ABSTRACT
Introduction and objectives: Recipients of a heart transplant need to receive serial endomyocardial biopsies (EMB) to discard rejection, a procedure that is usually performed through the femoral or jugular vein. Over the last few years, we have developed a technique to perform EMBs using the brachial venous access that we have implemented as the preferential access route. In this article, we describe the technique and the initial clinical experience of 2 different centers.
Methods: Between 2004 and 2016, we developed and implemented a brachial venous access technique. We registered the main clinical and procedural variables of all the brachial biopsies performed in both centers and compared them with a retrospective series of femoral and jugular procedures.
Results: Brachial EMBs were successfully performed 544 of the time with no major complications. The number of brachial procedures per patient rose from 1 to 14. Over the same period of time 1054 femoral and 686 jugular procedures were performed. The total procedural time was similar with different access routes (mean for brachial/femoral/jugular access: 28/26/29 min., P = .31) while fluoroscopy time was shorter in jugular procedures (mean 5/5/3 min. respectively; P < .001). The brachial procedure was recalled as the least painful procedure of all compared to the jugular or femoral ones (2/8/9 score on a scale from 1 to 10; P = .001) with an overall patient preference towards the brachial access.
Conclusions: The venous brachial access route is a good alternative to the central venous one to perform EMBs and is the route of choice in our centers. Also, it has high feasibility and safety and brings additional comfort to patients.
Keywords: Endomyocardial biopsy. Heart transplant. Brachial access.
RESUMEN
Introducción y objetivos: Los pacientes receptores de un trasplante cardiaco necesitan someterse a biopsias endomiocárdicas (BEM) para descartar el rechazo, procedimiento que habitualmente se realiza por acceso venoso yugular o femoral. En los últimos años hemos desarrollado una técnica de biopsia por vía braquial, que hemos implementado como acceso preferente. En este artículo describimos la técnica y la experiencia clínica inicial de 2 centros empleando el acceso braquial.
Métodos: Entre 2004 y 2016 desarrollamos e implementamos la técnica de biopsia por vía venosa braquial. Se registraron las principales variables clínicas y del procedimiento de todas las BEM realizadas por vía braquial en ambos centros, y se compararon las características con los procedimientos realizados por vía femoral y yugular.
Resultados: Se realizó la BEM por vía braquial en 544 casos, sin complicaciones mayores. El número de procedimientos braquiales por paciente varió entre 1 y 14. En el mismo periodo se realizaron 1.054 BEM femorales y 686 yugulares. La duración total del procedimiento fue similar por los distintos accesos (mediana braquial/femoral/yugular: 28/26/29 min; p = 0,31), con un menor tiempo de escopia por vía yugular (mediana 5/5/3 min, respectivamente; p < 0,001). Los procedimientos realizados por vía braquial se valoraron como menos dolorosos que los realizados por vía yugular o femoral (2/8/9 en la escala de dolor EVA de 1-10, respectivamente; p = 0,001), y fue la vía de elección por parte de los pacientes.
Conclusiones: La BEM por vía venosa braquial es una buena alternativa a la punción venosa central y la vía de elección en nuestros centros, con altas factibilidad y seguridad, y mayor comodidad para el paciente.
Palabras clave: Biopsia endomiocárdica. Trasplante cardiaco. Acceso braquial.
Abbreviations: EMB: endomyocardial biopsy. RHC: right heart catheterization. RV: right ventricle.
INTRODUCTION
Endomyocardial biopsy (EMB) is an invasive procedure usually performed using central venous access to obtain samples of the interventricular septum from the right ventricle (RV).1,2 Its main indication is for heart transplant recipients who need repeated EMBs to discard organ rejection despite immunosuppressive therapy.3 Less frequently, the EMB is also used as a diagnostic tool with certain heart diseases like myocarditis or suspected infiltrative disease,4 scenarios where the arterial femoral or radial approach may also be considered to access the left ventricle.5,6
EMBs are often performed through central venous access, femoral or jugular access;2-4 although it is a safe technique, it is associated with a risk of vascular or nerve damage that is inherent to jugular or femoral punctures.7
The forearm veins may be a good alternative access route to perform EMBs with the potential advantage of increased vascular safety and more comfort to the patient (figure 1). Basilic and cephalic veins are superficial veins that converge at the subclavian vein, superior cava vein, and ultimately right heart. However, the use of this access route known by the generic term “brachial” to perform EMBs is rare and, to this day, has been reported in one series only.8
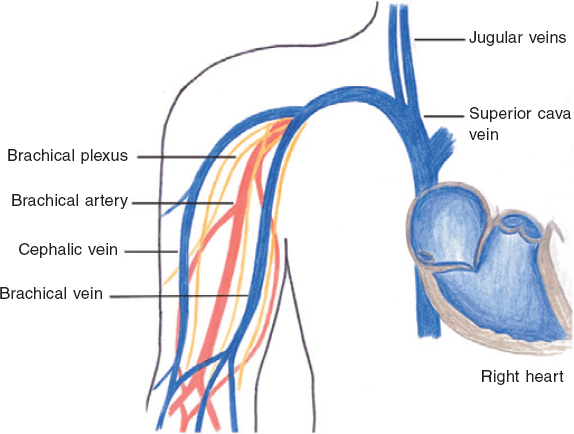
Figure 1. Schematic representation of the anatomy of the superficial veins of the arm, forearm and surrounding structures.
