ABSTRACT
Introduction and objectives: Regadenoson, a selective agonist of the A2a receptors of adenosine, has been proposed as an alternative for the measurement of fractional flow reserve (FFR). The goal of our study was to assess the utility of regadenoson compared to the use of intracoronary adenosine.
Methods: Forty-one intermediate coronary lesions (30%-70%), in which functional assessment with pressure wire was indicated, were included both prospective and consecutively. Each patient was sequentially administered intracoronary adenosine and intravenous regadenoson and hemodynamic data while the adverse effects were recorded with hyperemia induced by both drugs. The differences seen in the final FFR were analyzed using the linear regression model and the clinically relevant discrepancies were identified assuming 0.80 as the cut-off point.
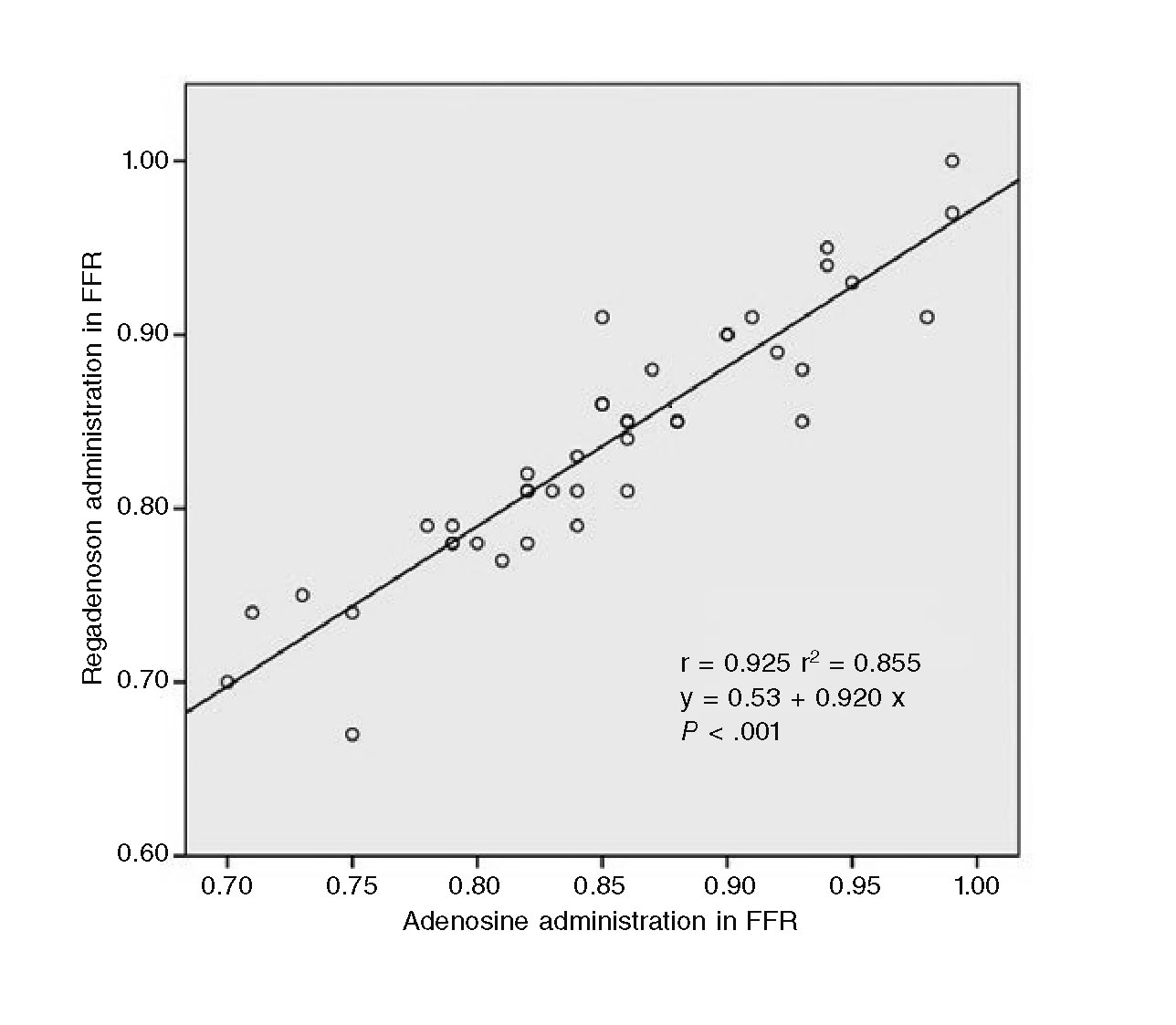
Results: The mean of the FFR was significantly lower with regadenoson compared to adenosine (0.838 ± 0.072 vs 0.852 ± 0.073, P = .002) and in 4 cases (9.8%) clinically relevant differences were found. The regression analysis showed a strong linear correlation between the individual values (r = 0.925, P < .001). Both adenosine and regadenoson significantly reduced mean arterial blood pressure and only regadenoson significantly increased baseline heart rate. In 2 cases (4.9%) asystole was recorded > 3 seconds after the administration of adenosine and no complications were observed with regadenoson.
