HOW WOULD I APPROACH IT?
Currently, the management of thrombosis refractory to IV anticoagulant therapy of heart valves is limited: reintervention or fibrinolysis. Both procedures bring acceptable immediate results, but logically reintervention has a greater impact on the patient’s recovery. Also, the treatment of choice will be influenced by a series of parameters including hemorrhagic risk, the patient’s clinical status, the size of the thrombus, other concomitant findings in the imaging study, etc.
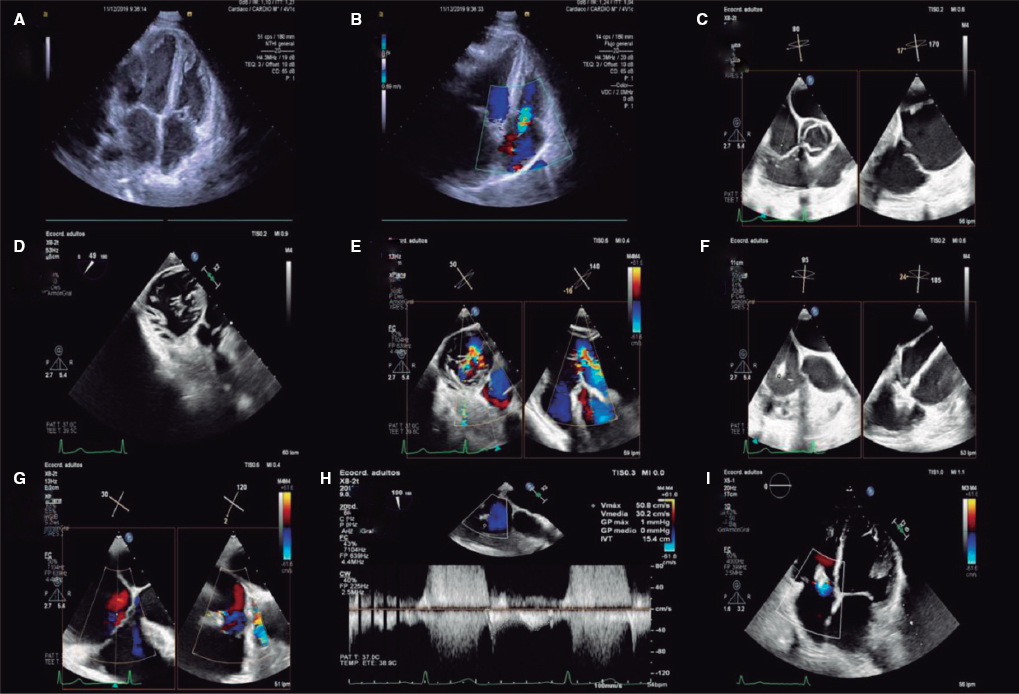
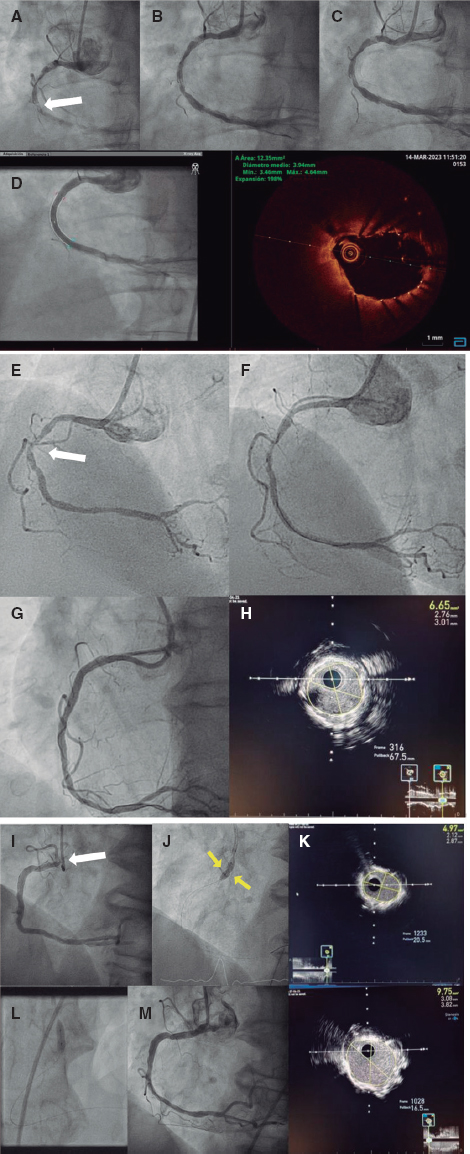
The female patient of this case is young with a mechanical prosthesis in the mitral and aortic position and a second episode of mitral valve thrombosis with serious clinical repercussions. Also, it is a case refractory to pharmacological treatment after reintervention due a first thrombosis of acute presentation (< 3 months after the intervention). This makes us have to consider 2 important details before moving on with the possible percutaneous treatment: could this be a case of endocarditis with an added thrombus? and also, is this the case of a patient with some sort of refractoriness to antithrombotic treatment? I am exposing this because, in both cases, the percutaneous therapeutic strategy did not seem like the optimal strategy to me. Since thrombotic content was not massive here, the first step in the percutaneous strategy should have been to regain the mobility of the prosthetic valve hemidiscs. It is somehow logical to think of regaining their movement: the best fibrinolytic agent is flow and the movement of the valve. Also, it is the cause of symptom onset. Percutaneous treatment has the limitation of the potential embolization of the attached thrombotic material. The idea of the percutaneous manipulation of the prosthetic valve discs was already described by Jabbour et al.1 back in 1996 as bridging therapy to reintervention. However, the greater experienced ever reported in the current medical literature is Hariram’s2 who described 5 cases of immobile prosthetic discs that were manipulated or limited in their atrial side using a Judkins Right guide catheter through a Mullins transseptal introducer sheath. The consensus achieved at the congress held by the American College of Cardiology in 2018 introduced the first case of a young female patient in whom transseptal access was also used to insert a deflectable Agilis introducer sheath (Abbott Cardiovascular, Sta. Clara, United States) by contacting an Amplatz Super Stiff guidewire (Boston Scientific, Marlborough, MA, United States) directly into the prosthetic valve. None of the cases reported developed embolic complications and all of them regained the disc movement in the mitral position. We have no further information on these patients’ clinical progression.