In our centers we have developed a new technique to perform EMBs through the brachial vein that we have been using since 2004. The main objective of this manuscript is to describe our technique to perform EMBs through brachial venous access, and the feasibility, safety, and efficacy reported by 2 different centers; our secondary objective was to compare the performance of the brachial route to that of conventional femoral and jugular access routes.
METHODS
Brachial biopsy technique
We have spent over 12 years modifying our technique in 2 different centers since we first described it,9 and have used different catheters and forceps to overcome the main difficulty we have encountered: the lack of devices specifically developed for this purpose. What follows is a description of the approach that has become predominant in our clinical practice.
After the identification of a large brachial vein, preferably the basilic vein over the cephalic one, we prepare a sterile field and puncture the vein with a regular venous catheter (18 gauge or larger) to allow the insertion of the sheath and guidewire. This first step used to be performed by our nursing team. When a vein was not readily visible or palpable, the physician in charge would perform an ultrasound-guided puncture to select the highest caliber vein. Similarly, when the standard puncture failed or if we knew of failed prior attempts or there were signs indicative that the veins had been punctured multiple times like bruising and scarring we used ultrasound guidance. The addition of ultrasound guidance has been gradual since 2015, and it has significantly increased the percentage of patients considered eligible to receive an EMB through brachial access. Once punctured, the vein is wired using a standard 0.035 in J wire, local anesthetics are administered, and a 7 Fr sheath is inserted. Afterwards, a long 0.035 in J wire is advanced and over the wire, a 7 Fr multipurpose guide catheter is positioned towards the right ventricle of the interventricular septum using fluoroscopy guidance. When the J wire could not be advanced easily often due to a venous valve or an occluded or spastic vein, a hydrophilic guidewire or a coronary 0.014 in guidewire was used.
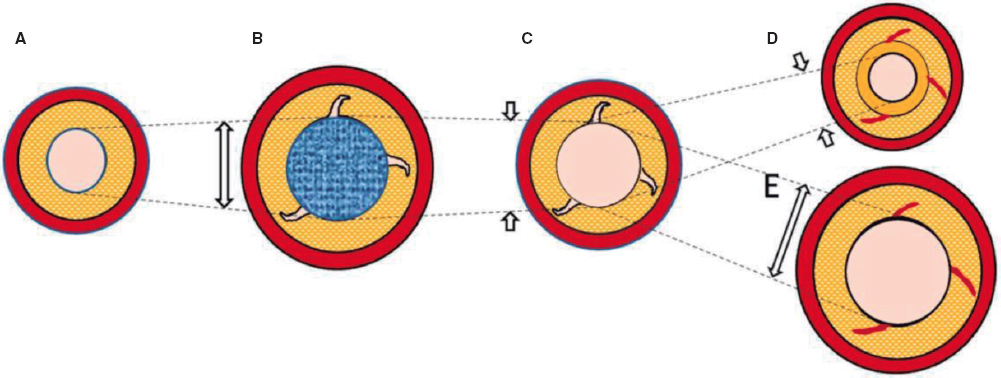
Regarding the biopsy, we used a long forceps (104 cm; Cordis, Johnson & Johnson, United States) that comes in 2 different sizes: 5.5 Fr (142 cases) and 7 Fr (402 cases). Since the guide catheter is longer compared to the biopsy forceps we made it shorter by cutting the proximal 5 cm to 10 cm. To prevent bleeding or air embolism during manipulation, a 7 Fr femoral sheath can be used to seal the proximal end of the catheter. To facilitate the advance of the forceps through the tricuspid valve and prevent it from acquiring caudal orientation we shaped its distal end with a curve. Once the delivery catheter was in place we inserted the forceps, checked the septal orientation with fluoroscopy, and took 3-6 samples as usual. Figure 2 shows the main steps of this technique. The procedure was considered successful when an adequate sample was obtained and no major complications occurred. The inability to advance the J wire or the guide catheter that would eventually lead to change the access route was considered a failure.
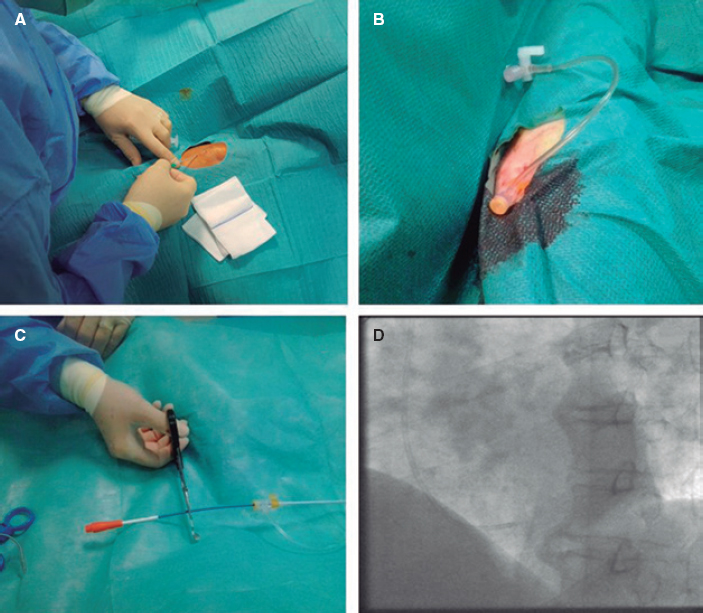
Figure 2. Step-by-step procedure of a brachial endomyocardial biopsy. A: a basilic or cephalic vein is identified and punctured with an 18-gauge venous catheter. B: the vein is wired for the insertion of a 7 F sheath. C: a multipurpose 7 Fr guide catheter is advanced over a J wire and the proximal 5 cm-to-10 cm are cut. D: the catheter is inserted into the right ventricle, and its septal orientation is checked through fluoroscopy before inserting the forceps.
