This is the case of a 34-year-old woman treated percutaneously for aortic coarctation repair. The patient’s past medical history included muscular ventricular septal defects with spontaneous closure, bicuspid aortic valve with asymptomatic moderate regurgitation with normal ventricular volume and function, and juxtaductal coarctation of the aorta treated with patch aortoplasty at 2 months old.
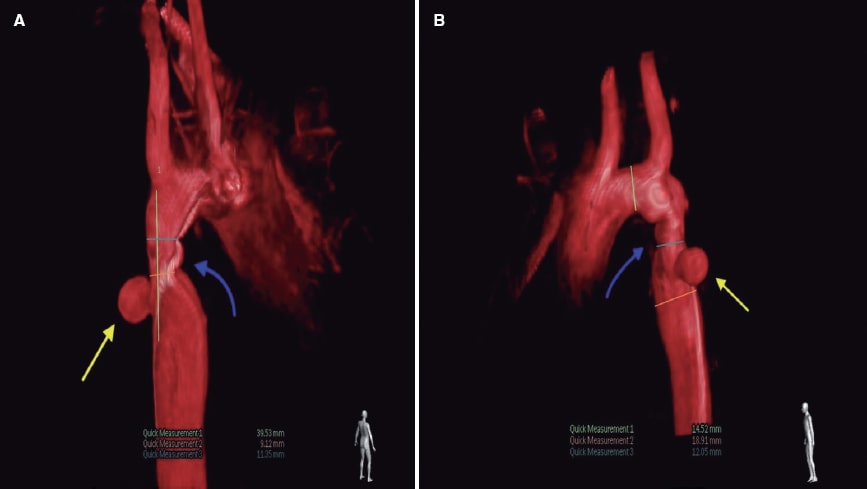
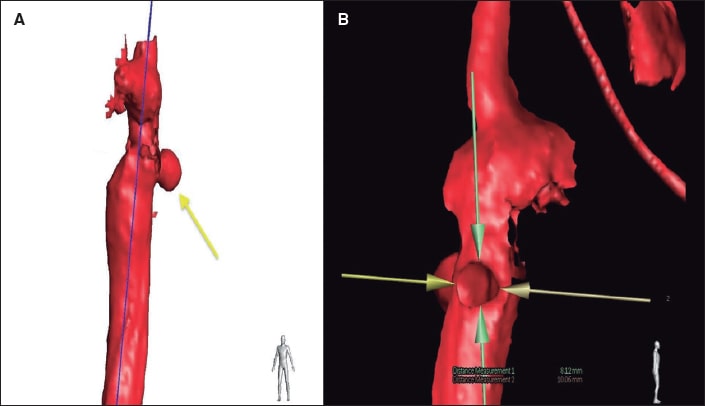
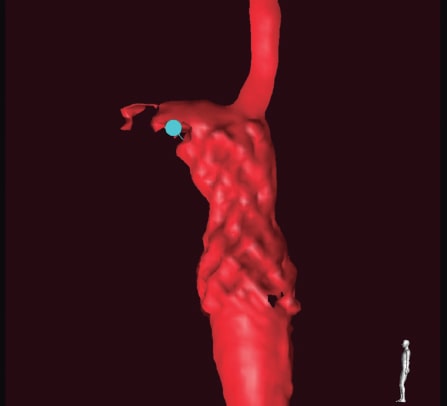
The data of progressive recoarctation were obtained from the echocardiography and magnetic resonance imaging at the outpatient follow-up, and the hypertensive response from the ergometric work. The case was brought to the heart team that decided to perform endovascular treatment. The aortography performed via right femoral access confirmed the presence of recoarctation at the junction between the aortic arch and the descending thoracic aorta (figure 1A,B, blue arrow) with a minimum diameter of 9 mm, and a peak-to-peak gradient of 20 mmHg. Similarly, a saccular-shaped pseudoaneurysm was found adjacent to the stenosed region (figure 1A,B; figure 2A, yellow arrow; video 1 of the supplementary data) with internal diameters of 8 mm x 10 mm (figure 2B). Therefore, it was decided to implant a 45 mm long covered stent (Covered CP Stent, NuMED Canada) (figure 3) with good angiographic results (videos 2 and 3 of the supplementary data), no evidence of residual gradient, and successful and complete exclusion of the pseudoaneurysm.
Figure 1.
Figure 2.
Figure 3.
The use of imaging modalities with 3D analysis including traditional fluoroscopy is a very useful tool to diagnosis of complex anatomies and plan therapeutic alternatives. Also, it allows us to shorten the duration of the procedure, reduce the dose of contrast used, and minimize radiation exposure time.
The patient’s written informed consent was obtained before publishing this clinical case.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
N. Barja González wrote the manuscript first draft as well as its final version. F. Rueda Núñez, and I. Martínez Bendayán provided the supplementary data and reviewed the manuscript draft and final version.
CONFLICTS OF INTEREST
None reported.