Conclusions: The administration of regadenoson through an intravenous single bolus has shown a significant reduction in the value of FFR compared to the administration of intracoronary adenosine boluses and the observed differences may be relevant in the clinical decision-making process.
Keywords: Adenosine. Regadenoson. Fractional flow reserve.
RESUMEN
Introducción y objetivos: El regadenosón, un agonista selectivo de los receptores A2a de la adenosina, se ha propuesto como una alternativa para el cálculo de la reserva fraccional de flujo (FFR). El objetivo de este estudio fue evaluar la utilidad del regadenosón en comparación con el uso de adenosina intracoronaria.
Métodos: Se incluyeron de forma prospectiva y consecutiva 41 lesiones coronarias intermedias (30-70%) en las que se indicó valoración funcional con guía de presión. A cada paciente se le administró de forma secuencial adenosina intracoronaria y regadenosón intravenoso, y se registraron los datos hemodinámicos y los efectos adversos con la hiperemia inducida mediante ambos fármacos. Las diferencias en la FFR final se analizaron mediante regresión lineal y se identificaron las discrepancias clínicamente relevantes asumiendo como punto de corte el valor de 0,80.
Resultados: La media de la FFR fue significativamente menor con regadenosón que con adenosina (0,838 ± 0,072 frente a 0,852 ± 0,073; p = 0,002), y en 4 casos (9,8%) se encontraron diferencias clínicamente relevantes. El análisis de regresión mostró una fuerte correlación lineal entre los valores individuales (r = 0,925; p < 0,001). Tanto la adenosina como el regadenosón redujeron de forma significativa la presión arterial media, y solo el regadenosón incrementó significativamente la frecuencia cardiaca basal. En 2 casos (4,9%) se registró asistolia > 3 s tras recibir adenosina y no se observó ninguna complicación con regadenosón.
Conclusiones: La administración de regadenosón en bolo único intravenoso mostró una significativa reducción en el valor de FFR en comparación con la administración de bolos de adenosina intracoronaria, y las diferencias observadas podrían resultar relevantes en la toma de decisiones clínicas.
Palabras clave: Adenosina. Regadenoson. Reserva fraccional de flujo.
Abbreviations: FFR: fractional flow reserve.
INTRODUCTION
The fractional flow reserve (FFR) measurement has become established as a valuable tool for the functional assessment of intermediate coronary stenoses.1 Maximum hyperemia is needed to be able to assess the FFR. The most widely used pharmacological agent to induce vasodilation is adenosine through an intravenous infusion or intracoronary injection.2
Regadenoson, a selective agonist of adenosine A2a receptors has been proposed as an alternative given how easy it is to use since only a single peripheral intravenous bolus at a fixed dose is needed regardless of the patient’s weight and renal function.3-7
Several studies have compared regadenoson to intravenous adenosine,8 but to our knowledge there are no studies comparing regadenoson to intracoronary adenosine for the assessment of the FFR.
The main objective of this study was to establish individual variability in the measurement of FFR using intracoronary adenosine and intravenous regadenoson administered sequentially so each patient is case and control at the same time.
Secondary objectives included analysis of the hemodynamic response, measurement of hyperemia times and assessment of adverse events.
METHODS
Forty-one (41) intermediate coronary lesions were studied both prospective and consecutively in 39 patients referred to undergo a coronary angiography and who had been prescribed functional assessment with pressure guidewire. Stenoses of 30% to 70% estimated visually or through automatic quantification during the angiography procedure were categorized as intermediate lesions. FFR cut-off values ≤ 0.80 were established to indicate revascularization. An informed written consent was obtained from all patients included in this study.