After the procedure and only if the patient needed right heart catheterization it was performed through the same vein. If the patient needed an additional coronary angiography, the arterial access route, preferably radial, was canalized. Finally, we extracted both the catheter and the sheath and left a gentle elastic compression for 2 hours. No bed rest was required after the EMB procedure.
Data collection and analysis
We retrospectively collected the demographics, main procedural characteristics, and immediate and 48 h complications of all consecutive patients admitted to our catheterization laboratory to receive EMB from August 2004 through April 2016. Major complications were defined as death, major bleeding, pneumothorax, stroke, and cardiac tamponade. We compared the characteristics of brachial procedures to those of a series of biopsies performed through the jugular or femoral access route. We retrospectively contacted a sample of patients who had received the procedure through 2 different venous routes (brachial and central venous access) and asked them to rate the pain experienced during the procedure on a scale from 1 to 10. Also, to state their preferred venous access for the future.
Statistical analysis was performed using R 3.2.3. Data were expressed as mean ± standard deviation, median (interquartile range) or number (percentage). Inter-group differences were studied using the unpaired Student t test, the Wilcoxon rank sum test, Kruskal-Wallis test or the chi-square test as appropriate.
RESULTS
Brachial biopsy population
Between August 2004 and April 2016 we performed a total of 544 brachial EMBs in 118 patients. Mean age of the cohort was 52 ± 13 years; 12% of the patients were female. The reason for the biopsy was post-transplant follow-up in 525 procedures (96.5%) and cardiomyopathy assessment in the remaining patients. The veins used for the procedure were the basilic (90%) and the cephalic (10%) veins; the right arm was more commonly used (74%). The number of brachial procedures per patient rose from 1 to 14 (mean of 5 [1-10]). In 71 cases (13% of the procedures) right heart catheterization (RHC) was performed too, and in 82 cases (15%) a coronary angiography was performed. In these procedures most of the coronary angiographies were performed through the radial or ulnar arteries (92%). Fifty-seven-point-four percent of the cases were outpatient procedures. No major complications were reported.
The brachial approach failed in 33 cases, always due to the impossibility to wire the vein or advance the catheter so we had to change the access route. Success rate for brachial EMBs was 94%. The percentage of ultrasound-guided procedures varied between both centers; we found that after its routine use in 1 center the brachial approach success rate has gone up up to 98.4% since 2015.
Venous access comparison
A total of 2284 biopsies were included in the registry from August 2004 through April 2016: 1054 femoral, 686 jugular, and 544 brachial. The main reason to perform this procedure was heart transplant in the 3 cohorts (P < .001). The patients’ clinical characteristics were similar except for brachial procedures that were less common in women (13% vs 26%, P < .001). Most of the patients were outpatient cases in all the groups (61% of the total procedures) who did not require hospitalization. The main clinical characteristics are shown on table 1.
Table 1. Demographics and baseline characteristics of jugular, femoral and brachial patients
| Jugular (n = 686) | Femoral (n = 1054) | Brachial (n = 544) | P | |
|---|---|---|---|---|
| Age (years) | 51 ± 13 | 52 ± 14 | 52 ± 13 | .38 |
| Women | 175 (25.5) | 257 (24.4) | 66 (12.1) | < .001 |
| Hypertension | 275 (46.6) | 444 (48.8) | 253 (52.7) | .14 |
| Hyperlipidemia | 218 (36.8) | 384 (42.6) | 195 (40.9) | .08 |
| Diabetes | 152 (31.1) | 269 (31.8) | 137 (34.7) | .49 |
| Reason for biopsy | < .001 | |||
| Heart transplant | 677 (98.7) | 989 (93.8) | 525 (96.5) | |
| Cardiomyopathy | 9 (1.3) | 65 (6.2) | 19 (3.5) | |
| Patient destination | .017 | |||
| Outpatient | 414 (60.3) | 666 (63.2) | 312 (57.3) | |
| Inpatient | 253 (36.9) | 336 (31.9) | 206 (37.9) | |
| Nonspecific | 19 (2.8) | 52 (4.9) | 26 (4.8) | |
Data are expressed as no. (%) and mean ± standard deviation. |
Success rate was 96.7% for jugular procedures, 99.8% for femoral procedures, and 93.9% for brachial procedures. Crossover to a different access route was required in 33 brachial cases (19 to femoral and 14 to jugular), 2 femoral cases, and 22 jugular cases (P < .001). Patients in whom the brachial access failed were similar to the remaining patients of the cohort: 12% were women with a mean age of 56 years [46-62] and 94% were heart transplant recipients. Seventeen (51.6%) out of the 33 failed procedures occurred during the early experience (between 2004 and 2007). Procedural characteristics are shown on table 2.
