To the Editor,
Acute SARS-CoV-2 infections (COVID-19) have caused a global pandemic since the first cases were described in Wuhan, China, back in December 2019. The first wave of COVID-19 cases in Western Europe led to substantial healthcare disruption and population lockdowns from March 2020 through May 2020. Regarding the cardiovascular implications, COVID-19 has been associated with higher in-hospital mortality rates in patients with coronary syndromes.1 Among others, a higher thrombogenic risk has been proposed as the underlying mechanism of this increased rate of adverse events.2 Subsequently, observational studies have suggested an increased number of stent thrombosis during acute COVID-19 infections.3 The underlying mechanisms of this stent thrombosis are endotheliitis, platelet activation, and coagulopathy. It is unknown whether these mechanisms could also lead to late adverse cardiovascular events or stent failure.
We previously reported on an increased 30-day mortality rate in patients with acute coronary syndrome and COVID-19 compared to non-COVID-19 patients.4 Later studies confirmed similar rates of death after myocardial infarction.5
This study aimed to analyze the 1-year rate of adverse cardiovascular events and stent failure in consecutive patients referred for coronary angiography from March through April 2020. All the participant patients gave their informed consent and the project was approved by the local ethics committee.
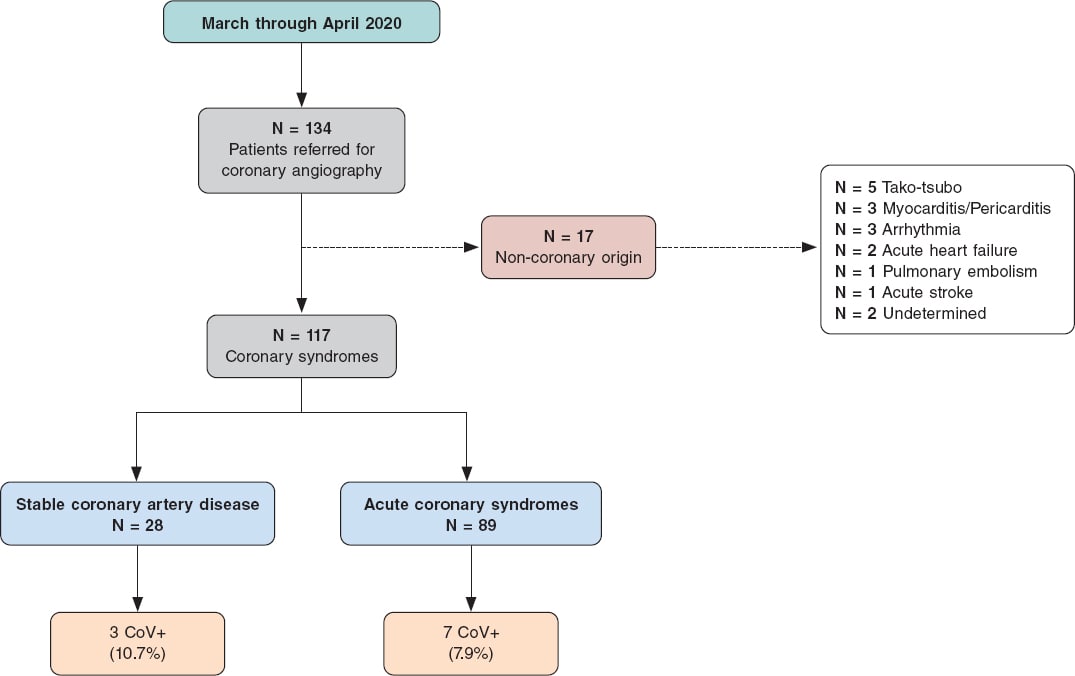
Out of a total of 134 patients, 117 had coronary artery disease (either acute coronary syndrome or stable coronary artery disease). Patients (n = 17) with alternative diagnoses (MINOCA, tako-tsubo, myocarditis, others) were excluded. A total of 10 (8.5%) of these 117 patients tested positive on the polymerase chain reaction (PCR) test for SARS-CoV-2 (CoV+) while the PCR of 107 patients tested negative or were never tested due to the lack of clinical data suggestive of acute COVID-19 (universal testing for COVID-19 was unavailable at this early stage of the pandemic). The primary event was a patient-oriented combined endpoint (POCE) of all-cause mortality, any myocardial infarctions or any revascularizations. The device-oriented composite endpoint (DOCE) was defined as a composite of cardiac death, target vessel revascularization or stent thrombosis. Both the patient selection and the study flowchart are shown on figure 1.
