To the Editor,
The management of chronic total coronary occlusions (CTO) has improved significantly over the last decade and reached success rates close to 85%-90% in contemporary registries.1 However, angiographically severe coronary calcifications are a common limitation of CTOs making revascularization more difficult.2
Intracoronary lithotripsy seems to be a safe and effective alternative for the management of severely calcified coronary lesions through the administration of pulsatile mechanical energy. This energy generates a pressure high enough to crack the intimal and medial calcium while minimizing mechanical damage to the remaining vascular tissues.3
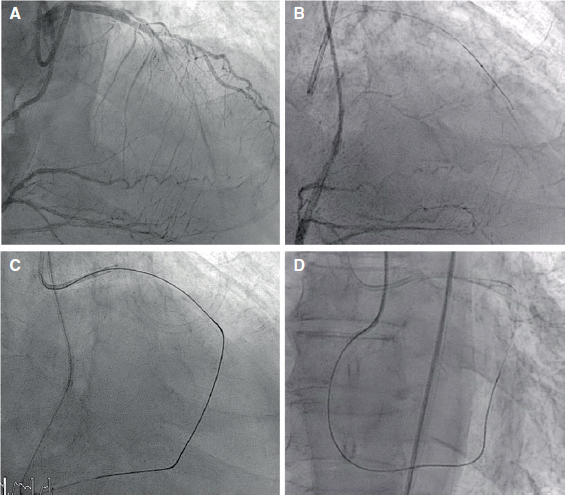
We present the case of a 77 year-old-male with a CTO in the mid left anterior descending coronary artery who underwent elective percutaneous coronary intervention. The distal left anterior descending coronary artery received retrograde flow through the septal collaterals from the right coronary artery (figure 1A).
Figure 1. A: chronic total coronary occlusion of the mid left anterior descending coronary artery. B: failed initial antegrade approach with subintimal progression of the guidewire. C: impossibility to advance the microcatheter retrogradely through the occlusion. D: creation of the arterioarterial loop using a RG3 guidewire in a second retrograde attempt.
The initial antegrade approach with guidewire escalation using the Sion (Asahi-Intecc, Abbott Vascular, United States), Gaia-Second (Asahi-Intecc, Abbott Vascular), and Progress-200T (Abbott Vascular) guidewires failed with progression through the subintimal space (figure 1B). Then the retrograde access was used. It facilitated the advance of a Fielder XT-R guidewire (Asahi-Intecc, Abbott Vascular) towards the proximal left anterior descending coronary artery and re-entry into the antegrade guide catheter. However, it was impossible to advance the Corsair-Pro (Asahi-Intecc, Abbott Vascular) and Turnpike (Teleflex, United States) microcatheters through the occlusion distal stump due to the heavy calcification at that point despite the balloon trapping of the retrograde guidewire into the guide catheter (figure 1C), so a second procedure was attempted 1 week later. This time the Corsair-Pro microcatheter was easily advanced using the retrograde access and the arterioarterial loop was completed using the RG-3 (Asahi-Intecc, Abbot Vascular) guidewire as shown on figure 1D.
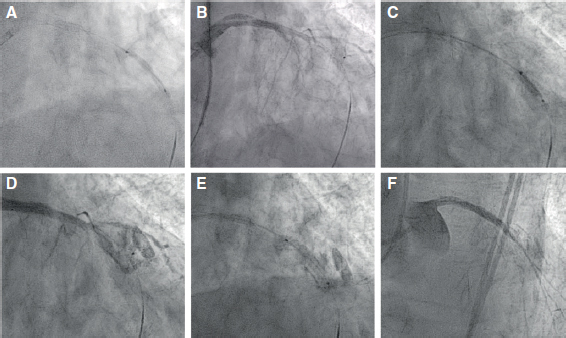
Then, the CTO was predilated using 2.0 mm and 2.5 mm semicompliant balloons (figure 2A,B) that were properly expanded. Considering the heavy coronary calcification and the previous difficulties, it was decided to perform an adjuvant intracoronary lithotripsy as the next step to crack the calcified plaque. In the procedure, non-compliant balloons were not used.