Procedure
Coronary angiography was conducted following routine clinical practice. The FFR was measured using the PressureWire guidewire (St Jude Medical, St Paul, Minnesota, United States) after administering of unfractionated heparin (50 IU/kg) and placing the sensor distal to the lesion, following the standards recommended for acquisition purposes, registry and interpretation of pressure tracings.9
Pharmacological protocol
Based on former dose-response studies, an initial dose of intracoronary adenosine of 100 µg for the right coronary artery and 200 µg for the left coronary artery was established.10
In an attempt to achieve a degree of optimal hyperemia, patients with values close to the cut-off value (FFR < 0.85) were eligible to receive, at the discretion of the operator, repeated doses of 60 µg in each bolus. The minimum value obtained was selected as the true FFR.
After the administration of adenosine, the registry was started, and the phase of hyperemia was considered over when the FFR returned to baseline values. Then, a peripheral intravenous bolus of 400 µg of regadenoson was injected and the measurements re-taken.
The FFR was obtained using an analysis performed on a beat-to-beat basis and when in doubt or in the presence of artifacts, the tracings stored in the console were reviewed.
Additionally, values such as heart rate and arterial blood pressure, both at baseline level and during the phase of hyperemia, were recorded and the possible side effects monitored.
Lastly, data such as the time required by each drug to achieve hyperemia and the duration of hyperemia were recorded for further analysis.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and categorical variables as absolute value or percentage. The Student t test for paired data was used to compare the different FFR values, hemodynamic values (arterial blood pressure and heart rate) and times of hyperemia observed after the administration of adenosine and regadenoson. Symptoms were studied using the chi-square test. Using the linear regression analysis, Pearson’s correlation coefficient and the Bland-Altman plot, the correlation between the different FFR values and both drugs was studied. The statistical analysis was conducted using the SPSS v20 statistical software package (IBM, Armonk, New York, United States) and results were considered significant with P values < .05.
