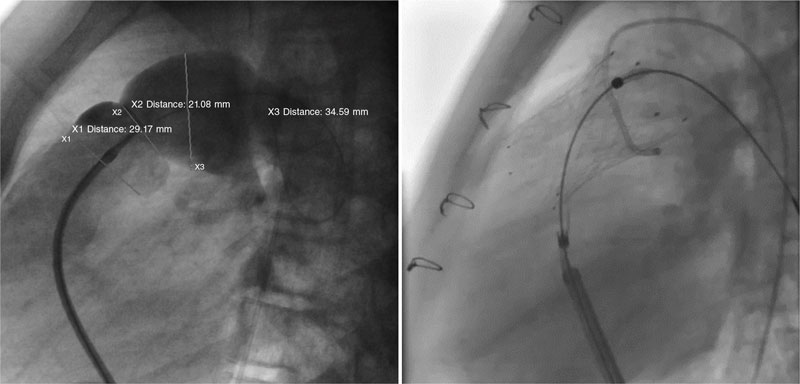
This is the case of 13-year-old teenage girl diagnosed with pulmonary atresia with intact ventricular septum treated in the neonatal period with valvulotomy with radiofrequency and percutaneous pulmonary valvuloplasty. Since then, the patient has developed severe pulmonary regurgitation and moderate tricuspid regurgitation. Valve implantation into the right ventricular outflow tract (RVOT) is decided due to worsening functional class with restrictive behavior of the right ventricle (without anticipated dilatation), and hepatic congestion. Cardiac catheterization reveals the presence of a dilated and pulsatile (pulmonary annulus: 29 mm) RVOT with supravalvular stenosis (minimum diameter: 21 mm), and a 34 mm post-stenotic dilatation (figure 1). A second-staged stent is implanted for percutaneous valve implantation. Given the absence of specific material for RVOTs so dilated, a 30 mm x 40 mm self-expandable Sinus-XL stent (Optimed, Germany) (off-label) is selected for being long enough, easy to implant, having enough navigability for the patient’s age (10-Fr sheath), and requiring less radial strength (favorable for dilated RVOTs).
Figure 1.
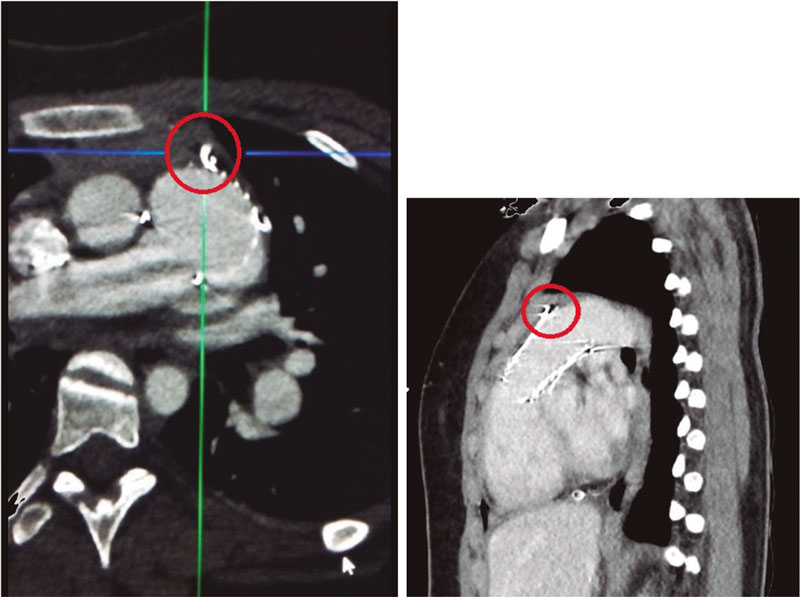
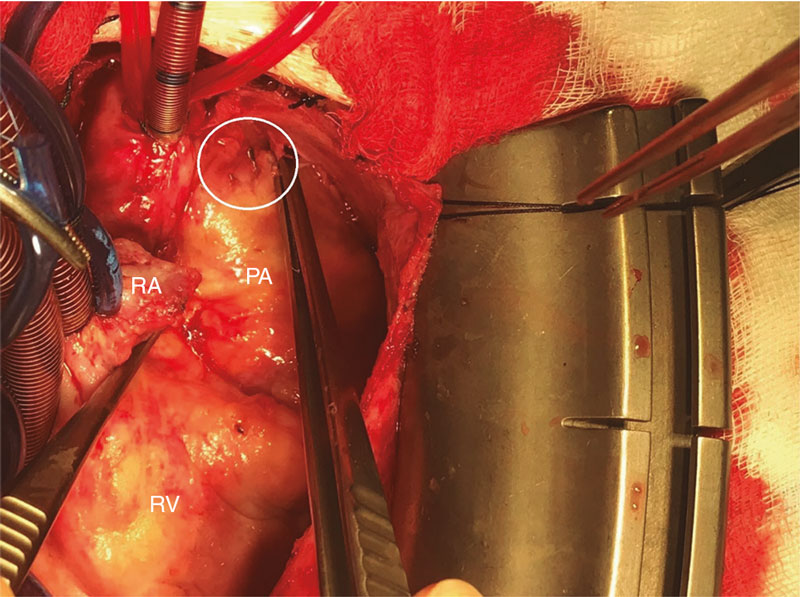
A 14-Fr sheath was used to perform position angiographies (figure 1). A few hours later, the patient showed hemodynamic instability with transthoracic echocardiography findings compatible with cardiac tamponade. An emergency computed tomography scan (figure 2) confirmed the perforation of the pulmonary trunk at the operating room (figure 3; RA, right atrium; PA, pulmonary artery; RV, right ventricle). The stent was removed, and a pulmonary valve was implanted with favorable progression.
Figure 2.
Figure 3.
The design of the stent is similar to that used during hybrid procedures in certain neonatal heart diseases, which means that similar complications can be expected.
The patient’s parents’ informed consent was obtained to be able to publish her case.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
A. Rasines Rodríguez: drafted the case. C. Abelleira Pardeiro: critical review and image selection. Direct patient care. E.J. Balbacid Domingo: critical review and image selection. Direct patient care. All authors: contributed to the study idea and design, data curation or its analysis and interpretation and final approval of the version that would eventually be published.
CONFLICTS OF INTEREST
None reported.