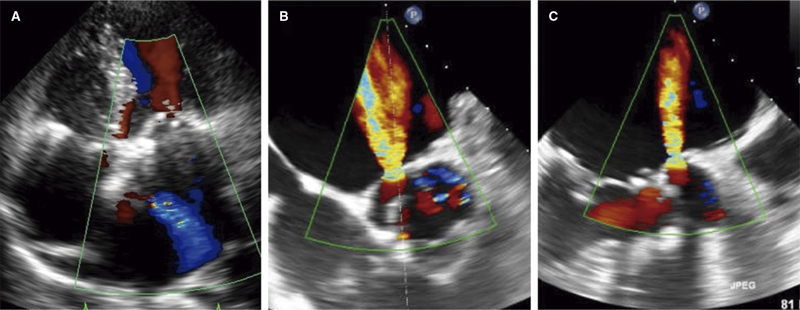
The transthoracic echocardiography revealed the presence of a preserved biventricular and valvular function, but also an abnormal systolic and diastolic jet in the left atrium (figure 1A and video 1 of the supplementary data). On the transoesophageal echocardiography this jet corresponded to an Ao-LA fistula through the aortic non-coronary sinus with a significant shunt across it (figure 1B,C and video 2 of the supplementary data). There were no images suggestive of infective endocarditis and repeated blood cultures remained negative for any bacterial growth. A computed tomography scan confirmed the findings, although mitral annuloplasty triggered metal artifacts, thus hindering 3D reconstruction. The individual was considered a high-risk patient for surgical reintervention by the heart team, and was initially treated with drugs. However, despite the optimal medical therapy he was readmitted twice within the following 3 months. Therefore, interventional management of the fistula was decided. The patient gave his written informed consent.
Figure 1. Transthoracic (A) and transoesophageal echocardiography (B, C) showing a high-velocity jet shunting from the non-coronary sinus of Valsalva towards the left atrium.
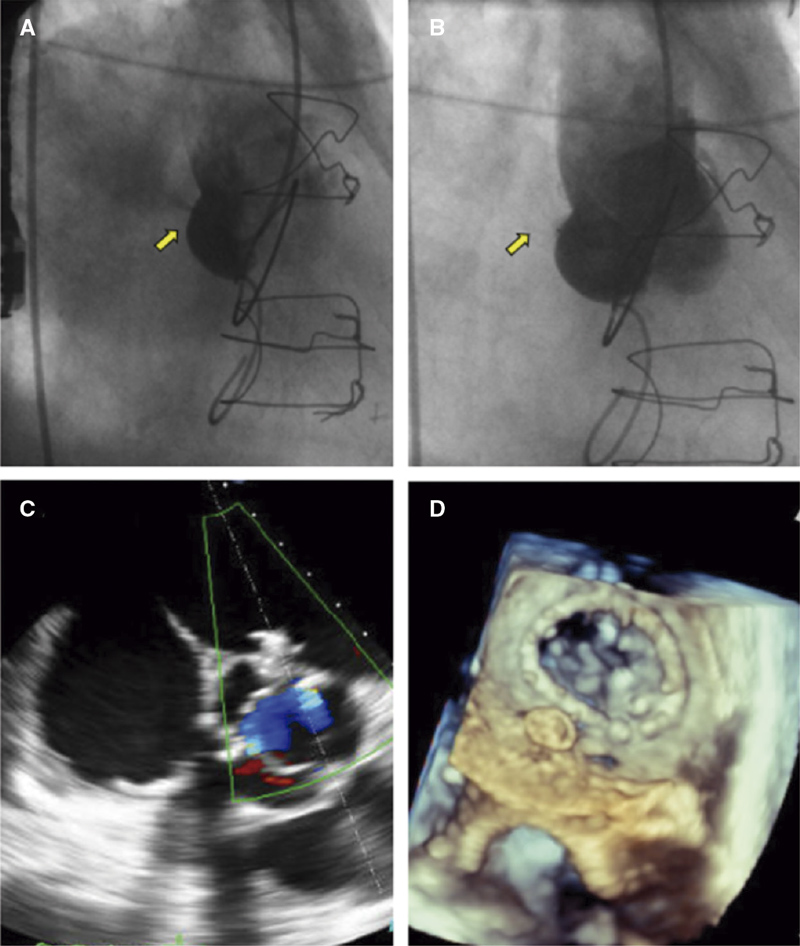
A percutaneous approach was attempted under general anaesthesia using retrograde access via right femoral artery. The initial angiography performed using a 6-Fr right Judkins(Medtronic, United States) guiding catheter showed a large flow of contrast from the non-coronary sinus to the left atrium (figure 2A and video 3 of the supplementary data). Afterwards, a Sion Blue (Asahi Intecc, Thailand) wire was placed into the left atrium and the right Judkins guiding catheter advanced into the atrium to be used as a delivery system. A 6 mm Amplatzer DuctOccluder II(Abbott, United States) was successfully deployed with simultaneous angiographic (figure 2B and video 4 of the supplementary data) and transoesophageal echocardiography (figure 2C,D and videos 5 and 6 of the supplementary data) confirmation of almost complete fistula closure. Although the patient was previously on anticoagulant therapy due to permanent atrial fibrillation, empirical combination therapy adding aspirin 100 mg was prescribed for 6 months. The 6-month follow-up was uneventful, and the patient remained in functional class I with no residual shunt on the 2D echocardiography performed at 1 month.