In our setting it seemed reasonable for me to suggest the following percutaneous access: radial access to control the central arterial pressure with a 5-Fr pigtail catheter (it is still a mark for transseptal access), venous access to perform a transseptal puncture trying a preferably posterior puncture with the deflectable Agilis NxT introducer sheath (Abbott Cardiovascular, Sta. Clara, United States), and contralateral venous access to guide the transseptal access with an intracavitary ultrasound. Both the puncture and the regain of disc mobility can be performed through transesophageal ultrasound guidance, which also facilitates residual thrombus comparison after finishing the maneuver. The patient’s clinical status is key regarding the decision of using one technique over the other. Theoretically speaking, a Judkins Right guide catheter (due to the location of the immobile disc) followed by active aspiration (a 50 mL Luer-Lock syringe directly connected to the catheter that a second operator can traction to perform the aspiration) can be used to safely cross the valve and smoothly impact the atrial surface of the prosthesis, the annulus or the disc until mobility is regained. We should not forget that the procedure should be performed with anticoagulation to keep the activated clotting time, at least, above 250 seconds in a patient operated on and who has been treated with fibrinolysis; that is why transseptal guidance seems important to me. Although according to the image the size of thrombosis seems limited, I would be suggesting protection against possible cerebral embolizations with a Sentinel device (Boston Scientific, Marlborough, MA, United States) via right radial access. Protection with a balloon inflated at left subclavian and other visceral branch level like the mesenteric branches seems optional to me given the size of the current thrombus. If the maneuver with the Judkins Right guide catheter fails, I think it would be safer to try with catheter tips of different shapes and, eventually, with a second pigtail catheter mounted over a guidewire to change the curve rather than the strategy of using guidewires to impact the discs. It is essential that the neuroradiology and angioradiology teams of our center are involved in this process.
We should mention that in the case presented here it is expected that percutaneous resolution will be a bridging therapy until the endothelization of the area of the prosthetic valve annulus can stop a third thrombosis from happening. Currently, pharmacological treatment with vitamin K antagonists is the right one. Due to the pathogenesis of this type of thrombosis where the intrinsic pathway is activated, antiplatelet therapy does not seem to play a key role and direct anticoagulants are ill-advised to prevent prosthetic valve thrombosis from happening (the REALIGN study). Finally, it is obvious that a strict clinical follow-up is required including a transesophageal ultrasound 1 month after the procedure with regular assessments of the international normalized ratio (to keep it between 3 and 3.5). The recurrence of thrombosis would make us have to rethink a third mitral valve replacement surgery and reconsider the type of prosthetic valve used. Biological valves in the mitral position are associated with a lower rate of thrombosis compared to mechanical prostheses. The downside of early degeneration in young patients should be compensated with that of recurrent prosthetic valve thrombosis. Also, thrombosis on a biological valve would be eligible for treatment with transcatheter valve implantation.3
FUNDING
No funding was received for this work.
CONFLICTS OF INTEREST
None declared.
REFERENCES
1. Jabbour S, Saldinger M, Alexander JC. Hemodynamic stabilisation of acute prosthetic valve thrombosis using percutaneous manipulation. Catheter Cardiovasc Diagn. 1996;39:e314-e316.
2. Hariram V. Percutaneous Management of Prosthetic Valve Thrombosis. Indian Heart J. 2014;66:427-429.
3. UnzuéL, García E, Rodríguez Rodrigo FJ. Percutaneous treatment of prosthetic mitral valve thrombosis. Rev Esp Cardiol. 2020;73:500.
Corresponding author: Unidad de Cardiología Intervencionista, Hospital Universitari Vall d’Hebron, Passeig de la Vall d’Hebron 119-129, 08035 Barcelona, Spain.
E-mail address: brunogb51@gmail.com (B. García del Blanco).