QUESTION: Is there a specific profile of patients with angina and without obstructive coronary artery disease?
ANSWER: Although we have been paying more attention to angina without obstructive coronary artery disease over the last few years (a more truthful denomination compared to ischemia with normal coronary arteries because it focuses on the clinical problem and also because many patients don’t have strictly normal coronary arteries) we still don’t know much about this syndrome. Syndrome X was the term coined back in 1973 after the group of patients with normal coronary arteries that was called group X.1 Actually this term is more appropriate since this is the letter used in algebra to represent something that remains unknown.
Answering your question, it is more common in women; it is often exertional although a different kind of pattern has been reported too (first effort, at rest during certain hours, especially at night-time, exertional dyspnea); also, it is associated with known cardiovascular risk factors since most patients with angina and without obstructive coronary artery disease have coronary atherosclerosis.2 Obesity, the association with inflammatory diseases (such as systemic lupus erythematous), mood swings, intolerance to different drugs are not rare, and make us have to try several combinations to control de symptoms.
Although it seems reasonable to suspect that a patient with angina may not have coronary artery lesions justifying the symptoms, these patients’ profile is somehow similar to that of patients with clinically significant coronary artery lesions. Only an imaging modality capable of discarding clinically significant coronary artery disease can lead to a definitive diagnosis of angina without obstructive coronary artery disease.
Q.: The diagnosis of type of angina is, by definition, achieved after performing an invasive coronary angiography, but since the use of the computed tomography (CT) scan for coronary artery assessment has become more popular, can it also be diagnosed with a non-invasive angiography with a CT scan?
A.: To achieve the diagnosis of angina without obstructive coronary artery disease the following requirements need to be met:3 a) compatible symptoms, b) lack of obstructive coronary artery disease, c) myocardial ischemia, and d) microvascular dysfunction. Therefore, if microvascular dysfunction is not confirmed, the diagnosis cannot be achieved. To answer this question properly we should ask ourselves a couple more questions first: can we diagnose microvascular dysfunction with non-invasive imaging modalities including the CT scan? also, can we achieve the diagnosis only with the clinical signs and proof that there is no obstructive coronary artery disease?
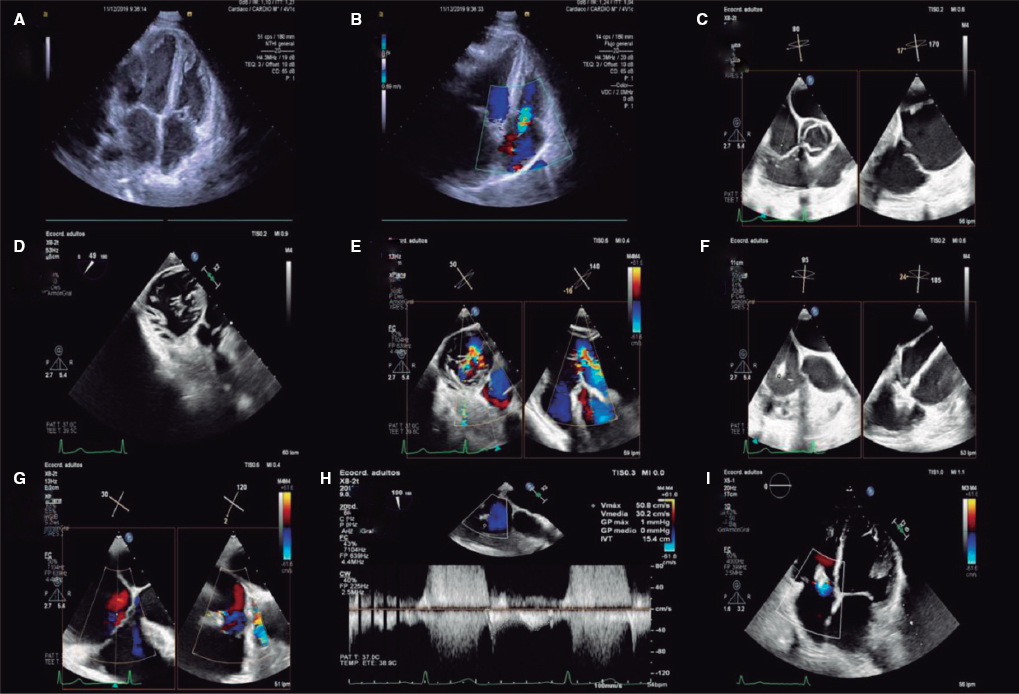
The diagnosis of microvascular dysfunction with non-invasive imaging modalities is feasible, although these are expensive or have been insufficiently validated. Positron emission tomography4 and magnetic resonance imaging5 have been able to confirm the presence of microvascular dysfunction in patients without macrovascular disease in different clinical settings. Contrast echocardiography6 and Doppler echocardiography of the left anterior descending coronary artery7 have also yielded favorable results in this context, but they are barely used.
