The authors present the case of a preterm baby of 27 + 5 weeks of gestational age and 990 grams of body weight at birth. After an IV dose of ibuprofen to treat a ductus arteriosus with hemodynamic repercussion, a serious femoral pulse wave attenuation occurred with a systolic gradient of 60 mmHg in the aortic isthmus as seen on the Doppler ultrasound followed by significant diastolic prolongation of forward flow, and distal transverse arch hypoplasia. The diagnosis was severe aortic coarctation (AoC). Treatment was initiated with prostaglandins. Still, the arm-leg blood pressure gradient increased until the patient’s condition got worse on his 13th day of life with a body weight of 1200 grams. Also, the patient’s hemodynamic status got worse with severe left ventricular dysfunction and dilatation refractory to high-frequency ventilation and inotropic support with dobutamine.
The surgical approach of severe AoC in newborn babies with body weights < 2000 grams, especially in situations of multiorgan failure and coagulopathy, is often discarded in most centers because of the poor short and mid-term results; also, the incidence of brain injuries is very high. Over the last few years, balloon angioplasty has become a very popular bridging therapy to treat severe AoC in newborn babies. However, the incidence of a new AoC is fairly high.
Isolated, still promising, experiences have been published over the years regarding coronary stent implantation to treat AoC in newborn babies. This procedure has reduced the rate of new AoC significantly, postponed surgery until the baby’s age and weight are more suitable, and facilitated the expansion of the transverse arch within the first months of life, thus reducing the need for more aggressive surgeries to expand the arch.1
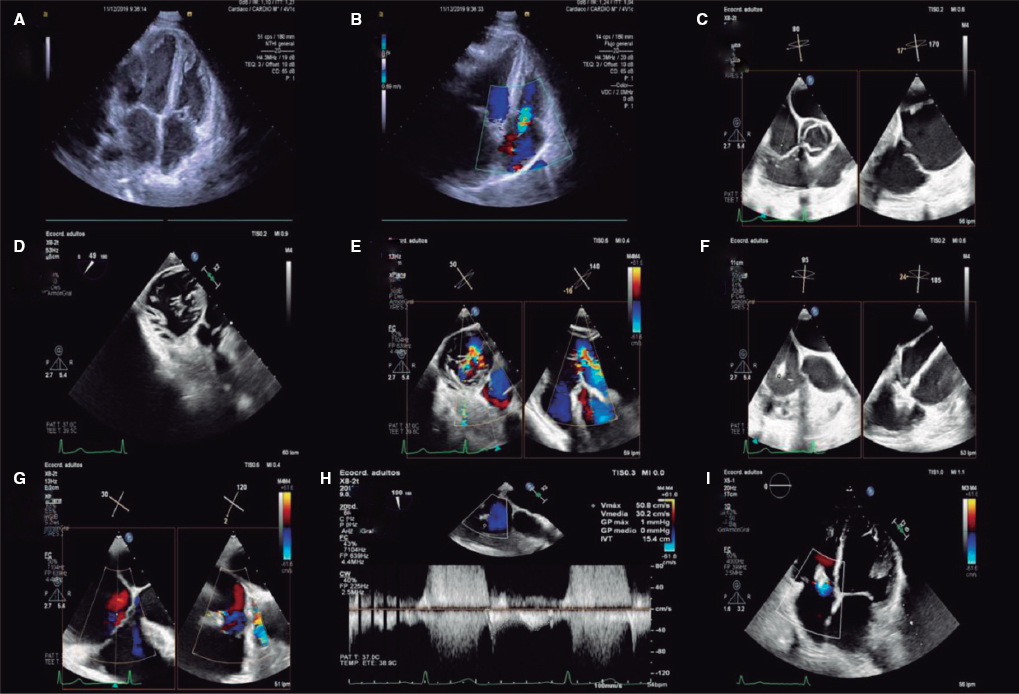
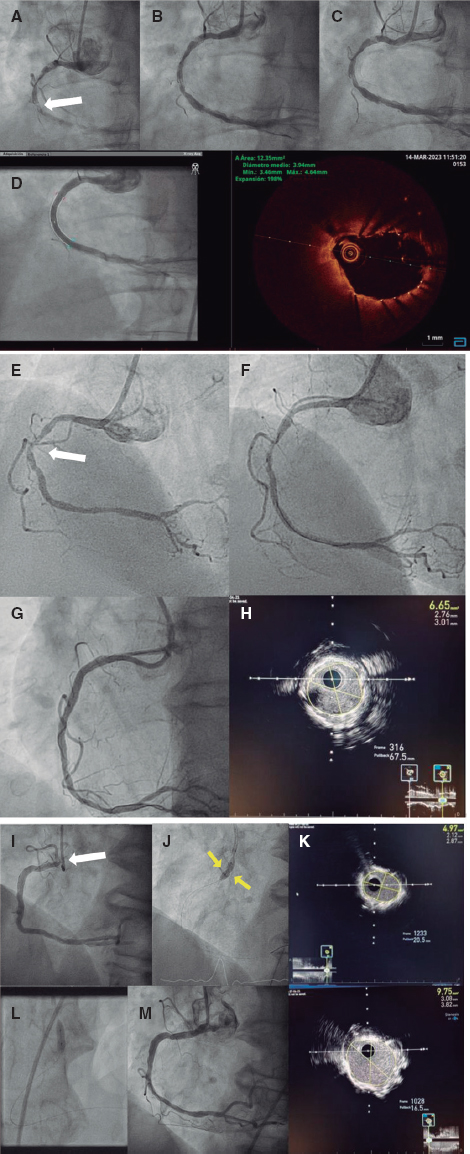
However, retrieving a bare metal stent from the arch is not always easy. Our group has published the series with the largest number of pediatric patients to this date whose different vascular injuries were treated by implanting the Absorb bioresorbable coronary stent (Abbott, United States) built from a kind of lactic acid polymer. This series included a patient with 2.3 kilos of weight, AoC, and hemodynamic deterioration who received a 3.5 mm × 12 mm Absorb device. The patient was operated on 155 days later with termino-terminal anastomosis. The surgeons had no difficulty moving the structures and found no traces of any foreign material (figure 1). The resorption of this type of stent is associated with the absorption of water by the lactic acid in its structure. Usually, in adults the resorption of the stent occurs 2 years after the intervention. The fastest resorption reported in babies (in our patients after 5 months) may be due to the exposure of the endoprosthesis to higher blood flows in relation to coronary flow.2 After this first case, our hospital has treated another 2 newborn babies with weights < 2000 grams and severe AoS through angioplasty with an Absorb device. Both patients underwent surgery 2 to 4 months later with good results. The consent necessary to carry out the procedure was obtained and the parents gave their consent for the reproduction of the images for scientific dissemination.