Figure 2. A: Basal aortography with left atrium filling through the fistula (arrow).D: No contrast passage after Amplatzer Duct Occluder II deployment (arrow).E, F: Amplatzer device positioned with no shunt on the color Doppler ultrasound and 3D transoesophageal echocardiography view.
Aorta-atrial fistulas are a rare condition being cardiac surgery a recognized cause.1 Among them, fistulas between the Ao-LA are very unusual, and occurrence is much more common after aortic compared to coronary artery bypass graft surgery. To this date, no cases have ever been associated with mitral valve repairs.1 The abnormal flow between the aorta and the left atrium often leads to volume overload and signs and symptoms of heart failure.2 Early recognition and diagnosis of this severe condition relies on its echocardiographic characterization being the transoesophageal echocardiography the imaging modality of choice regarding diagnosis. Combination with 3D imaging modalities is highly advised, when available either transoesophageal echocardiography or computed tomography scan as they allow spatial orientation and high anatomical definition for procedural planning.3 Evaluation can also include cardiac magnetic resonance imaging or cardiac catheterization to additionally assess shunt quantification.4
Due to the low incidence rate of aorto-atrial fistulas, treatment strategies depend on the underlying disease, and interventions are based on expert opinions and consensus among the treating physicians. Nevertheless, closure of the fistula is highly advised in symptomatic patients.5 Although surgery is the standard treatment, percutaneous closure can be considered in high-risks patients with favorable angiographic characteristics like location in the non-coronary sinus or fistulas of small diameters.1 In the absence of specific percutaneous material, the off-label use of an Amplatzer DuctOccluder II device with simultaneous echocardiographic and fluoroscopy guidance is an amenable option as described in our case and isolated cases in the medical literature available.6,7 Further antiplatelet/anticoagulant therapy after device implantation is advised although evidence regarding the optimal antithrombotic regimen and duration remains empirical.
In conclusion, although rare, aorto-atrial fistulas are a severe complication that can led to refractory heart failure. Closure of the fistulous tract is often advised. Evidence on this regard is scarce and mostly based on case reports or case series.2,6 More data is needed to better define optimal therapeutic strategies in this scenario.
Funding
M. Tamargo was partially supported by grants from Fundación para la Investigación Biomédica Gregorio Marañón, Madrid, Spain, and CM20/00054 from Instituto de Salud Carlos III, Madrid, Spain.
Authors’ contributions
All the authors contributed equally to this work.
Conflicts of interest
None whatsoever.
SUPPLEMENTARY DATA
Vídeo 1. Tamargo M. DOI: 10.24875/RECICE.M23000387
Vídeo 2. Tamargo M. DOI: 10.24875/RECICE.M23000387
Vídeo 3. Tamargo M. DOI: 10.24875/RECICE.M23000387
Vídeo 4. Tamargo M. DOI: 10.24875/RECICE.M23000387
Vídeo 5. Tamargo M. DOI: 10.24875/RECICE.M23000387
Vídeo 6. Tamargo M. DOI: 10.24875/RECICE.M23000387
REFERENCES
1. Fierro EA, Sikachi RR, Agrawal A, Verma I, Ojrzanowski M, Sahni S. Aorto-Atrial Fistulas: A Contemporary Review. Cardiol Rev. 2018;26:137-144.
2. Foster TJ, Amin AH, Busu T, et al. Aorto-cardiac fistula etiology, presentation, and management: A systematic review. Heart Lung. 2020;49:317-323.
3. Patel V, Fountain A, Guglin M, Nanda NC. Three-Dimensional Transthoracic Echocardiography in Identification of Aorto-Right Atrial Fistula and Aorto-Right Ventricular Fistulas. Echocardiography. 2010;27:E105-E108.
4. Valsangiacomo Buechel ER, Grosse-Wortmann L, Fratz S, et al. Indications for cardiovascular magnetic resonance in children with congenital and acquired heart disease: an expert consensus paper of the Imaging Working Group of the AEPC and the Cardiovascular Magnetic Resonance Section of the EACVI. Eur Heart J Cardiovasc Imaging. 2015;16:281-297.
5. Jainandunsing JS, Linnemann R, Maessen J, et al. Aorto-atrial fistula formation and therapy. J Thorac Dis. 2019;11:1016-1021.
6. Alkhouli M, Almustafa A, Kawsara A, et al. Transcatheter closure of an aortoatrial fistula following a surgical aortic valve replacement. J Card Surg. 2017;32:186-189.
7. Hernández García JM, Alonso-Briales JH, Jiménez-Navarro MF, Cabrera-Bueno F, González-Cocina E, Such-Martínez M. Transcatheter Closure of Aorto-Left Atrial Fistula Using an Amplatzer Device. Rev Esp Cardiol. 2005;58:1121-1123.