Table 2. Procedural characteristics
| Jugular (n = 686) | Femoral (n = 1054) | Brachial (n = 544) | P | |
|---|---|---|---|---|
| Systolic BP (mmHg) | 148 ± 25 | 147 ± 24 | 140 ± 24 | .01 |
| Diastolic BP (mmHg) | 79 ± 14 | 82 ± 14 | 77 ± 13 | .03 |
| Procedural success | 664 (96.7) | 1052 (99.8) | 511 (93.9) | < .001 |
| Crossover | 22 | 2 | 33 | < .001 |
| Brachial to femoral | 19 | |||
| Brachial to jugular | 14 | |||
| Femoral to jugular | 2 | |||
| Jugular femoral | 22 | |||
BP, blood pressure. Data are expressed as no. (%) and mean ± standard deviation. | ||||
We compared total procedural and fluoroscopy times among different venous routes. Total procedural time for biopsy alone was similar among the groups (mean for brachial/femoral/jugular: 28/26/29 min., P = .31); however, fluoroscopy time was the shortest of them all in jugular procedures (mean 5/5/3 min., respectively; P < .001). Additional RHC or coronary angiography were performed less frequently in the jugular cohort (P < .001 in both cases).
Together with RHC, the total procedural time was longer in the brachial route compared to the central one (P = .004); however, fluoroscopy time was longer in the femoral cohort compared to both the brachial (P = .003) and the jugular (P < .001) cohorts.
When the EMB was combined with coronary angiography, procedural times were again longer in the brachial group (brachial/femoral/jugular: 66/59/61 min., P = 0.02), but they were only statistically significant with femoral times (P = .022); also, longer fluoroscopy times were required in the brachial compared to jugular access (P = .002), but not in the femoral access (P = .6). Table 3 and figure 3 show the total and fluoroscopy times per procedure alone and combined with RHC or angiography. When we compared our experience with brachial EMBs half way and then over the last half we saw a reduction in the total procedural time (30 min. vs 28 min., P = .366) and total fluoroscopy time (6.6 min. vs 6.0 min., P = .031).
Table 3. Procedure and fluoroscopy times grouped by access and procedures
| Jugular (n = 686) | Femoral (n = 1054) | Brachial (n = 544) | P | |
|---|---|---|---|---|
| EMB only | ||||
| Number of cases | 596 (86.9) | 738 (70) | 394 (72.4) | < .001 |
| Procedural time | 29 [20-40] | 26 [20-37] | 28 [19-40] | .31 |
| Fluoroscopy time | 3 [2-5] | 5 [3-8] | 5 [3-7] | < .001 |
| EMB + RHC | ||||
| Number of cases | 46 (6.7) | 131 (12.4) | 69 (12.7) | < .001 |
| Procedural time | 43.5 [32.75-63.5] | 43.5 [37-54.75] | 51 [45-63.5] | .004 |
| Fluoroscopy time | 3 [2-5.5] | 11 [7.75-15.25] | 7 [6-11] | < .001 |
| EMB + CA | ||||
| Number of cases | 44 (6.4) | 185 (17.6) | 81 (14.9) | < .001 |
| Procedural time | 61 [52-77.5] | 59 [46-70] | 66 [53-87] | .019 |
| Fluoroscopy time | 8 [7-18] | 12 [8-17] | 14 [10-19] | .003 |
Data are expressed as median [interquartile range] and no. (%). CA, coronary angiography; EMB, endomyocardial biopsy; RHC, right heart catheterization. | ||||
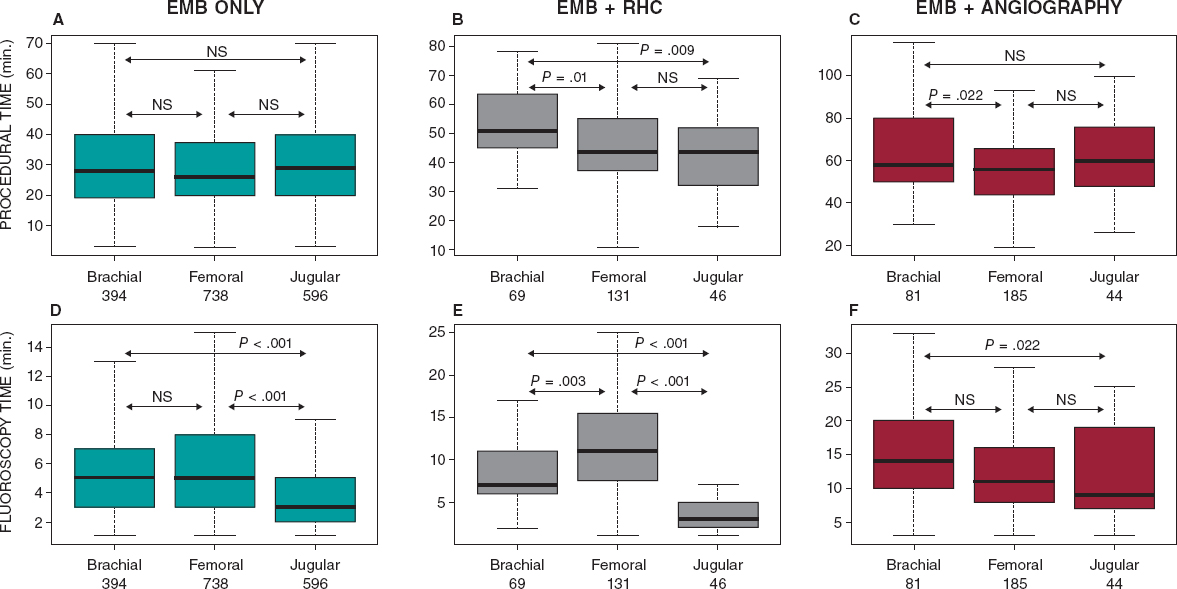
Figure 3. Comparison between the total procedural time (top charts) and fluoroscopy time (bottom charts) according to the different access routes. Inter-group comparisons were conducted using the Kruskal-Wallis and pairwise Wilcoxon tests. RHC, right heart catheterization; NS, not significant.
