QUESTION: Could tell us what the prevalence of angina without obstructive coronary artery disease is in patients referred for invasive angiography and how has it evolved over the last few years?
ANSWER: Nearly half of the patients referred for cardiac catheterization due to suspected stable angina have coronary arteries without obstructive lesions.1 These numbers are even higher in the series of patients studied through cardiac computed tomography to the point that up to 3 out of 4 patients do not show any obstructive lesions. Women have a higher prevalence compared to men of up to 70%. Therefore, angina without obstructive lesions should not be considered a secondary problem, but a fundamental aspect of our routine clinical practice at the cath lab. Also, these patients have high rates of recurring angina and disability,2 which means that achieving the proper diagnosis and administering the right treatment is of paramount importance.
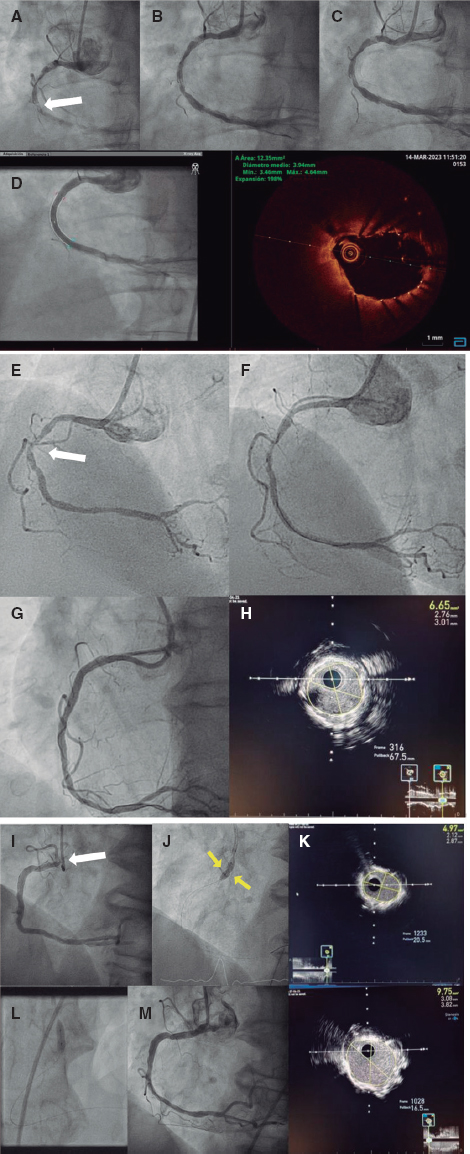
Q.: We have been using the expression «without obstructive coronary artery disease», but it can be put into context. Shouldn’t we rather say «without angiographically significant stenoses». Do you think that the physiological significance of stenoses with guidewire pressure should always be excluded, even the mild ones?
A.: With the evidence available, I believe that the systematic use of guidewire pressures to assess mild epicardial lesions is not justified. As a matter of fact, the correlation and concordance between angiography and fractional flow reserve (FFR) are modest, which is especially important in 50% to 90% stenoses where the angiography often overestimates functional severity systematically with rates of false positives > 50%.3 On the other side of the spectrum, stenotic lesions < 50% on the angiography have a relatively low risk of being ischemic on the FFR and are almost anecdotal if < 30%. In a study conducted with 139 patients with angina and without obstructive lesions, the frequency rate of lesions with FFR ≤ 0.8 was 5%.4 On the other hand, we should mention that the cut-off value validated to tag a coronary lesion as ischemic is 0.75 although, in practice, 0.8 is used to decide on whether to revascularize or not.
Regarding the clinical benefit of this approach, the large clinical trials that have proven the utility of FFR have only studied lesions > 50%, which is why we don’t have data supporting the clinical utility of assessing mild lesions.5,6 The RIPCORD-2 trial7 presented in the Congress held by the European Society of Cardiology back in September 2021 included patients with, at least, 1 stenotic lesion > 30%. All these patients’ vessels were studied using the FFR and no clinical benefit was found. What this means is that probably the greatest benefit of FFR is to avoid unnecessary revascularizations, and to clarify the significance of truly suspicious lesions.
In practice, I think that the best thing to do is to individualize the decision-making process considering the angiographic severity, location of the lesion, and quality of angiographic assessment. A 20% lesion in a diagonal branch and a 40% lesion in the proximal left anterior descending coronary artery are 2 completely different things. Also, a focal lesion in a well-studied segment does not cast the same doubts as a long and calcified disease where a good angiographic assessment is not an easy thing to do due to curves, shortening, etc. Finally, we should remember that if a decision is made to measure microvascular function using a flow-pressure guidewire, the FFR can be established, almost at the same time, on suspicious lesions.
Q.: Once the significant stenosis of the epicardial vessel has been excluded, what should be the assessment protocol inside the cath lab?
A.: The invasive assessment of ischemia without obstructive lesions rests on 2 pillars mainly: the study of microcirculation, and the study of vascular reactivity.