Although it does not seem right to achieve the diagnosis without prior confirmation of microvascular dysfunction, it can be reasonable under certain circumstances. If the patient has typical symptoms and cardiovascular risk factors, treatment can be initiated after discarding obstructive coronary artery disease with a CT scan. If symptoms cannot be controlled, we can turn to the invasive study of microvascular function. This can be the go-to strategy in elderly or frail patients or with severe noncardiac diseases. It can even be used for the rest of patients since delaying symptom control does not compromise or worsen prognosis.
Q.: In the presence of mild or moderate stenoses on the CT scan, do you think that a non-invasive assessment of ischemia can help?
A.: Theoretically speaking, as I have already mentioned, we need confirmation of myocardial ischemia to achieve a definitive diagnosis of microvascular disease. There are situations, however, when we can assume the diagnosis if the patient shows typical symptoms and obstructive coronary artery disease has been discarded.
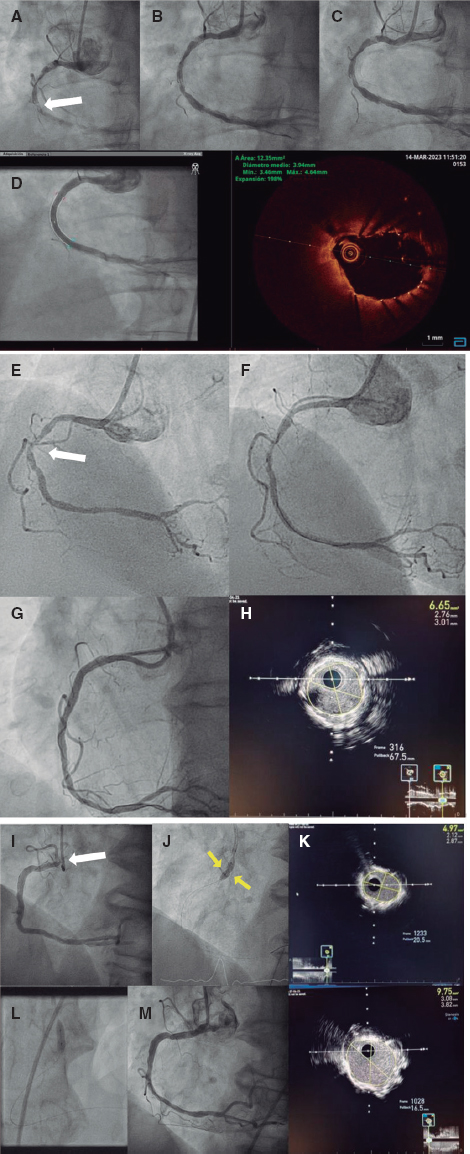
In patients with CT scans showing non-severe coronary artery lesions, we need to make sure that these lesions are not functionally significant before accepting the diagnosis of microvascular disease. The milder the lesion, the more certain we’ll be that it is a non-functionally significant lesion, but microvascular dysfunction. Therefore, in moderate lesions, functional assessments are necessary to discard functionally significant disease. This assessment can be made while the CT scan is being performed by assessing coronary flow reserve8 or with functional tests to see if there are traces of ischemia, and whether these traces originate at the diseased artery.
In any case, to me this question looks more like an academic issue than a practical one. If a patient has angina pectoris, a positive functional test for ischemia, a CT scan showing moderate disease of a coronary artery, and no left main coronary artery disease, medical therapy can be initiated, and the evolution of symptoms assessed. That is so because prognosis is not much better with an invasive approach as the ISCHEMIA trial proved.9
Q.: There are times when, depending on the center, the clinician can find himself with a symptomatic patient for angina who has been diagnosed with lack of coronary stenoses without even an invasive study of coronary physiology. What would the role of non-invasive imaging modalities be here?
A.: That is correct, a few years ago that was the rule of thumb: coronary artery disease was discarded, and there was no need to assess the vascular function. Currently, cardiologists are more aware of its importance, in part due to the interest shown by interventional cardiologists in this disease. Even so, we still see patients with angina pectoris in whom obstructive epicardial vessel disease has been discarded, but endothelium-related o non-related vascular dysfunction hasn’t.
