CASE PRESENTATION
Fontan procedure is a complex surgery with more risks compared to other cardiac surgeries. Also, complications have been associated with it because of its physiology being the most common of all elevated blood pressure in the cavopulmonary connection, low cardiac output syndrome, hypoxemia, and arrhythmias; others like plastic bronchitis, protein-losing enteropathy, ascites, pleural effusion, portal hypertension, and hepatic fibrosis can also occur. Similarly, connections between the pulmonary and the systemic circuits can be established triggering higher pressures of Fontan circulation.
This is the case of a 17-year-old male patient diagnosed at birth with tricuspid atresia with restrictive interventricular communication (IVC), large vessel malapposition, and severe mixed pulmonary stenosis (PS). The patient’s corresponding informed consents—that remain on file—were obtained to conduct this study.
At the age of 7 the patient was treated with a single-stage fenestrated Fontan procedure with independent anastomoses of the superior vena cava and, on the other hand, right atrial roof with right pulmonary branch, ventricular septal defect enlargement, and pulmonary artery trunk ligation (video 1 of the supplementary data). Lesion was solved with continuous suture during surgery in the left circumflex coronary artery. Disease progression was good, and the patient remained asymptomatic for the next 7 years with excellent functional capacity and 95% oxygen saturation. At the follow-ups, the echocardiographic presence of severe subvalvular pulmonary stenosis was confirmed with pulmonary artery trunk dilatation and turbulent flow inside. No other findings were reported.
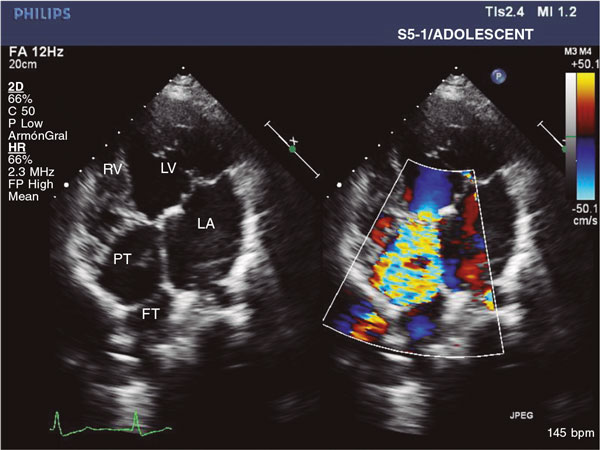
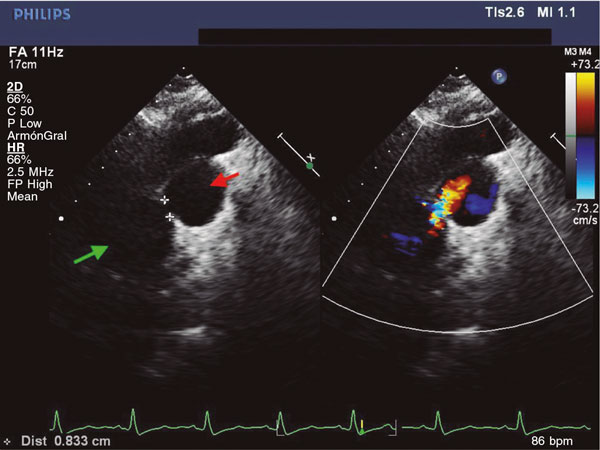
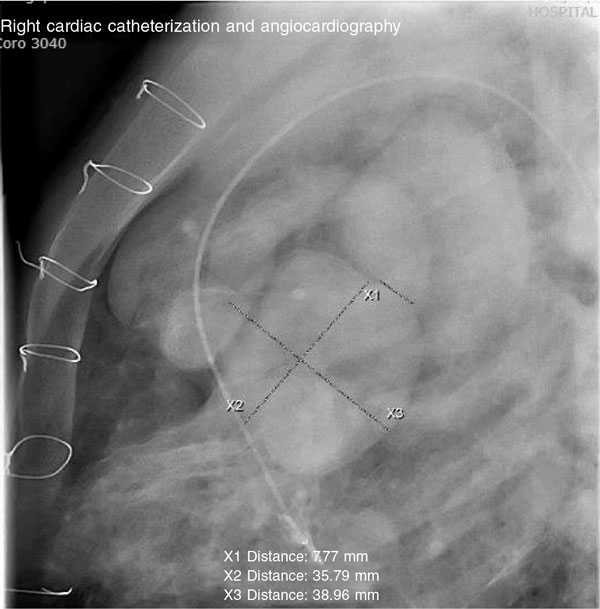
In the clinical examination performed at 14 years, the transthoracic echocardiography revealed the presence of severe subvalvular pulmonary stenosis (figure 1) with a gradient of 90 mmHg through it plus suspected fistulization between the pulmonary artery trunk and Fontan circulation (figure 2) with a pulsatile flow with a maximum systolic gradient of 73 mmHg. Diastolic flow was maintained from the pulmonary artery trunk towards the right atrium while connected to the pulmonary branches. Cardiac catheterization was performed. It revealed a mean Fontan pressure of 16 mmHg and oximeter jump between the pulmonary artery compared to the rest of circulation (91% vs 78%) discarding aortopulmonary collaterality. Ventriculography revealed the presence of severe subvalvular pulmonary stenosis with aneurysmal dilatation of pulmonary artery trunk and presence of a fistula between the trunk and the right pulmonary artery (figure 3 and video 2 of the supplementary data). Also, the presence of a pseudoaneurysm of posterior location and left to the aorta (30 mm x 38 mm) with a wide entry (figure 4 and video 3 of the supplementary data), and calcification in pairs with mobility basically of the posterior wall associated with the coronary event of the surgical procedure.
Figure 1. Echocardiographic apical four-chamber view showing the origin of turbulent flow in the subpulmonary region until the roof of pulmonary trunk. FT, Fontan tube; LA, left atrium; LV, left ventricle; PT, pulmonary trunk; RV, right ventricle.
Figure 2. Echocardiographic right parasternal view showing the connection between the pulmonary trunk and pulmonary circulation with passage of flow. Green arrow: pulmonary trunk. Red arrow: right pulmonary branch.
Figure 3. Lateral angiography in the pulmonary trunk showing the fistula towards the right branch.
Figure 4. Ventriculography showing pseudoaneurysm, pulmonary trunk, and anterior aorta in vessel malapposition with passage of contrast from the pulmonary trunk towards Fontan circulation. X1: fistula between the pulmonary trunk and the right branch. X2 and X3: dimensions of pulmonary trunk.
After the diagnosis of fistula between the pulmonary artery trunk and Fontan circulation plus the left ventricular pseudoaneurysm, a medical-surgical session was presented where the fistula was percutaneously closed and subvalvular pulmonary stenosis was solved. Regarding the pseudoaneurysm, due to the size of the entry orifice, the percutaneous procedure was ill-advised. This, added to serial radiographic stability, suggested the use of conservative approach.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
J.M. Blanco Borreguero drafted and reviewed the manuscript. I. Guillén Rodríguez assisted the patient and supervised the manuscript. L. Marcos Fuentes assisted the patient and provided the images. A. Capilla Miranda drafted and reviewed the manuscript. J.F. Coserria Sánchez supervised the manuscript, assisted the patient, and provided the images.
CONFLICTS OF INTEREST
None reported.
SUPPLEMENTARY DATA
Vídeo 1. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000300
Vídeo 2. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000300
Vídeo 3. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000300