Figure 1. Study flowchart.
The baseline and clinical characteristics of both CoV- and CoV+ patients are shown on table 1. Patients who were CoV+ had been revascularized slightly less frequently (60.0% vs 74.7%). Also, complete revascularization was less likely (30.0% vs 56.2%) although both were non-significant differences (P = .312, and P = .183, respectively).
Table 1. Clinical characteristics and angiographic findings
| CoV– | CoV+ | P | |
|---|---|---|---|
| N | 107 | 10 | |
| Age (years) | 64.8 (16.9) | 66.8 (25.0) | .730 |
| Female sex | 30 (28.04) | 2 (20.0) | .726 |
| Hypertension | 72 (69.23) | 7 (70.0) | .721 |
| Hyperlipidemia | 58 (55.24) | 4 (44.0) | .533 |
| Diabetes | 33 (31.43) | 2 (20.0) | .719 |
| Tobacco use (former or active smoker) | 54 (51.43) | 6 (60.0) | .496 |
| Chronic kidney disease | 17 (16.5) | 1 (10.0) | 1.000 |
| LVEF | 52.2 (12.5) | 48.8 (19.3) | .611 |
| Clinical presentation | .701 | ||
| SA/UA | 25 (23.36) | 3 (30.0) | |
| MI (STEMI, NSTEMI) | 82 (76.64) | 7 (70.0) | |
| Vessels with > 70 stenosis | .549 | ||
| 0 | 19 (17.76) | 1 (10.0) | |
| 1 | 48 (44.86) | 3 (30.0) | |
| 2 | 22 (20.56) | 3 (30.0) | |
| 3 | 18 (16.82) | 3 (30.0) | |
| Left main coronary artery disease | 5 (4.67) | 2 (20.0) | .110 |
| Revascularization | .312 | ||
| No | 27 (25.23) | 4 (40.0) | |
| PCI | 73 (68.22) | 5 (50.0) | |
| CABG | 7 (6.54) | 1 (10.0) | |
| Complete revascularization | 59 (56.19) | 3 (30.0) | .183 |
| PCI patients (n) | 73 | 5 | |
| Stent implantation | 66 (90.4) | 5 (100) | .438 |
| Procedural success | 69 (94.5) | 5 (100) | .548 |
| Successfully treated lesions | .602 | ||
| 0 | 4 (5.5) | 1 (20.0) | |
| 1 | 52 (71.2) | 3 (60.0 | |
| 2 | 13 (17.8) | 1 (20.0) | |
| 3 | 4 (5.5) | 0 (0) | |
| Procedural time (min) | 63.5 (44.3) | 55.56 (32.0) | .599 |
| Fluoroscopy time (min) | 13.2 (10.7) | 10.8 (7.1) | .502 |
| Contrast volume (ml) | 136.3 (77.5) | 148.8 (120.5) | .681 |
|
CABG, coronary artery bypass graft; LVEF, left ventricular ejection fraction; NSTEMI, non-ST-elevation acute myocardial infarction; PCI, percutaneous coronary intervention; SA, stable angina; STEMI, ST-segment elevation myocardial infarction; UA, unstable angina. Data are expressed as mean (± standard deviation) or no. (%) for categorical variables. |
|||
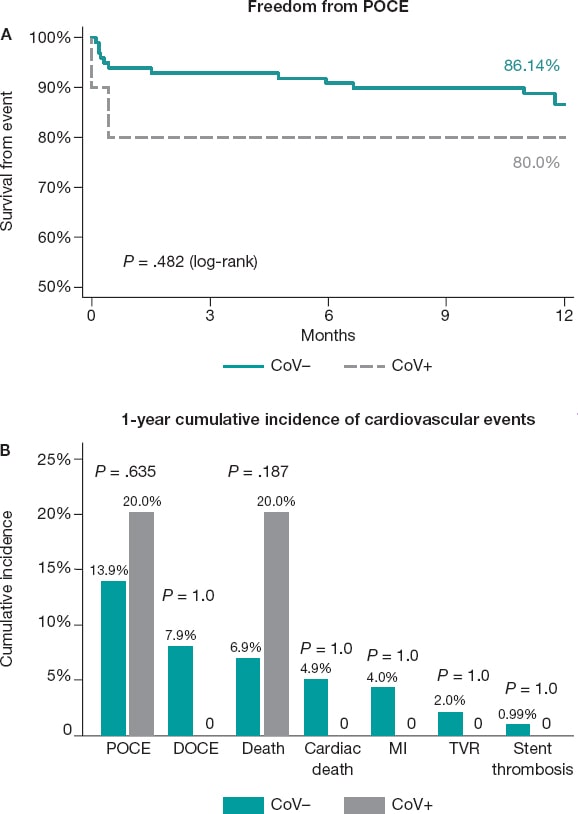
At the 1-year follow-up, the rate of MACE was similar in CoV+ and CoV- patients (20.0% vs 13.9%, respectively, P = .635) as shown on figure 2A. Two deaths were reported among CoV+ individuals (20.0% vs 6.9% in CoV-). These deaths occurred shortly after performing a coronary angiography due to COVID-19-related severe respiratory failure. Interesting enough, none of the other CoV+ patients experienced any adverse cardiovascular events at the 1-year follow-up (figure 2B). Among stent-revascularized patients (5 in the CoV+ group; 573 in the CoV- group, the rate of DOCE was 0%, and 10.0%, respectively). One stent thrombosis was reported in the CoV- group, and neither definitive nor suspected thrombosis were reported in CoV+ patients who underwent stent implantation.
