The calcified nodule has been established as the least common underlying substrate in the acute coronary syndrome; however calcium can be widely present in other acute-common scenarios. In this setting, the optical coherence tomography (OCT) study has identified 3 different types of calcification according to morphology. Former studies have already documented calcified nodules in patients with peripheral artery disease; however the different patterns that exist beyond coronary arteries remain unknown.
An 80-year-old patient was referred for coronary angiography following systolic dysfunction. The coronary angiography performed through right radial approach showed a severely calcified vessel (mid portion of the left anterior descending artery) and mitral and aortic calcification. The OCT pullback performed with 6 mL of contrast at 3 mm/seg through the radial artery removed 4 cm of the radial sheath and showed multiple calcified plaques (mid portion of the artery) defined by the presence of superficial, well-established, low-backscattering and heterogeneous regions (video 1 of the supplementary data). The simultaneous angiography co-registration confirmed the presence of ulnar artery occlusion. Three patterns of superficial calcification were identified:
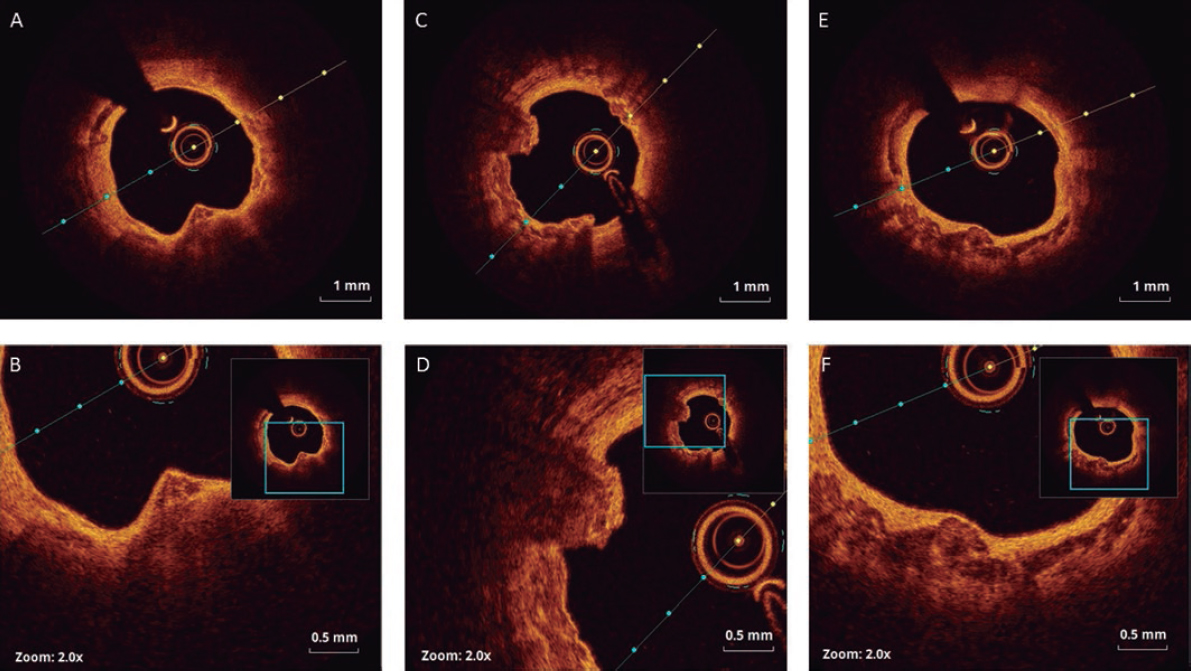
- – Calcified protrusion (protruding calcified mass without eruptive nodules [figure 1A,B]).
- – Eruptive calcified nodules (cluster of small calcified nodules protruding into the lumen [figure 1C,D]).
- – Sheet-like superficial calcified plate (without superficial coating disruption and minimal laminar protrusion [figure 1E,F]).
Figure 1.
The types and causes of peripheral calcification described included calcified atherosclerosis, calcific medial vasculopathy, elastocalcinosis, and calcific uremic arteriolopathy. This is the first time that an OCT study describes calcification patterns of atherosclerotic plaques in peripheral artery disease. As previously defined for calcified coronary culprit lesions, 3 types could be identified. The coexistence of ulnar artery occlusion suggests causality, but further studies will be needed to clarify its pathological meaning in the setting of the acute peripheral syndrome.
CONFLICTS OF INTEREST
R. Moreno Gómez is associate editor of REC: Interventional Cardiology. The journal’s editorial procedure to ensure impartial handling of the manuscript has been followed.
SUPPLEMENTARY DATA
Video 1. Arroyo-Úcar E. DOI: 10.24875/RECICE.M20000094