CASE PRESENTATION
Fifty-three-year-old woman with dyslipidemia who was admitted due to effort angina of 1-week duration and an episode of angina at rest the night before. The electrocardiogram did not show any repolarization alterations. Troponin T levels were measured with a 4-h interval and they duplicated the normal reference levels (28 ng/L, 31 ng/L; normal reference value: 0-14 ng/L). Initially, acetylsalicylic acid was administered (300 mg). That same morning an exercise testing was conducted that turned out clinically inconclusive and electrically non-assessable to rule out ischemia because it did not reach 85% of the theoretical maximum frequency.
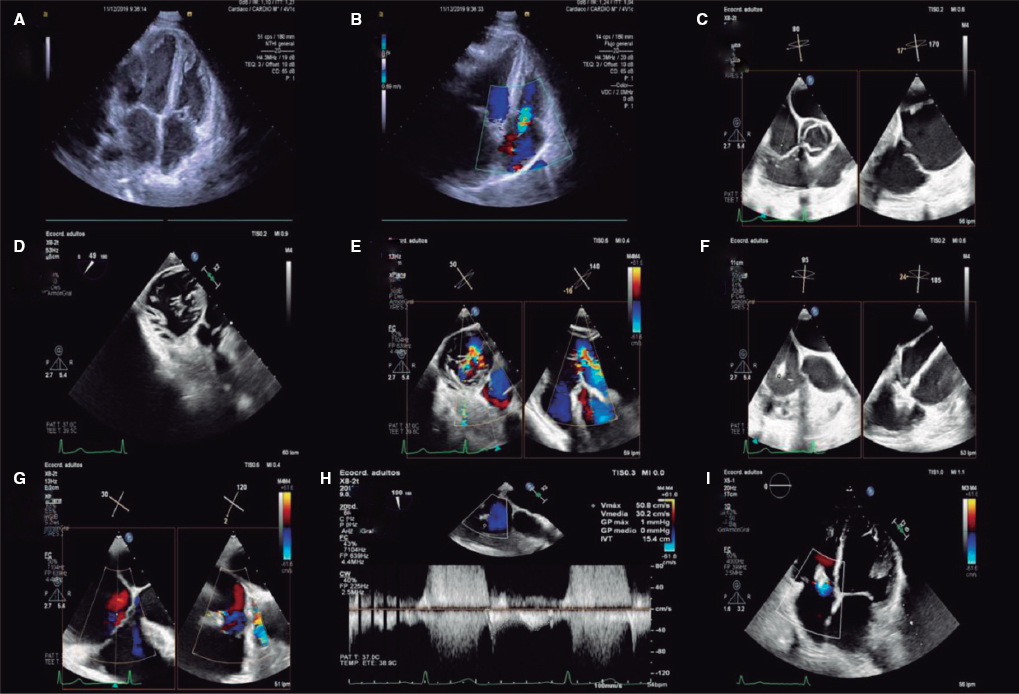
The coronary angiography showed non-significant angiographic lesions in the anterior descending and circumflex arteries. The right coronary artery (RCA) showed a severe lesion in its middle segment. Taking into consideration that therapy with only acetylsalicylic acid was used, the patient’s clinical manifestations at rest, and the markers on borderline significance it was decided that the patient was suffering from unstable angina and a loading dose of ticagrelor (180 mg), a bolus of tirofiban (25 µg/kg, without infusion), and heparin (70 U/kg) were administered. A 3.5 x 24 mm drug-eluting stent was deployed in the middle RCA with optimal results (figure 1).
