This is the case of a 27-year-old male patient admitted to our hospital with acute oppressive chest pain. Clinical history was only remarkable for HIV infection under treatment with antiretroviral therapy. The electrocardiogram revealed the ST-segment elevation in leads II, III, aVF, and a QS-pattern in leads V1 to V4 suggestive of established anterior necrosis.
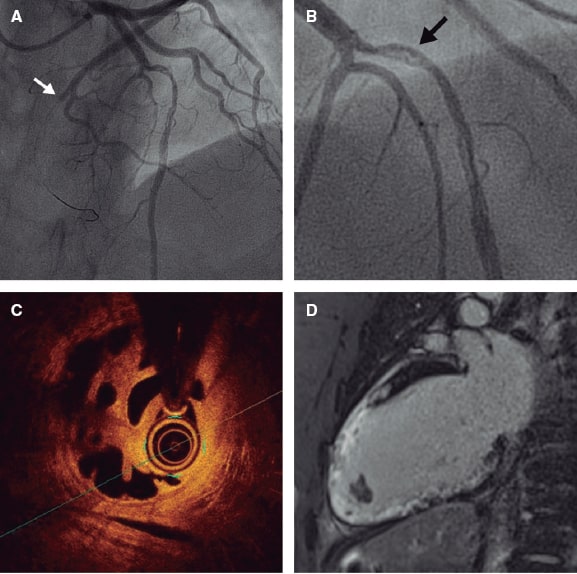
Coronary angiography was performed 1 hour after symptom onset revealing a total acute thrombotic occlusion of the left circumflex artery (white arrow, figure 1A), and angiographic haziness in the mid left anterior descending coronary artery (black arrow, figure 1B). The circumflex artery was treated with thrombectomy and angioplasty with drug-eluting stent implantation. The optical coherence tomography performed on the left anterior descending coronary artery revealed a honeycomb-like structure with multiple intraluminal channels. (figure 1C, video 1 of the supplementary data). The MRI confirmed the presence of moderate left ventricular systolic dysfunction (left ventricular ejection fraction = 45%), established anterior, anteroseptal, apical, and inferoseptal transmural necrosis without myocardial viability, and apical thrombi. (figure 1D). Dyslipidemia and thrombophilia were investigated and discarded. The patient was discharged on triple antithrombotic therapy. Informed consent was obtained from the patient for case report purposes.
Figure 1.
Woven coronary artery disease is an extremely rare congenital anomaly in which the coronary artery branches into multiple thin channels that merge once again to form a normal vessel. The optical coherence tomography is crucial here for the differential diagnosis of thrombotic recanalization, dissection or chronic occlusion with bridging collaterals. In woven disease, histopathology and intravascular imaging have reveal the presence of elastic tunicae and endothelial coating. In our case, despite the patient’s young age, the presentation of ST-segment elevation myocardial infarction in a different coronary territory, the electrocardiogram changes suggestive of anterior necrosis, the magnetic resonance imaging findings, and the intravascular imaging all confirmed thrombotic recanalization.
FUNDING
None reported.
AUTHORS’ CONTRIBUTIONS
All authors have participated in the writing of this article, edition, and graphic composition of the figures and video. All authors approved the final version of this manuscript.
CONFLICTS OF INTEREST
None reported.
SUPPLEMENTARY DATA
Vídeo 1. Serra-Creus B. DOI: 10.24875/RECICE.M21000226