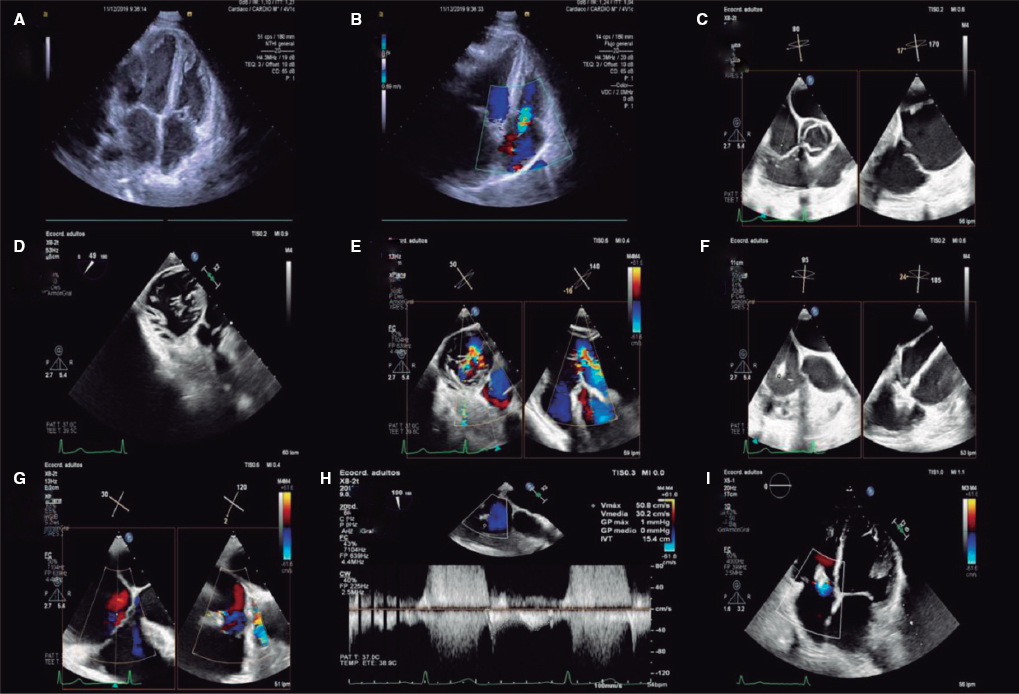
The study of microcirculation consists of assessing coronary flow at rest and during maximum hyperemia. To this end, pressure and flow guidewires, whether thermodilution-based (PressureWire, Abbott, United States) or Doppler-based (Combowire, Philips, The Netherlands) are used. Baselines measures are taken, then maximum hyperemia is induced with adenosine to eventually take the same measures once again. This allows us to estimate the coronary flow reserve that is the ratio between hyperemic and baseline flow (which should be > 2). Coronary flow reserve < 2 means that, in situations of exercise or other stressors, the patient cannot duplicate his oxygen supply to the myocardium eventually, thus leading to ischemia easily. Added to flow coronary reserve, the combination of pressure and hyperemic flow, can also estimate microvascular resistance. The most widely used measure is the microvascular resistance index (considered pathological if > 25.)8
The second part is to assess vasoreactivity since coronary arteries do not necessarily respond to physiological stimuli the same way they do to adenosine. As a matter of fact, coronary flow and vascular tone both of epicardial artery and microcirculation largely depend on the production of nitric oxide by the endothelium. If this production does not properly work, paradoxical vasoconstriction can be seen in physiological situations that would require hyperemia. That is why it is important to assess coronary reactivity, preferably using the acetylcholine provocation testing. It allows us to discard the presence of vasospastic angina, and endothelial dysfunction. We have recently published an article on REC: Interventional Cardiology with a detailed description on how to run and then interpret an acetylcholine provocation testing.9
This approach based on microvascular function and on the acetylcholine provocation testing has been backed by a group of experts from the European Society of Cardiology.8 Regarding the logistics of the procedure, each lab should assess, depending on time availability, resources, and experience whether to perform the procedure ad hoc or whether to stage it, and arrange the order in which the tests will be run. We should bear in mind that, although the assessment of microcirculation requires the previous administration of nitroglycerin, the acetylcholine provocation testing requires just the opposite. Therefore, a possibility is to perform the angiography without nitroglycerin first, then the acetylcholine provocation testing, and finally measure the microvascular function. If nitroglycerin has been administered to achieve the diagnosis, the best thing to do is to measure the microvascular function next and leave the acetylcholine provocation testing for the end.
Q.: Is it possible to draw therapeutic implications from the comprehensive assessment of micro- and macrovascular coronary physiology?
A.: The main problem with microvascular and endothelial dysfunction is that no large clinical trial has ever confirmed any benefits regarding adverse events with any drugs. However, this should not take us to therapeutic nihilism because some former studies have proven the utility of different drugs reducing symptoms and improving quality of life.
If the patient is diagnosed with microvascular dysfunction, the first-line therapy here is beta-blockers. As coadjuvant or alternative therapy ivabradine, ranolazine, nicorandil, and calcium channel blockers can be used; nitroglycerin is not very useful here because it has a minor effect on microcirculation. Statins, and renin-angiotensin system inhibitors are advised too for the primary prevention of events.