No major complications occurred at the 48-hour follow-up although 9 minor complications were reported: 2 vein dissections and 3 phebitis all in the brachial procedures, and 4 hematomas, 1 in the brachial access and 3 in the jugular one. Bed rest after femoral access extended for 2 hours. However, it was not required after brachial or jugular access, which facilitated shorter recovery time.
We contacted 19 patients who received repeated procedures (64 total) through 2 or 3 different access routes. They all said that the brachial route was less painful compared to the femoral and jugular ones (2/10 vs 9/10 and 8/10, respectively; P < .001). When asked about their personal preference regarding future procedures, the brachial access was the preferred access route in all the patients. Figure 4 shows the pain and discomfort reported for each access route.
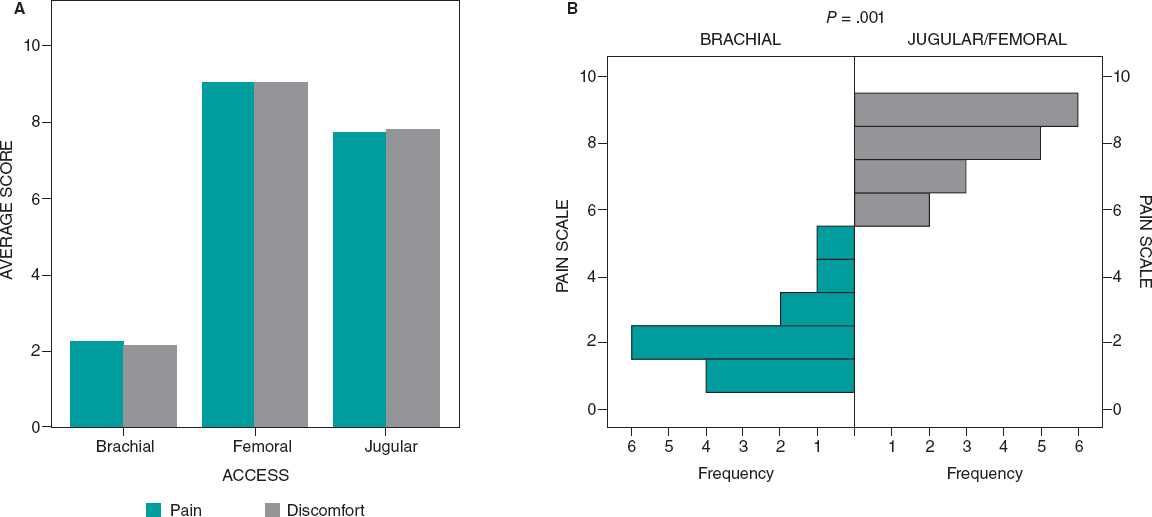
Figure 4. Pain and discomfort perceived during the procedures in patients treated through 2 different access locations (brachial and other). Chart A shows the average numeric pain score for each route from 0 (no pain) to 10 (maximum pain). Chart B shows the distribution of the pain score for the brachial access (green) vs femoral and jugular accesses combined (gray). Differences are statistically significant (Wilcoxon signed-rank test; P = .001).
DISCUSSION
We report the experience of 2 Spanish centers performing EMBs through the brachial veins and the largest series described so far. We showed that it is a feasible and safe alternative that can be used in most patients on a routine basis. Also, we found that in these patients this access route was less painful and uncomfortable compared to the jugular and femoral ones. They also chose it for future prospective procedures.
Experience with the brachial approach
The forearm approach to access the right heart has already been described as a feasible and safe procedure to perform hemodynamic studies in patients with heart failure.9 Since patients with a heart transplant need to receive repeated EMBs as part of rejection monitoring, it is important to use a technique that brings both safety and comfort and avoids central venous punctures to minimize EMB risks.10 For this reason, we decided to describe this new peripheral venous access and compared it to the other 2 approaches often used in our centers.
Brachial vein is a good-sized vessel capable of accommodating 7 Fr sheaths. Its superficial location facilitates easy punctures that can be improved using ultrasound-guidance in cases of suboptimal palpation. Because of its straighter path, the basilic vein was mainly used in both traditional and ultrasound-guided accesses. The cephalic vein, although a plausible access too, connects to the subclavian with a pronounced angle that can stop the advance and rotation of the catheters. The technique described here facilitated the performance of EMBs in all but 33 cases where the guidewire or the catheter could not be advanced. We should mention that ultrasound guidance was not recorded on a routine basis and that half of the failures occurred within the first 3 years of using this approach; we think that both the learning curve and ultrasound guidance are major contributors to access failure.