RESULTS
Study patients
Table 1 shows patients baseline characteristics. Overall, 41 intermediate lesions (average stenosis: 52 ± 9%) were studied, 29 of them located in the anterior descending artery, 7 in the right coronary artery, and 5 in the circumflex artery. The average dose of intracoronary adenosine administered was 236 ± 60 µg. No postprocedural complications were observed.
Table 1. Characteristics of the study population
| Sample (n = 41) | |
| Age (years) | 65 ± 14 |
| Women | 27% |
| Body mass index (kg/m2) | 30 ± 3 |
| Prior medical history | |
| Hypertension | 73% |
| Dyslipidemia | 58% |
| Diabetes mellitus | 24% |
| Smoking | 36% |
| Prior infarction | 33% |
| Prior revascularization | 49% |
| Heart failure | 3% |
| Diseased vessels | |
| 1 | 59% |
| 2 | 25% |
| 3 | 16% |
| Artery studied | |
| Anterior descending artery | 67% |
| Circumflex artery | 15% |
| Right coronary artery | 18% |
| Degree of stenosis | |
| 30%-50% | 42% |
| 50%-70% | 58% |
| 70%-90% | 0% |
| Diameter of the vessel (mm) | 3.3 ± 0.5 |
| Dose of intracoronary adenosine (µg) | |
| Left coronary artery | 243 ± 55 |
| Right coronary artery | 206 ± 76 |
Measurement of FFR with intracoronary adenosine vs intravenous regadenoson
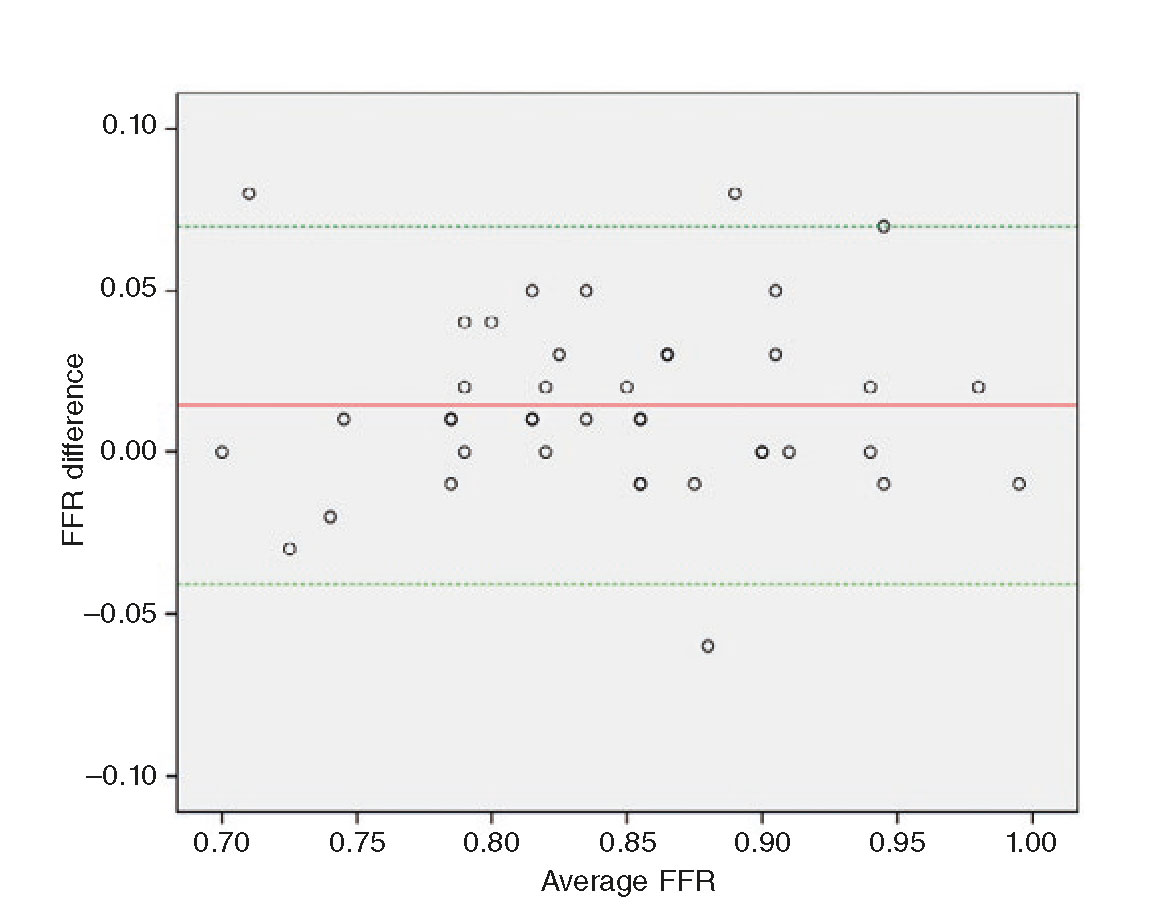
With 1 or both drugs, 13 lesions (33%) showed FFR values ≤ 0.80, indicating a significant functional stenosis. Also, a strong linear correlation with both hyperemic stimuli was seen (r = 0.925; P < .001) (figure 1 and figure 2). However, the FFR measured after the administration of regadenoson was lower compared to the one obtained after the administration of intracoronary adenosine (0.838 ± 0.072 vs 0.852 ± 0.073; P = .002) (table 2). Also, in four different cases (9.8%) there were relevant discrepancies when FFR values > 0.80 with adenosine and ≤ 0.80 with regadenoson were obtained, which led to reclassifying the lesion (table 3).