Figure 2. A: predilatation of the chronic total coronary occlusion using a 2.5 mm semicompliant balloon that proved ineffective (B). After the inflation of the Shockwave balloon in the mid left anterior descending coronary artery and the administration of the lithotripsy (C) an Ellis type III coronary perforation occurred (D) that was sealed using a Papyrus covered coronary stent (E). F: final result with flow restoration up to the level of the occlusion.
A 2.5/12 mm Shockwave lithotripsy balloon (Shockwave-Medical, United States) was advanced towards the mid left anterior descending coronary artery. After the balloon was inflated at a low pressure of 4 atm, 2 series of 10 acoustic shock waves were applied (figure 2C) with postdilatation at 6 atm following the technical specifications. The subsequent angiographic injection revealed the presence of an Ellis type III coronary perforation (figure 2D) that was controlled by implanting a 3.0/22 mm Papyrus covered coronary stent (Biotronik, Switzerland) (figure 2E), and a 3.0/22mm Onyx drug-eluting stent (Medtronic, United States) proximally overlapped. However, this did not restore flow to the distal left anterior descending coronary artery (figure 2F).
Intracoronary lithotripsy is an attractive therapeutic alternative for the management of severely calcified coronary lesions. It has been used in isolated cases of CTO,4,5 but for the time being there are no solid clinical data supporting its efficacy and safety in this specific context. However, this technique may be associated to potentially serious complications like coronary perforations and deep dissections6 reported in up to 13% of the vessels treated with lithotripsy at the optical coherence tomography assessment.7
In our patient the guidewire possibly advanced through the true lumen in the first retrograde attempt and the severe calcification of the CTO prevented the advance of the catheter. In the second attempt, the easier and less difficult advance of the microcatheter was possibly associated with the subintimal progression of the guidewire with posterior re-entry into the true lumen that facilitated the completion of the arterioarterial loop. Although no intracoronary imaging modality was performed for confirmation purposes, inflating the lithotripsy balloon and delivering of high-pressure pulsatile energy in the subintimal plane may have caused the tear of the coronary adventitia.
This case is indicative of the need to be more thorough in the assessment of the safety of coronary lithotripsy in the management of CTOs. From our standpoint, it is important to confirm the intraluminal position of the guidewire before using this technology, especially in complex lesions like CTOs. Hence, we think it is advisable to guide the application of intracoronary lithotripsy with intracoronary imaging modalities if feasible.
REFERENCES
1. Amat-Santos IJ, Martin-Yuste V, Fernández-Díaz JA, et al. Procedural, Functional and Prognostic Outcomes Following Recanalization of Coronary Chronic Total Occlusions. Results of the Iberian Registry. Rev Esp Cardiol. 2019;72:373-382.
2. Galeote G, Hernández H, Codón JC, et al. Índice de calcificación coronaria en la tomografía computarizada para predecir la necesidad de aterectomía rotacional. REC Interv Cardiol. 2019;1:167-174.
3. Ali ZA, Nef H, Escaned J, et al. Safety and Effectiveness of Coronary Intravascular Lithotripsy for Treatment of Severely Calcified Coro-nary Stenoses:The Disrupt CAD II Study. Circ Cardiovasc Interv. 2019;12:e008434.
4. Azzalini L, Bellini B, Montorfano M, Carlino M. Intravascular litho-tripsy in chronic total occlusion percutaneous coronary intervention. EuroIntervention. 2019;15:e1025-e1026.
5. Yeoh J, Hill J, Spratt JC. Intravascular lithotripsy assisted chronic total occlusion revascularization with reverse controlled antegrade retrograde tracking. Catheter Cardiovasc Interv. 2019;93:1295-1297.
6. López-Lluva MT, Jurado-Román A, Sánchez-Pérez, et al. Shockwave:Useful But Potentially Dangerous. JACC Cardiovasc Interv. 2019;12:500-501.
7. Ali ZA, Brinton TJ, Hill JM, et al. Optical Coherence Tomography Characterization of Coronary Lithoplasty for Treatment of Calcified Lesions:First Description. JACC Cardiovasc Imaging. 2017;10:897-906.
Corresponding author: Departamento de Cardiología, Hospital Clínico Universitario de Salamanca, Paseo San Vicente 182, 37007 Salamanca, Spain.
E-mail address: , (B. Trejo-Velasco).