Figure 2. A: Kaplan-Meier survival curves of the patient-oriented composite endpoint for CoV- and CoV+ patients. B: cumulative incidence at the 1-year follow-up of patient-oriented and device-oriented composite endpoints and their components in both CoV– and CoV+ patients. DOCE, device-oriented composite endpoint; MI, myocardial infarction; POCE, patient-oriented composite endpoint; TVR, target vessel revascularization.
Although these results should be interpreted while understanding the inherent biases of observational reports, this small series suggests that CoV+ patients may be at a higher risk of death, but not precisely at a higher risk of cardiovascular events. We did not find a significant or numerical trend towards more myocardial infarctions, target vessel failures or stent thromboses. The low rate of adverse cardiovascular events reported in our cohort of CoV+ patients suggests that, in clinically indicated cases, the invasive management of coronary artery disease should not be different from that of non-COVID-19 patients. We acknowledge the limitation of the small number of patients. However, as far as we know, this is the first series to report on the 1-year outcomes of coronary syndromes treated during the COVID-19 pandemic. Certain rare events such as stent thrombosis may need a much larger series to be properly examined, but conversely, the global pandemic may have led to an unsought positive publication bias of COVID-19-related complications. The reporting of consecutive patient data like our cohort, rather than selected case series, will refine our knowledge on the actual cardiovascular outcomes in patients recovered from COVID-19.
We conclude that the invasive management of coronary artery disease in COVID-19 positive patients did not convey a higher risk of adverse events at the 1-year follow-up. Therefore, management should not be different when dealing with acute SARS-CoV-2 infections.
FUNDING
No financial conflicts of interest have been disclosed regarding this study.
AUTHORS’ CONTRIBUTIONS
A. Travieso: manuscript writing, data curation, data analysis, and project design. C. E. Vergara-Uzcategui: data curation, and manuscript corrections. I. J. Núñez-Gil: data curation, and manuscript corrections. A. Fernández-Ortiz: project organization, and manuscript corrections. P. Salinas: manuscript writing, data curation, project design, and study direction.
CONFLICTS OF INTEREST
None.
REFERENCES
1. Rodriguez-Leor O, Cid-Alvarez B, de Prado AP, et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16:1426–1433.
2. Ranucci M, Ballotta A, Di Dedda U, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020;18:1747–1751.
3. Prieto-Lobato A, Ramos-Martínez R, Vallejo-Calcerrada N, Corbí-Pascual M, Córdoba-Soriano JG. A Case Series of Stent Thrombosis During the COVID-19 Pandemic. JACC Case Reports. 2020;2:1291–1296.
4. Salinas P, Travieso A, Vergara-Uzcategui C, et al. Clinical profile and 30-day mortality of invasively managed patients with suspected acute coronary syndrome during the COVID-19 outbreak. Int Heart J. 2021;62:274–281.
5. Kite TA, Ludman PF, Gale CP, et al. International Prospective Registry of Acute Coronary Syndromes in Patients With COVID-19. J Am Coll Cardiol. 2021;77:2466–2476.