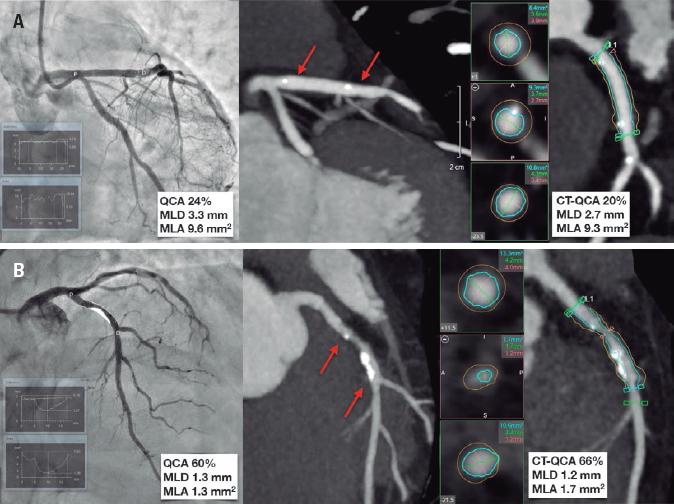
Fifty-five-year-old male with signs of angina and anterior ischemia as seen on the single-photon emission computed tomography. The invasive coronary angiography performed confirmed the presence of significant stenosis in the proximal left anterior descending coronary artery (LAD). A percutaneous coronary intervention was attempted using a 3.5 x 20 mm Magmaris bioresorbable scaffold. At the 12-month follow-up and as part of a clinical research protocol, both the control invasive coronary angiography and cardiac computed tomography (cardiac CT) performed confirmed the good correlation between the minimum lumen diameter (MLD) and the minimum lumen area (MLA). The quantitative coronary angiography (QCA) performed showed the same results (figure 1A; note that in the cardiac CT the 2 hyperintense points pointed with red arrows show the location of the borders of the stent.)
Figure 1.
A second 65-year-old male with previous ischemic heart disease underwent an invasive coronary angiography due to new-onset angina that revealed the presence of a significant stenosis in the proximal LAD. A percutaneous coronary intervention was performed using a 3.5 x 15 mm Magmaris scaffold. At the 12-month follow-up, the angina symptoms relapsed with a positive ergometric test to moderate load. The cardiac CT revealed the presence of moderate in-stent restenosis that was later confirmed and treated percutaneously. Also, in this clinical scenario a good correlation was seen between the diameters and the areas measured with both imaging modalities (figure 1B).
Both cases suggest that cardiac CT can be a useful tool in the follow-up of patients who are carriers of a Magmaris bioresorbable scaffold, especially in patients with larger diameters implanted in not severely calcified lesions. This may be applicable to other types of polylactic acid-based devices if the new generations of devices achieve enough clinical evidence. The present study was conducted in accordance with the Helsinki Declaration Code of Ethics. The patients granted their verbal and written consent to the diagnostic tests, and to the data analysis and processing.
FUNDING
No funding was received for this work.
CONFLICTS OF INTEREST
None declared.
ACKNOWLEDGEMENTS
The authors wish to thank the funding from Canon Medical through an unconditional graft.