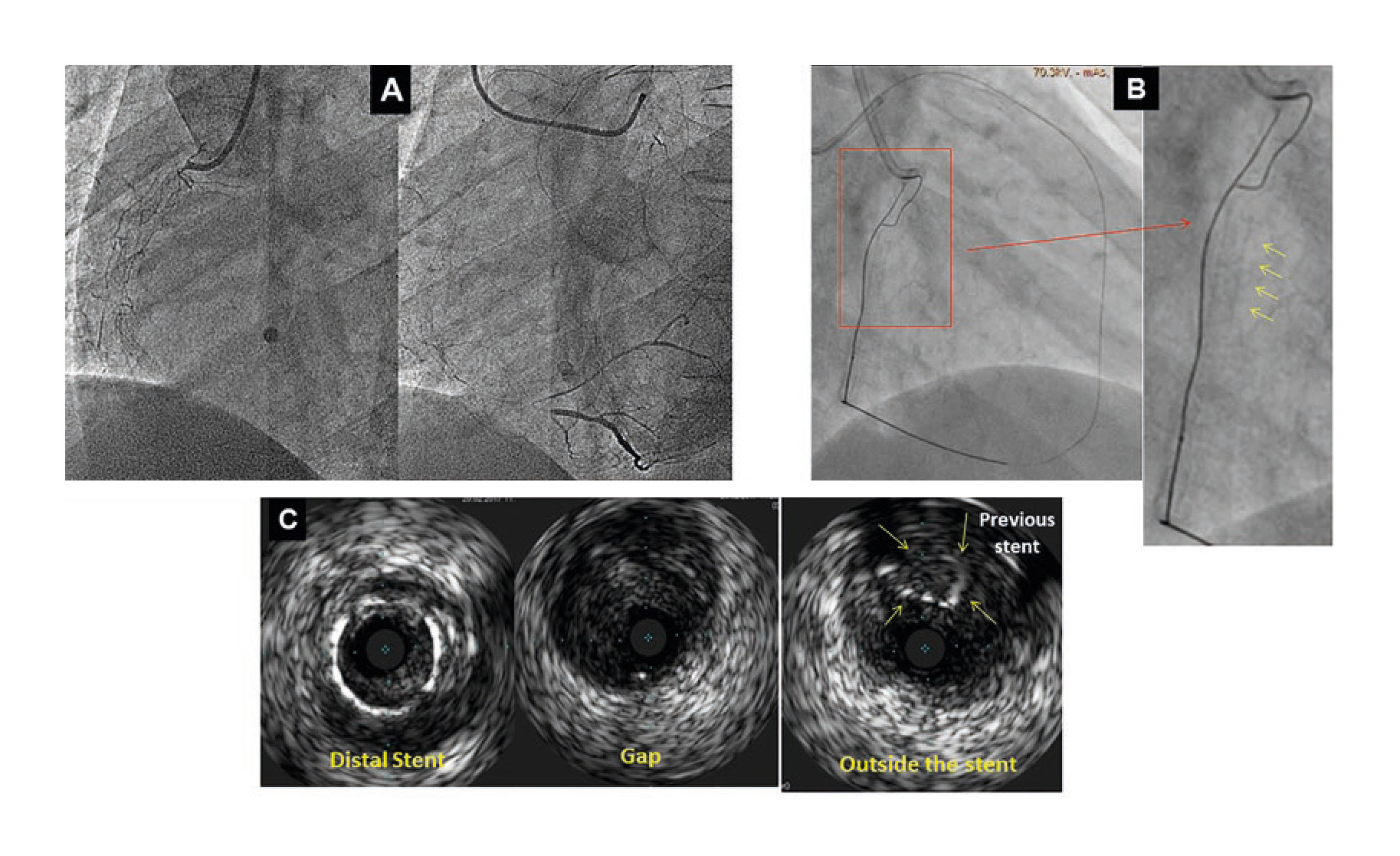
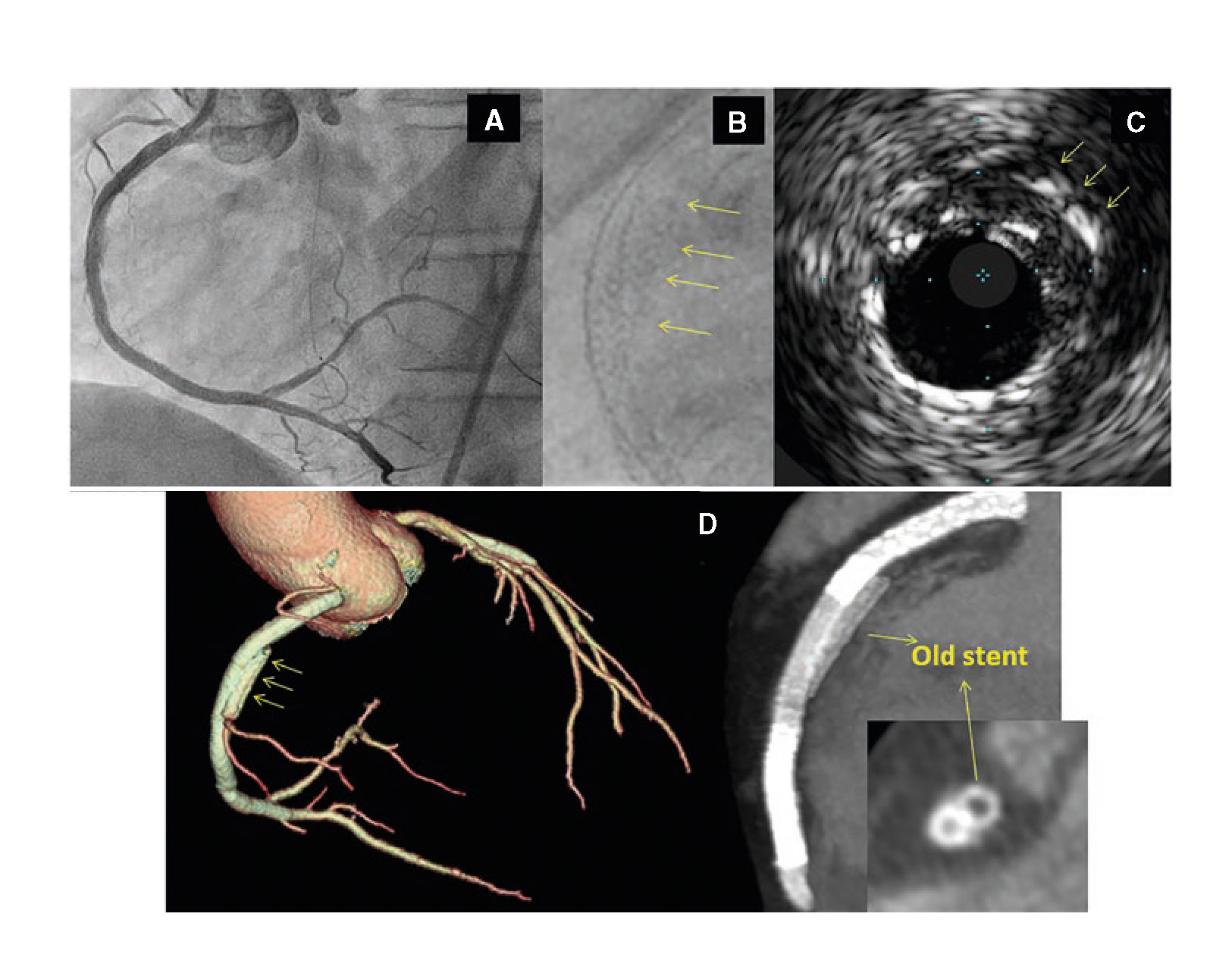
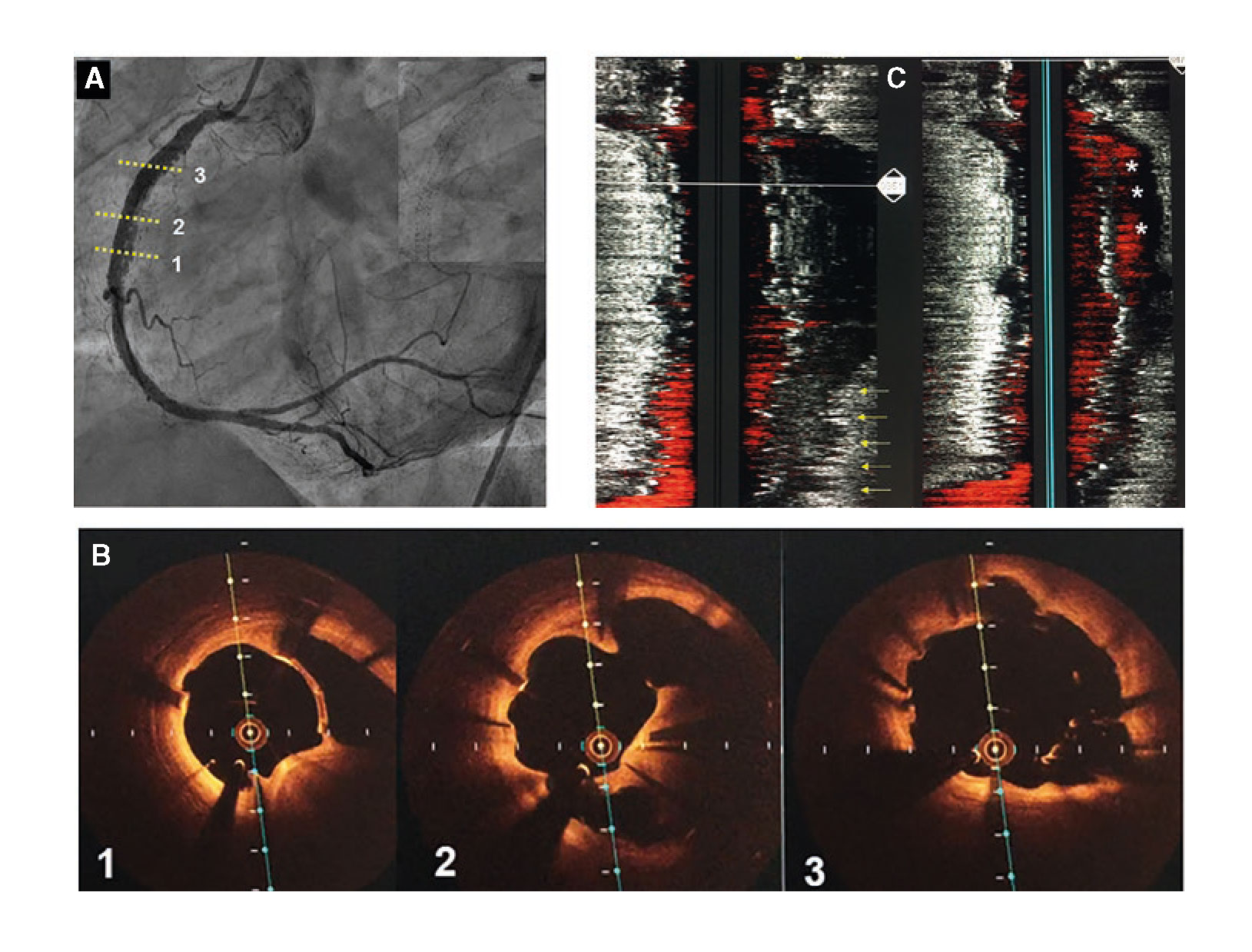
A 48-year-old male was admitted to the hospital due to stable angina. The coronary angiography showed a very long in-stent coronary chronic total occlusion in his right coronary artery (RCA) (figure 1A). We attempted the retrograde access following failed antegrade access. At mid-RCA level, the guidewire was advanced outside the stent (arrows) (figure 1B). The intravascular ultrasound (IVUS) conducted confirmed the correct position of the guidewire at the stent distal edge. However, in the gap between both stents, the guidewire was advanced to the subadventitial space and maintained this position along the full length of the proximal stent (arrows) (figure 1C). After predilation, 3 drug-eluting stents were successfully implanted (figure 2A). A double stent can be seen in the angiographic and IVUS images obtained (figure 2B and figure 2C): the previous (arrows) and the newly implanted stent. The computed tomography scan conducted 3 months later confirmed the exclusion of the old stent (arrows) from the coronary flow and the patency of the stents implanted in the subadventitial space (figure 2D). Six months after the index procedure, a new angiographic assessment confirmed the long-lasting good results (figure 3A). However, the optical coherence tomography showed significant late-acquired stent malapposition (figure 3B). The IVUS longitudinal views showed the old occluded stent (arrows) and, on the other plane, the stent malapposition (asterisks) (figure 3C), probably due to the hematoma reabsorption induced during the recanalization process. The patients remained asymptomatic. It was decided to maintain aspirin and ticagrelor until the next reassessment scheduled after an 18-month follow-up.
Figure 1
Figure 2
Figure 3