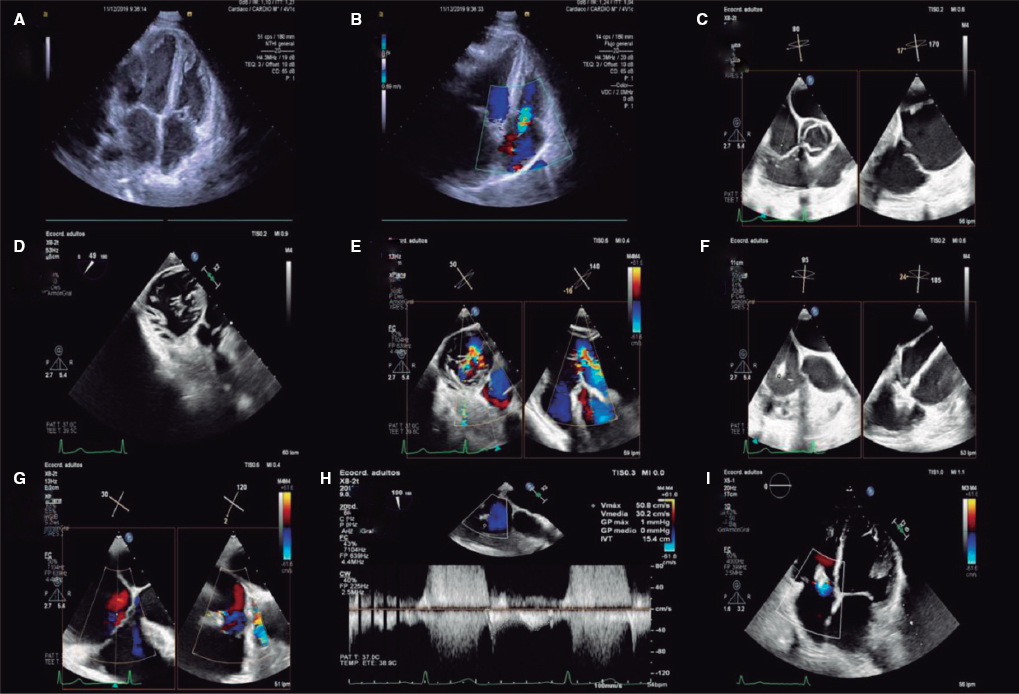
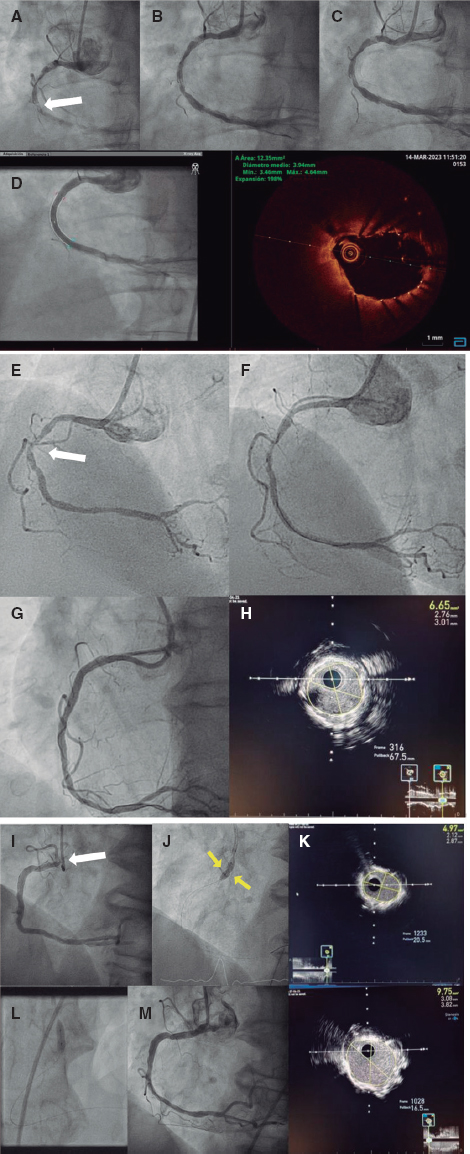
This is the case of a 72-year-old man with mitral and aortic mechanical prosthetic valves, chronic kidney disease, and severe pulmonary hypertension. In 2019, a mitral anterolateral paravalvular leak (PVL) was percutaneously closed with implantation of 2 devices (the AVP III 10 mm x 5 mm, and the AVP III 8 mm x 4 mm, St Jude Medical, United States) due to heart failure. The patient’s clinical progression was favorable with moderate mitral regurgitation. One year later, the patient’s symptoms worsened, and the transesophageal echocardiogram performed revealed severe mitral regurgitation due to recurrent PVL around the devices (figure 1A). A second percutaneous closure attempt was scheduled to close the PVL. The initial procedure was to implant another device next to the other devices, but they embolized into the left ventricle when the deflectable catheter touched them (figure 1B). They were captured using a gooseneck loop snare through the PVL and then retrieved using 2 sheaths in the left atrium (figure 1C). Two hours later, the patient developed hemodynamic instability, and ST-segment elevation. An emergency coronary angiogram revealed the presence of severe stenosis in the left main coronary