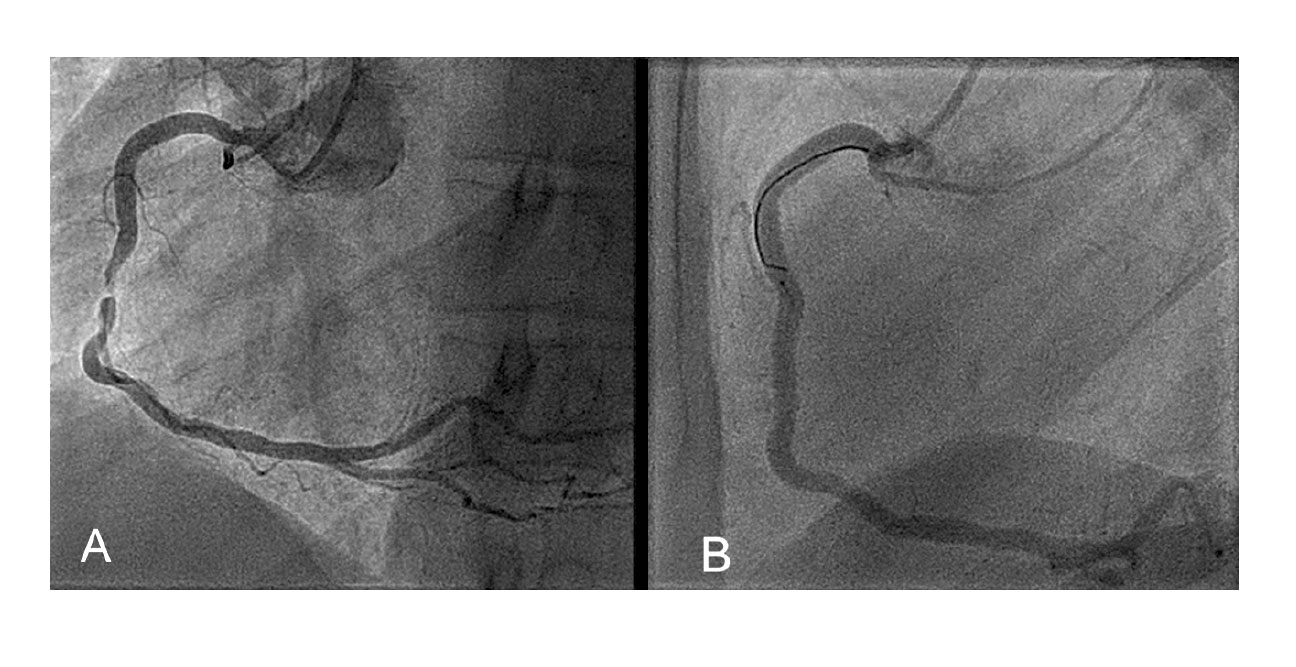
Figure 1. Right coronary artery before (A) and after deploying the 3.5 x 24 mm stent (B)
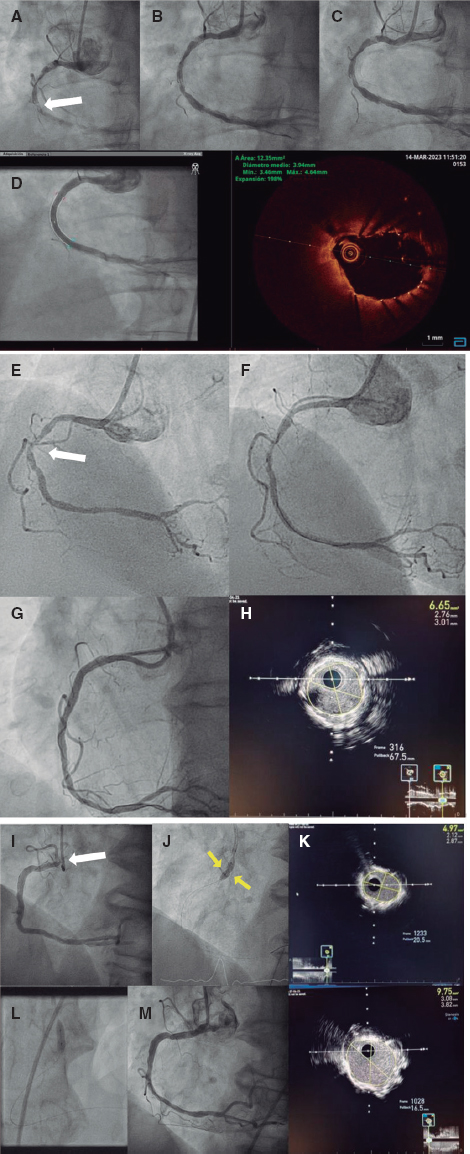
Forty minutes after the procedure, the patient started experiencing chest pain and ST-segment elevation in the inferior leads, which is so a new cardiac catheterization procedure was conducted that confirmed the presence of an occlusion distal to the stent. On suspicion of dissection/hematoma, a intravascular ultrasound study was conducted that confirmed the presence of a wall hematoma from the stent towards the posterior-posterolateral (PL) descending bifurcation (figure 2).