A positive ischemia assessment testing supports the diagnosis of microvascular dysfunction and, even in the absence of an invasive study of coronary physiology, it is good enough to initiate therapy. But if the patient does not get any better with the treatment suggested the invasive assessment of coronary physiology will be necessary to direct therapy towards the specific origin that’s causing the coronary disorder.
Q.: What specific medical therapies are optimal based on the profile of coronary micro- and macrovascular pathophysiology?
A.: Evidence-based recommendations are very scarce. In the first place, cardiovascular risk factors should be put under control adequately, especially hypertension and diabetes mellitus, both of which contribute to vascular disease. Angiotensin-converting enzyme inhibitors and statins have proven effective to treat these patients. Controlling weight is essential, and a cardiac rehabilitation program can reduce symptoms and improve quality of life.
All types of antianginal drugs can be used in these patients, many times using a trial-and-error approach to it, because patients may be intolerant or drugs ineffective.
To choose the optimal drug therapy we should make a distinction between 2 different profiles of patients with angina pectoris without obstructive coronary artery disease: those with vasospastic angina pectoris and those with microvascular angina pectoris.
Patients with micro- or macrovascular spasm benefit from calcium channel blockers. Both dihydropyridine and non-dihydropyridine drugs can be effective, and the lack of effectiveness of one does not predict a lack of effectiveness of the other. Also, nitrates, both oral an in patches, can be used in this context.
In patients with microvascular angina pectoris not due to vasospasm, beta-blockers, calcium channel blockers, ranolazine, aminophylline, and trimetazidine have given effective results in preliminary trials, but not yet in randomized clinical trials. Although nitrates can be used in this type of patients, it has been proposed that symptoms could become worse.
Finally, antianginal drugs without significant hemodynamic effects can minimize symptoms in both groups of patients, especially ranolazine and trimetazidine.
Q.: With this therapeutic individualization, have any advantages been identified regarding prognosis?
A.: No beneficial effects have been confirmed regarding prognosis in mortality or myocardial infarction. However, fewer events of angina pectoris have been reported leading to a better quality of life, which is essential in these patients. The CorMicA trial10 confirmed that an invasive study of coronary physiology in patients with chest pain and without obstructive coronary artery disease could identify 3 different groups (vasospastic angina pectoris, microvascular angina pectoris, and noncardiac chest pain). Also, that a specific medical strategy for each specific group reduced the occurrence of angina pectoris.
FUNDING
None whatsoever.
CONFLICTS OF INTEREST
None reported.
REFERENCES
1. Arbogast R, Bourassa MG. Myocardial function during atrial pacing in patients with angina pectoris and normal coronary arteriograms. Comparison with patients having significant coronary artery disease. Am J Cardiol. 1973;32:257-263.
2. Lee BK, Lim HS, Fearon WF, et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015;131:1054-1060.
3. Kunadian V, Chieffo A, Camici PG, et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology &Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41:3504-3520.
4. Di Carli MF, Charytan D, McMahon GT, Ganz P, Dorbala S, Schelbert HR. Coronary circulatory function in patients with the metabolic syndrome. J Nucl Med. 2011;52:1369-1377.
5. Panting JR, Gatehouse PD, Yang GZ, et al. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med. 2002;346:1948-1953.
6. Caiati C, Montaldo C, Zedda N, et al. Validation of a new noninvasive method (contrast-enhanced transthoracic second harmonic echo Doppler) for the evaluation of coronary flow reserve:comparison with intracoronary Doppler flow wire. J Am Coll Cardiol. 1999;34:1193-1200.
7. Hildick-Smith DJ, Maryan R, Shapiro LM. Assessment of coronary flow reserve by adenosine transthoracic echocardiography:validation with intracoronary Doppler. J Am Soc Echocardiogr. 2002;15:984-990.
8. Khav N, Ihdayhid AR, Ko B. CT-Derived Fractional Flow Reserve (CT-FFR) in the Evaluation of Coronary Artery Disease. Heart Lung Circ. 2020;29:1621-1632.
9. Maron DJ, Hochman JS, Reynolds HR, et al.;ISCHEMIA Research Group. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med. 2020;382:1395-1407.
10. Ford TJ, Stanley B, Good R, et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina:The CorMicA Trial. J Am Coll Cardiol. 2018;72:2841-2855.
* Corresponding author: Servicio de Cardiología, Hospital Clínico Universitario de Valladolid, Avda. Ramón y Cajal s/n 7.ª planta, 47003 Valladolid, Spain.
E-mail address: asanroman@secardiologia.es (J.A. San Román).