In the absence of specific materials we decided to adapt the ones available in our catheterization laboratories to meet our purposes. Although we did not observe any complications from cutting the catheter (air embolism, bleeding) having better suited devices would have made the procedures safer and easier.
Peripheral versus central venous access
In this manuscript we reported the differences in procedural and fluoroscopy times among brachial, femoral, and jugular access routes. The brachial route did not seem to increase significantly the total procedural time except for when the biopsy was combined with RHC or angiography. Brachial fluoroscopy time was similar to femoral fluoroscopy time although both were longer compared to the jugular one. These differences remained even when the EMB was combined with the RHC or angiography and are consistent with those previously described in the only other series reported so far.8 The longer total procedural time of brachial procedures may be explained by the longer it took to puncture and wire the peripheral vein; conversely, the femoral vein allows faster punctures, but a more difficult positioning of the catheters–especially the Swan-Ganz–which may explain why fluoroscopy time was longer when using the femoral access in cases that combined EMB plus RHC. Although we did not study operator radiation exposure directly, we think that the radiation the operator may be exposed to is lower in the brachial approach compared to the jugular one. That is so because the former allows keeping further distance away from the X-ray source and use of radioprotective screens, which is something uncomfortable with jugular procedures where the operator is straddling on the C-arm. We should mention that we found a tendency towards shorter total and fluoroscopy times in procedures performed by more experienced operators.
Although previous reports of RHC revealed more complications in the access site in patients treated with transfemoral procedures,11 we could not confirm these findings in patients who received EMB. No major complications occurred in any of the groups either. However, rare minor complications were reported more frequently in the brachial access group. Minor complications in other central locations–such as accidental arterial punctures, small hematomas or nerve damage–maybe were underestimated since data were recorded retrospectively and therefore with reporting bias; considering the location of the jugular and femoral access, we still believe that the risk of complications is real.12,13 Probably, over the next few years ultrasound-guided punctures of central veins will become widely used, which should contribute to increase the safety and comfort of all vascular access routes.
Women had a lower probability of undergoing brachial procedures compared to males. This may be associated with the smaller size of their brachial veins, which may have discouraged the operators from attempting this route.
Regarding the degree of discomfort, patients with brachial access reported significantly lower pain measured through numeric rating scales. Regarding pain and comfort patients with a history of 2 different venous approaches (brachial and another one) preferred the brachial access compared to the femoral or jugular one. Although this cohort was small, these data are consistent with those reported by Harwani et al,8 where the overall preference was brachial approach. This added to the fact that no bed rest is required, makes the brachial access a good choice for subjects in the outpatient setting mainly.
Limitations
This is a retrospective, observational study from 2 tertiary centers and has certain inherent limitations in the comparison of the different routes mainly. One of the main limitations is the retrospective collection of femoral and jugular procedures, which may have underestimated the real prevalence of vascular complications. In our opinion, brachial access may be safer, but this still needs to be confirmed in prospective series of cases. Also, we have to acknowledge that the use of ultrasound-guidance, the reasons for changing the access route or the need for special material (hyrophilic guidewires, contrast injection) were not recorded on a routine basis. Another major limitation is the small number of patients asked to compare their experience with the different accesses; the small size of the cohort led to lower statistical consistency. Finally, the procedures were performed with equipment not specifically designed for these purposes, so it was not the ideal equipment to use. This may indeed have held our technique back. Also, we believe that the development of a low-profile catheter specifically designed for brachial EMBs may contribute to easier and shorter procedures in the future.
CONCLUSION
EMBs obtained from the arm are highly feasible and safe compared to the standard jugular or femoral access. The arm brings extra comfort to the patients and may become the route of choice in experienced centers.
FUNDING
The study did not receive any specific funding. M. Tamargo has been receiving a grant from IISGM (Ayuda Intramural PostMIR del Instituto de Investigación Sanitaria Gregorio Marañón, Madrid, Spain) since 2019. F. Díez-Delhoyo received funds from 2016 to 2019 from Contrato i-PFIS (Doctorados IIS-Empresa en Ciencias y Tecnologías de la Salud, Instituto de Salud Carlos III, Ministry of Economy, Industry and Competitivity, Spain). J. García-Carreño has been receiving funds from Contrato Instituto de Investigación Sanitaria Gregorio Marañón-IISGM, Madrid, Spain since 2019.
L. Grigorian has been receiving funds from Contrato CIBERCV with the project Retos Colaboración — RTC- 2016-4611-1, Madrid, Spain since 2016.
CONFLICTS OF INTEREST
The authors have declared no conflicts of interest whatsoever.
MAIN POINTS
WHAT IS KNOWN ABOUT THE TOPIC?
- EMB is still the gold standard for rejection monitoring purposes and histological confirmation of myocarditis.
- It is usually performed through a central vein, which is associated with the potential risk of major complications.
- Previous evidence shows that right heart catheterization can be performed through a brachial vein. Still, evidence is scarce regarding the possibility of performing EMBs through this vein.