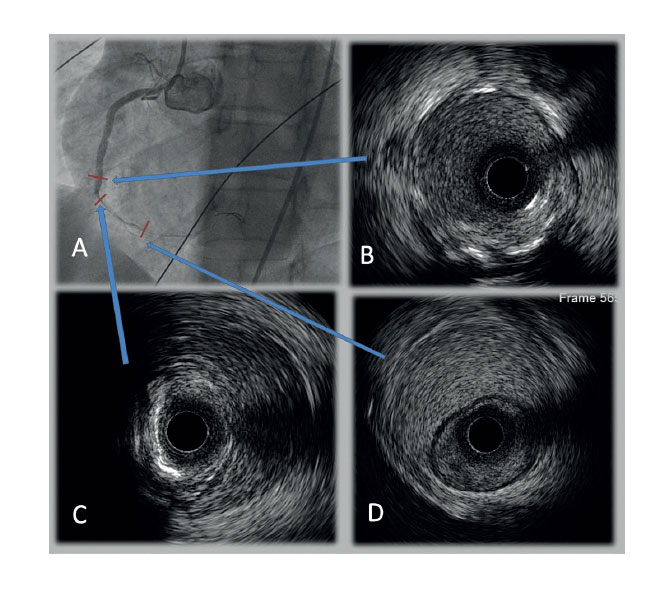
Figure 2. Angiography (A) and intravascular ultrasound imaging, in-stent (B), distal stent margin (C) and in distal right coronary artery (D).
Initially, a 3 x 20 mm drug-eluting stent was implanted overlapping the stent deployed in the middle RCA, but since the RCA distal occlusion was persistent, another 2.25 x 26 mm overlapping stent had to be implanted distally with which the hematoma progressed towards the PL and occluded the posterior descending artery. Then we proceeded with the overlapping deployment of another 2 x 30 mm drug-eluting stent from the distal RCA towards the PL resulting in recovered TIMI (Thrombolysis in Myocardial Infarction) flow 3 in the PL with still a persistent occlusion of the posterior descending artery. The stents of the distal CRA and PL have a smaller caliber compared to the initial vessel lumen in order to avoid the distal progression of the hematoma (figure 3). Although the stents are apposed to the endothelium, the intravascular ultrasound imaging shows that the distance from the stent to the blood vessel middle layer is 1 mm.
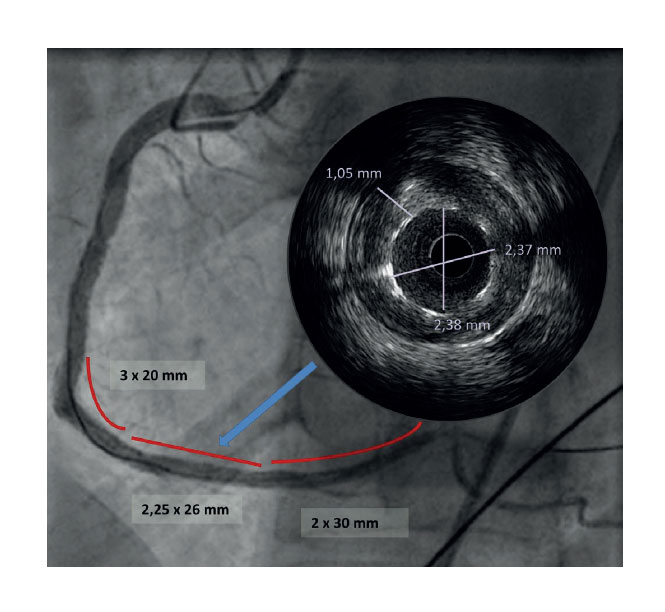
Figure 3. Final result after implanting three drug-eluting stents (lines) in the posterolateral right coronary artery.
Although both the symptoms and the ST-segment elevation persisted, the procedure was completed due to the risk of the hematoma progressing even more distally towards the PL and the impossibility to re-cross the guidewire towards the posterior descending artery.
The electrocardiogram that followed the procedure showed the persistence of the ST-segment elevation in the inferior leads; 3 h after the procedure the patient’s pain improved and the ST-segment became normal. Considering that an excess of antiplatelet therapy could have favored the appearance of hematoma, it was decided to switch from ticagrelor to clopidogrel.
Afterwards, the patient remained asymptomatic and with an enzyme reaction progress curve with peak troponin T levels at 24 h (4490 ng/L, 4a-type myocardial infarction). The echocardiogram showed a non-dilated left ventricle at discharge with preserved global systolic function, and inferior segments and basal posterior segment hypokinesia.
E-mail address: laura.sarnak@gmail.com (L. Mañas Alonso).