Table 2. Hemodynamic effects of adenosine and regadenoson
| Fractional flow reserve | Average arterial blood pressure (mmHg) | Heart rate (beats/min) | |
|---|---|---|---|
| Baseline | 0.94 ± 0.05 | 114 ± 22 | 69 ± 12 |
| Adenosine | 0.85 ± 0.07 | 92 ± 21 | 70 ± 14 |
| Regadenoson | 0.84 ± 0.07* | 85 ± 18* | 89 ± 18* |
|
Data are expressed as mean ± standard deviation. *P < .05 with respect to baseline values and adenosine. |
|||
Table 3. Individual values of fractional flow reserve with intracoronary adenosine and intravenous regadenoson
| Case | Age (years) | Sex | Coronary artery | Dose of adenosine (µg) | Adenosine administration in FFR | Regadenoson administration in FFR |
|---|---|---|---|---|---|---|
| 1 | 49 | Male | ADA | 240 | 0.88 | 0.85 |
| 2 | 82 | Male | Cx | 160 | 0.73 | 0.75 |
| 3 | 60 | Male | ADA | 300 | 0.84 | 0.81 |
| 4 | 79 | Male | ADA | 240 | 0.79 | 0.78 |
| 5 | 54 | Male | ADA | 120 | 0.70 | 0.70 |
| 6 | 54 | Male | RCA | 120 | 0.98 | 0.91 |
| 7 | 53 | Male | RCA | 180 | 0.85 | 0.86 |
| 8 | 67 | Male | ADA | 180 | 0.84 | 0.83 |
| 9 | 56 | Male | ADA | 180 | 0.86 | 0.84 |
| 10 | 81 | Male | ADA | 180 | 0.85 | 0.91 |
| 11 | 60 | Female | Cx | 240 | 0.94 | 0.95 |
| 12 | 46 | Male | RCA | 120 | 0.84 | 0.79* |
| 13 | 62 | Male | ADA | 240 | 0.92 | 0.89 |
| 14 | 80 | Female | ADA | 180 | 0.93 | 0.88 |
| 15 | 89 | Female | ADA | 240 | 0.86 | 0.85 |
| 16 | 79 | Male | RCA | 300 | 0.95 | 0.93 |
| 17 | 71 | Female | ADA | 240 | 0.85 | 0.86 |
| 18 | 76 | Female | ADA | 300 | 0.78 | 0.80 |
| 19 | 52 | Male | Cx | 180 | 0.86 | 0.85 |
| 20 | 52 | Male | ADA | 300 | 0.81 | 0.75* |
| 21 | 67 | Male | Cx | 300 | 0.99 | 0.97 |
| 22 | 63 | Male | ADA | 240 | 0.87 | 0.88 |
| 23 | 49 | Female | ADA | 300 | 0.71 | 0.74 |
| 24 | 45 | Female | ADA | 180 | 0.83 | 0.81 |
| 25 | 58 | Male | ADA | 240 | 0.94 | 0.94 |
| 26 | 62 | Male | ADA | 300 | 0.93 | 0.85 |
| 27 | 64 | Male | ADA | 240 | 0.82 | 0.82 |
| 28 | 64 | Male | RCA | 240 | 0.88 | 0.85 |
| 29 | 57 | Female | Cx | 180 | 0.99 | 1.00 |
| 30 | 54 | Male | ADA | 300 | 0.82 | 0.81 |
| 31 | 81 | Male | ADA | 300 | 0.79 | 0.79 |
| 32 | 81 | Male | ADA | 300 | 0.88 | 0.89 |
| 33 | 77 | Female | ADA | 240 | 0.75 | 0.74 |
| 34 | 75 | Male | ADA | 240 | 0.82 | 0.81 |
| 35 | 62 | Female | ADA | 300 | 0.90 | 0.90 |
| 36 | 58 | Male | ADA | 120 | 0.75 | 0.67 |
| 37 | 65 | Male | ADA | 240 | 0.90 | 0.90 |
| 38 | 67 | Male | ADA | 300 | 0.79 | 0.78 |
| 39 | 61 | Female | ADA | 300 | 0.81 | 0.77* |
| 40 | 83 | Female | ADA | 300 | 0.82 | 0.78* |
| 41 | 69 | Male | RCA | 240 | 0.91 | 0.91 |
|
ADA, anterior descending artery; Cx, circumflex artery; FFR, fractional flow reserve; RCA, right coronary artery. *Cases with clinically relevant discrepancies. |
||||||
Figure 1. Linear regression analysis. Correlation of fractional flow reserve values measured with intracoronary adenosine and IV regadenoson in each patient. FFR: fractional flow reserve.
Figure 2. Bland-Altman plot. Graphic representation of the differences seen in the fractional flow reserve measured using intracoronary adenosine and intravenous regadenoson. FFR: fractional flow reserve.
Hemodynamic parameters
With both drugs we observed a significant drop in baseline average arterial blood pressure levels, which was even more pronounced with regadenoson. However, only regadenoson significantly increased baseline heart rate (table 2).
