CASE PRESENTATION
The incidence of ST-segment elevation acute myocardial infarction (STEMI) complicated with cardiogenic shock is between 5% and 8% and hospital and long-term mortality is up to three times higher compared to uncomplicated STEMI.
The leading cause of STEMI is the sudden rupture of an atherosclerotic plaque, but there are other less common causes such as cardiac myxoma-induced embolization which, same as it happens with atherosclerotic events, can lead to hemodynamic instability and cardiogenic shock.
We hereby present the case of a 61-year-old male with a past medical history of arterial hypertension and diabetes mellitus type 2 who experienced sudden loss of consciousness in his house; after remaining in this state for 10 minutes, the emergency medical team examined the patient and confirmed that the patient was experiencing confusional state and was hemodynamically unstable (arterial blood pressure, 60/40 mmHg). It was decided to proceed with orotracheal intubation and initiate the infusion of norepinephrine. The electrocardiogram performed confirmed the depression of the ST-segment of up to 5 mm at the inferior-lateral side, which is why the infarction code was activated and the patient was transferred to our center to perform a primary angioplasty procedure.
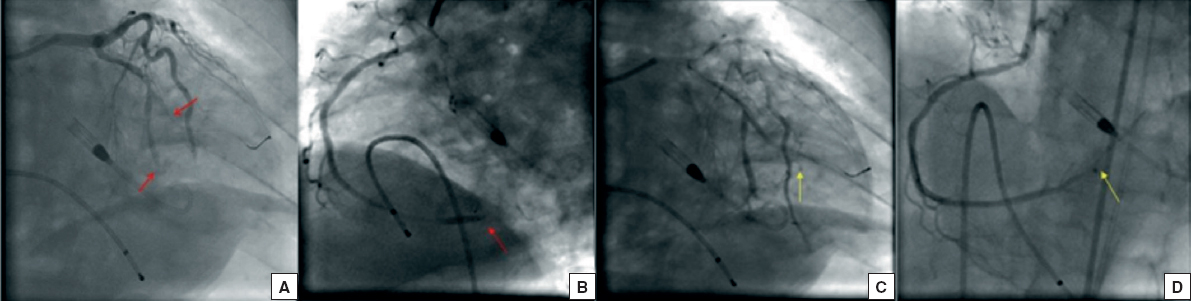
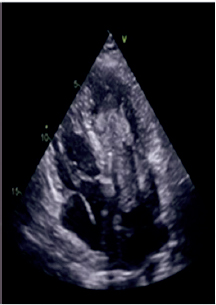
Upon arrival to the cath lab, the patient remained in a state of cardiogenic shock and complete atrioventricular block. A temporary pacemaker was urgently implanted through the right femoral vein and an Impella CP device (AbioMed, Danvers, Massachusetts, United States) was placed in the left ventricle through the left femoral artery. The coronary angiography was performed using the right femoral access and showed an acute embolic-like occlusion of the middle of the circumflex and distal right coronary arteries (figure 1A,B). Thrombus aspiration was performed in both arteries, and abundant thrombotic material was extracted. A simple angioplasty procedure was performed on the distal right coronary artery with suboptimal recovery of epicardial flow (Thrombolysis in Myocardial Infarction ≤ 2) (figure 1C,D). After the procedure, the transthoracic echocardiography performed revealed the presence of an intracavitary mass attached to the left atrial ceiling and spreading towards the left ventricle (figure 2). Given the images available and the patient’s persistent hemodynamic instability despite the vasoactive drugs administered at maximum doses and percutaneous circulatory support, the heart team was activated and a decision was made to implant a extracorporeal oxygenation membrane system percutaneously and remove the Impella CP device.
Figure 1. A: the arrows point at the embolization of the distal circumflex artery. B: the arrow points at the embolization of the distal right coronary artery. C-D: the arrows point at the outcomes of the interventional procedure.
Figure 2. Mass displaced towards the left ventricle.
Prior to the patient’s admission to the cardiac intensive care unit, the computed tomography scan performed on the patient’s brain revealed the total occlusion of intracranial arteries and diffuse cerebral edema. During the patient’s stay at the cardiac intensive care unit, he remained in a state of refractory cardiogenic shock; the new transthoracic echocardiography performed revealed the presence of a tumor in the left atrium causing a double severe mitral lesion (regurgitation and stenosis), and severe left ventricular dysfunction.