WHAT DOES THIS STUDY ADD?
- EMB performed through a peripheral vein is a feasible and safe option.
- Basilic and cephalic veins can easily be used to obtain endomyocardial samples using the material available in any catheterization laboratory with results comparable to the femoral or jugular vessels.
- The brachial approach seems less painful and should be considered for patients undergoing EMBs.
References
1. Cooper LT, Baughman KL, Feldman AM, et al. The role of endomyocardial biopsy in the management of cardiovascular disease:A Scientific Statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. Eur Heart J. 2007;28:3076-3093.
2. AM, Maleszewski JJ, Rihal CS. Current Status of Endomyocardial Biopsy. Mayo Clin Proc. 2011;86:1095-1102.
3. Kern MJ. Endomyocardial biopsy in cardiac transplant recipients using the femoral venous approach. Am J Cardiol. 1991;67(4):324.
4. Esplugas E, Jara F, SabatéX, et al. Right ventricular endomyocardial biopsy. Description of the percutaneous femoral vein technic. Rev Esp Cardiol. 1987;40:410-414.
5. Schäufele TG, Spittler R, Karagianni A, et al. Transradial left ventricular endomyocardial biopsy:assessment of safety and efficacy. Clin Res Cardiol. 2015;104:773-781.
6. García-Izquierdo Jaén E, Oteo Domínguez JF, Jiménez Blanco M, et al. Diagnostic yield and safety profile of endomyocardial biopsy in the nontransplant setting at a Spanish referral center.REC:interventional cardiology. REC Interv Cardiol. 2019;2:99-107.
7. Practice Guidelines for Central Venous Access:A Report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2012;116:539-573.
8. Harwani N, Chukwu E, Alvarez M, Thohan V. Comparison of Brachial Vein Versus Internal Jugular Vein Approach for Access to the Right Side of the Heart With or Without Myocardial Biopsy. Am J Cardiol. 2015;116:740-743.
9. Bielsa I, España J, Perez Quesada J, Pacheco A. Biopsia cardiaca y cateterismo derecho a través de la vena basílica. Metas Enf. 2006;9:22-26.
10. D'Amario D, Burzotta F, Leone AM, et al. Feasibility and Safety of Right and Left Heart Catheterization Via an Antecubital Fossa Vein and the Radial Artery in Patients With Heart Failure. J Inv Cardiol. 2017;29:301-308.