If endothelial dysfunction-induced vasoconstriction or vasospastic angina are predominant, beta-blockers are ill-advised since they can make things worse. In this case, the first-line therapy is calcium channel blockers, nitrates, and nicorandil. The use of statins, and renin-angiotensin system inhibitors can be considered here too.
Empirical treatment has often been advised as an easier approach compared to physiological diagnosis and targeted therapy. Once again, each center should adapt its own clinical practice to its own possibilities. However, my own experience is that when these patients are not properly studied, they are not committed to the frequent visits that a careful empirical treatment would require; on the contrary, they are often discharged from the hospital and assessed at the 1-year follow-up, preventing us from conducting a proper follow-up of the symptoms and the effectiveness of treatment. On the other hand, considering that based on the physiological problem, there are very little effective treatments (like nitrates in microvascular dysfunction), and others are harmful (like beta-blockers in vasospasm), I think empirical treatment confront us with true dilemmas when treating patients who are not doing well.
Q.: What is the clinical evidence behind the invasive comprehensive assessment of coronary circulation? Have some advantages been identified regarding prognosis?
A.: Numerous studies from the 90s have proven that physiological disorders in patients with angina and without obstructive lesions are directly associated with myocardial ischemia and with long-term prognosis, as well as with the presence of atheromatous plaques and vulnerability data from intravascular imaging modalities. This is important because it is wrong to assume that all patients with angina and without lesions have the same disease and the same benign prognosis. Truth is that patients with endothelial and microvascular dysfunction have a far worse prognosis compared to patients with normal studies. Also, small trials have allowed us to establish the efficacy of different drugs based on the type of physiological dysfunction, as we have already discussed, thus supporting targeted therapy.
Regarding the prognostic benefit of individualized therapy, the CorMicA trial proved that this approach is superior to empirical treatment offering a better quality of life after 6 and 12 months.10 To this date, we are still lacking studies with large enough samples to detect benefits regarding the adverse events. The iCorMicA trial (clinicaltrials.gov. Identifier: NCT04674449), currently ongoing, will be recruiting 1500 patients to study the benefits in quality of life and adverse events. In any case, with the results of the ISCHEMIA trial in mind,11 I believe that only focusing on reducing hard events is a mistake that can prevent patients from receiving therapies that do help from the symptomatic and functional standpoint. In conclusion, I think there are enough scientific data to say that patients with angina and without obstructive lesions benefit from knowing their physiology and receiving individualized therapies.
FUNDING
None whatsoever.
CONFLICTS OF INTEREST
The author has received payments for training sessions organized by Abbott.
REFERENCES
1. Wang ZJ, Zhang LL, Elmariah S, Han HY, Zhou YJ. Prevalence and Prognosis of Nonobstructive Coronary Artery Disease in Patients Undergoing Coronary Angiography or Coronary Computed Tomography Angiography. Mayo Clin Proc. 2017;92:329-346.
2. Shaw LJ, Merz CNB, Pepine CJ, et al. The Economic Burden of Angina in Women With Suspected Ischemic Heart Disease:Results From the National Institutes of Health-National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation. Circulation. 2006;114:894-904.
3. Park S-J, Kang S-J, Ahn J-M, et al. Visual-Functional Mismatch Between Coronary Angiography and Fractional Flow Reserve. JACC Cardiovasc Interv. 2012;5:1029-1036.
4. Lee BK, Lim HS, Fearon WF, et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015;131:1054-1060.
5. Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224.
6. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991-1001.
7. Curzen N. RIPCORD 2:does routine pressure wire assessment influence management strategy of coronary angiography for diagnosis of chest pain?En:ESC Congress 2021. The Digital Experience;2021, 27-30 August. Available online:https://digital-congress.escardio.org/ESC-Congress/sessions/2835-hot-line-ripcord-2. Consultado 4 Sep 2021.
8. Kunadian V, Chieffo A, Camici PG, et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology &Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41:3504-3520.
9. Gutiérrez E, Gomez-Lara J, Escaned J, et al. Valoración de la función endotelial y provocación de vasoespasmo coronario mediante infusión intracoronaria de acetilcolina. Documento técnico del Grupo de Trabajo de diagnóstico intracoronario de la Asociación de Cardiología Intervencionista. REC Interv Cardiol. 2021. https://doi.org/10.24875/RECIC.M21000211
10. Ford TJ, Stanley B, Sidik N, et al. 1-Year Outcomes of Angina Management Guided by Invasive Coronary Function Testing (CorMicA). JACC Cardiovasc Interv. 2020;13:33-45.
11. Maron DJ, Hochman JS, Reynolds HR, et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med. 2020;382:1395-1407.
* Corresponding author: Servicio de Cardiología, Hospital Gregorio Marañón, Doctor Esquerdo 46, 28007 Madrid, Spain.
E-mail address: egutibanes@gmail.com (E. Gutiérrez Ibañes).