artery (LMCA) that was not present in the previous angiogram (figure 1D). The optical coherence tomography demonstrated calcium embolization (figure 1E) that was treated with stenting (figure 1F). Eventually, the patient underwent the surgical repair of the PVL. As far as we know, this is the first time that coronary artery embolization of calcified tissue in the LMCA is ever reported during maneuvers to retrieve embolized devices in the left ventricle. The non-occlusive nature of the LMCA embolus may have led to a better prognosis. The patient accepted the publication of the case and have his informed written and signed consent.
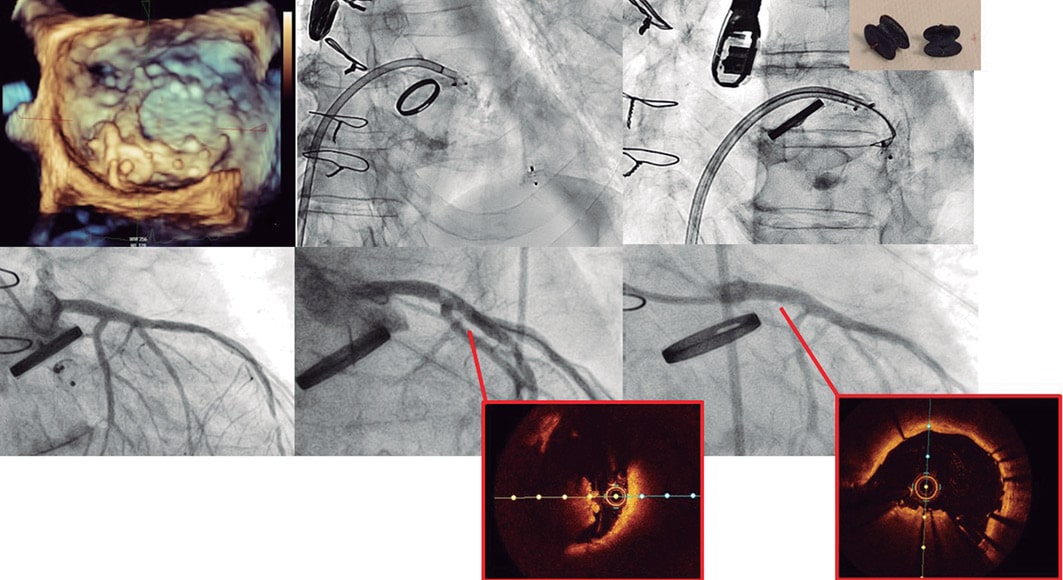
Figure 1.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
A. Pardo Sanz gathered all the information, prepared, and drafted the case report. L. Salido Tahoces was one of the interventional cardiologists involved. J.L. Mestre Barcelo, and M. Abellás Sequeiros helped prepare the case. J.L. Zamorano Gómez is the head of the cardiology unit and collaborated during the manuscript review process. Á. Sánchez-Recalde is the head of the interventional cardiology unit, and one of the operators of the case.
CONFLICTS OF INTEREST
None reported.
* Corresponding author.
E-mail address: anapardosanz0@gmail.com (A. Pardo Sanz).