11. Imamura T, Kinugawa K, Nitta D, et al. Is the Internal Jugular Vein ornFemoral Vein a Better Approach Site for Endomyocardial Biopsy in Heart Transplant Recipients?Int Heart J. 2015;56:67-72.
12. Yang C-H, Guo GB-F, Yip H-K, et al. Bilateral Cardiac Catheterizations. Int Heart J. 2006;47:21-27.
13. Speiser B, Pearson K, Xie H, Shroff AR, Vidovich MI. Compared to femoral venous access, upper extremity right heart catheterization reduces time to ambulation:A single center experience:Arm Access for RHC and Ambulation Times. Catheter Cardiovasc Int. 2017;89:658-664.
14. Bennett MK, Gilotra NA, Harrington C, et al. Evaluation of the Role of Endomyocardial Biopsy in 851 Patients With Unexplained Heart Failure From 2000-2009. Circ:Heart Failure. 2013;6:676-684.
Corresponding author: Departamento de Cardiología, Hospital General Universitario Gregorio Marañón, Dr. Esquerdo 46, 28007 Madrid, Spain.
E-mail address: enrique.gutierrez@salud.madrid.org (E. Gutiérrez Ibañes)
2604-7322 / © 2020 Sociedad Española de Cardiología. Published by Permanyer Publications. This is an open access article under CC BY‑NC‑ND 4.0 license
Congresses abstracts
Special articles
Original articles
Editorials
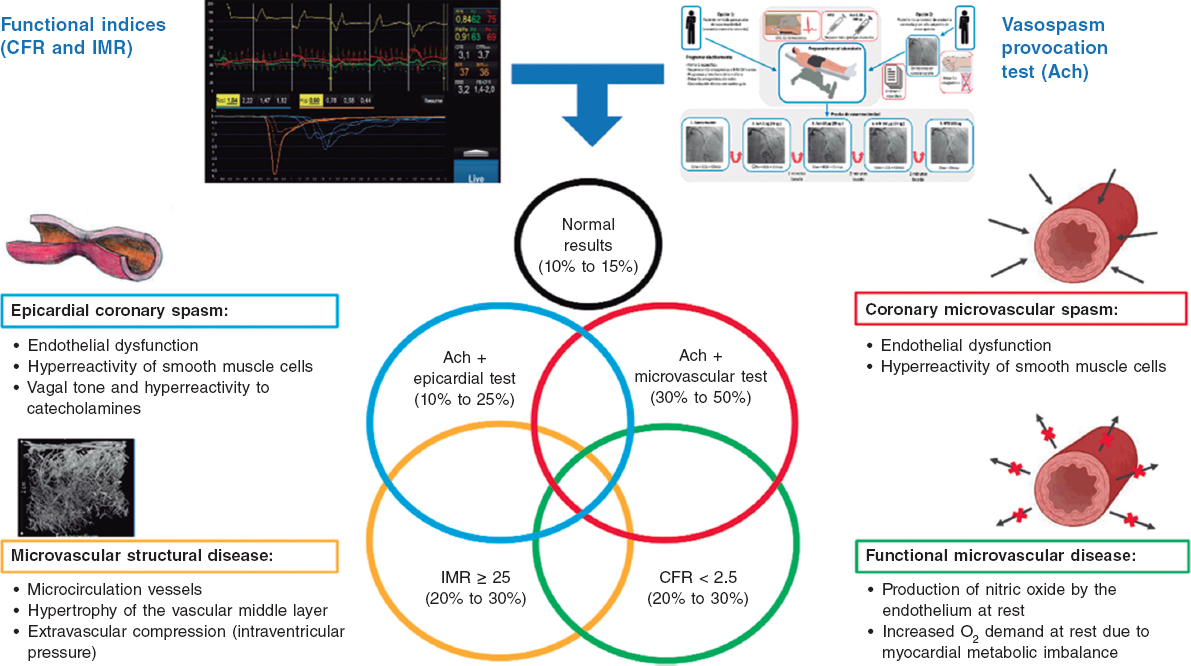
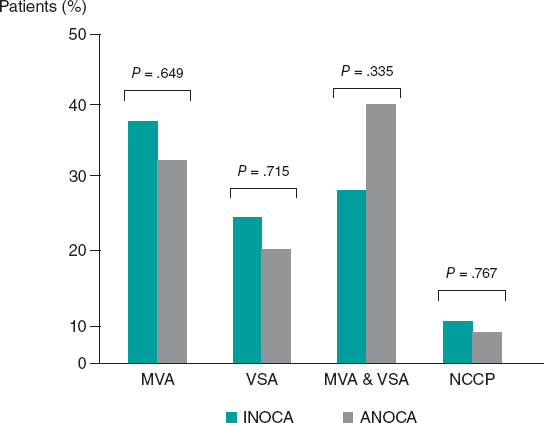
Implementing an ANOCA clinic
aCardiovascular Center Aalst, OLV Clinic, Aalst, Belgium
bDepartment of Cardiology, Lausanne University Hospital, Lausanne, Switzerland
Original articles
Editorials
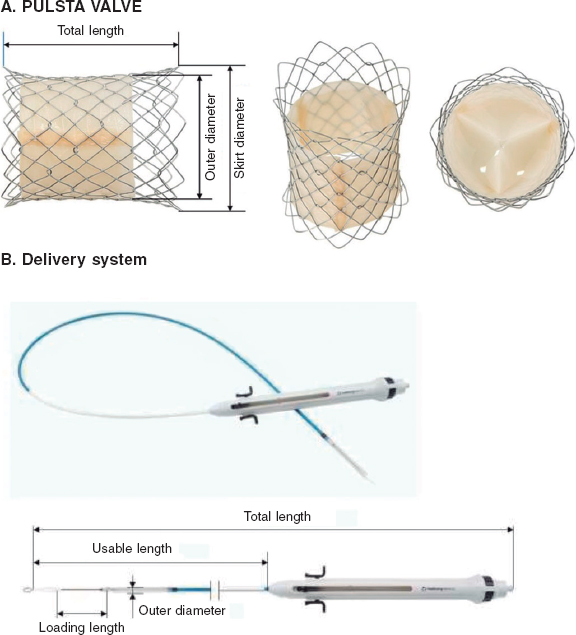
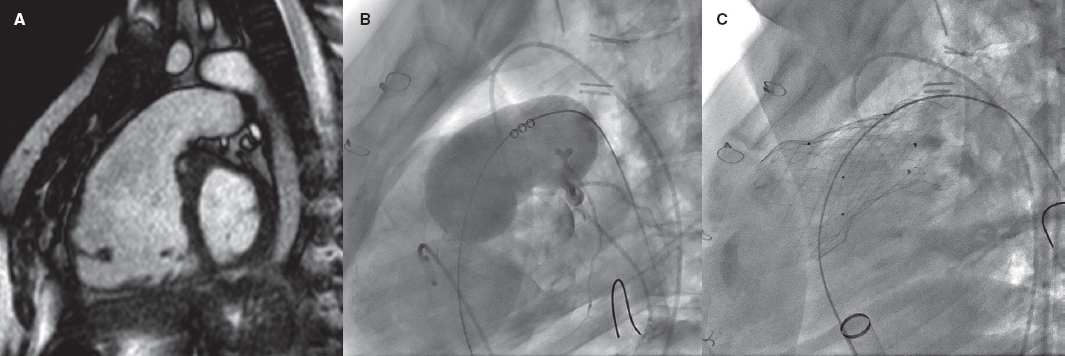
Percutaneous pulmonary valve implantation in native outflow tracts: has the time come?
Servicio de Cardiología, Hospital Universitario La Paz, Madrid, Spain
Debate
Debate: Ablation vs lithotripsy in calcified coronary lesions
The ablation perspective
Unidad de Cardiología Intervencionista, Servicio de Cardiología, Complejo Hospitalario Universitario de Santiago de Compostela, Santiago de Compostela, A Coruña, Spain
Perspective from lithotripsy
Servicio de Cardiología, Hospital Universitario La Paz, Madrid, Spain