Figure 1. Aortic coarctation (AoC) treated with angioplasty and implantation of a 3.5 mm × 12 mm Absorb stent via carotid access in a newborn baby of 1400 grams of body weight. A: baseline angiographic measures; AoC, 1.2 mm; transverse arch, 2.2 mm; downstream aorta, 2.7 mm. B: angiography prior to implantation. C: result of the implant.
Unfortunately, we have not added more patients to this registry because the Absorb stent was removed from the market due to its unsatisfactory results treating coronary injuries. However, Sallmon et al.3 have recently published the case of a newborn baby of 2100 grams of body weight and severe AoC implanted with a Magmaris bioresorbable coronary stent (Biotronik, Germany) with good results. It seems that the use of bioresorbable stents for the management of AoC in newborn babies is still promising because it improves the results of plain angioplasty and avoids the inconveniences associated with bare metal stents in postponed surgeries.
Therefore, the therapeutic approach in this patient would be to implant a bioresorbable stent. We would proceed with the surgical dissection of the right carotid artery followed by catheterization with a 5-Fr introducer sheath. Carotid access through dissection is our first option in patients < 3 kilos of weight who require aortic arch or aortic valve interventions since the incidence of vascular complications is lower. Also, it decreases the x-ray imaging exposure time.1 The position of the tip of the introducer sheath would be verified under x-ray guidance and the downstream aorta would be catheterized using a 0.014 inches hydrophilic guidewire. Then, a 3.5 mm × 12 mm Magmaris stent would be mounted on the guidewire through the hemostatic valve. The introducer sheath side port would be used to perform the manual angiographies to check the position of the stent with respect to the AoC. The stent would progressively be dilated with increases of 2 atmospheres at a time until reaching 10 atmospheres. In the end, the final structural result would be tested on an angiography and the hemodynamic results on a transthoracic color Doppler echocardiography. This is how to avoid recrossing the stent with catheters and minimize the risk of stent displacement. At the end of the procedure, the surgical reconstruction of the carotid artery would be attempted (video 1 of the supplementary data).
FUNDING
No funding was received for this work.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Zunzunegui Martínez JC. DOI: 10.24875/RECICE.M20000189
REFERENCES
1. Lucas V. Stent treatment of neonatal coarctation:another option for critically ill or extremely small patients with unoperated coarctation or failed surgery. Catheter Cardiovasc Interv. 2010;75:562.
2. Rodríguez Ogando A, Ballesteros Tejerizo F, Sarnago Cebada F, Medrano López C, Gil Jaurena JM, Zunzunegui Martínez JL. Experience With the Absorb Bioresorbable Vascular Scaffold in Various Scenarios of Congenital Heart Disease. Rev Esp Cardiol. 2018;71:988-990.
3. Sallmon H, Berger F, Cho M-Y, Opgen-Rhein B. First use and limitations of Magmaris®bioresorbable stenting in a low birth weight infant with native aortic coarctation. Catheter Cardiovasc Interv. 2019;93:1340-1343.
Corresponding author: Unidad de Hemodinámica Pediátrica, Hospital Gregorio Marañón, Dr. Esquerdo 46, 28007 Madrid, Spain.
E-mail address: zunzu69@hotmail.com (J.L. Zunzunegui Martínez).