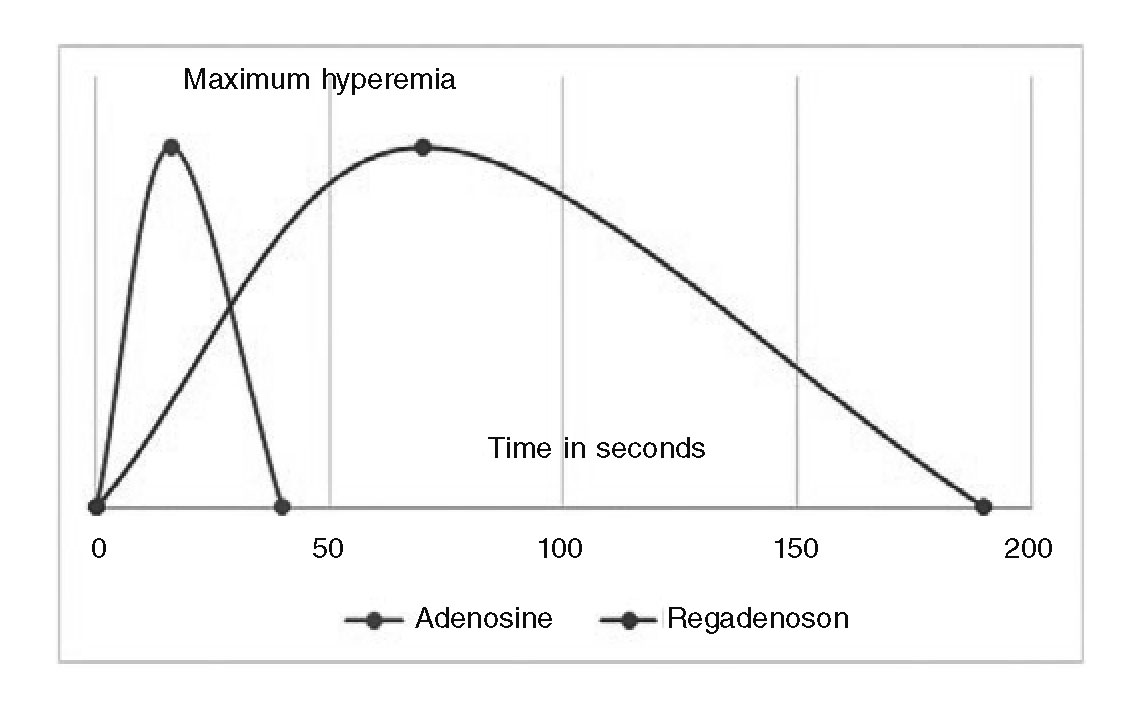
The average time elapsed until reaching maximum hyperemia was significantly lower with adenosine (15 ± 6 vs 61 ± 49 s; P < .001), and this effect was even more prolonged with regadenoson (44 ± 29 vs 174 ± 72 s; P < .001) (figure 3).
Figure 3. Times of hyperemia. Differences seen in the time elapsed until reaching hyperemia and its average duration (in seconds) between intracoronary adenosine and intravenous regadenoson.
Side-effects profile
Side effects were mild with both drugs (table 4). After the administration of regadenoson, most patients experienced some kind of discomfort that they tolerated well and was not an obstacle to continue with the study.
Table 4. Symptoms and adverse events while measuring fractional flow reserve
| Event | Adenosine | Regadenoson | P |
|---|---|---|---|
| Symptoms* | 11 (27) | 30 (73) | .29 |
| Asystole > 3 seconds | 2 (5) | 0 | < .001 |
| Other complications | 0 | 0 | - |
|
Data express n (%). *Dyspnea, chest pain, headache, myocardial blush or nausea. |
|||
Two cases of blockade with pauses longer than 3 seconds after the administration of adenosine were observed in the right coronary artery that resolved spontaneously. No conduction disorders or any other kind of complications were reported with regadenoson.
DISCUSSION
The reliability of FFR measurements depends on the capacity to induce maximum coronary hyperemia.11 The pharmacological agent most widely used is adenosine in intravenous infusions, although intracoronary adenosine is also used by many laboratories because it is faster and achieves similar results. The doses recommended are 100 µg and 200 µg for the right and left coronary arteries, respectively. However, we know that the response to these different doses varies depending on the patient. Some authors recommend doses of 300 µg or even higher, but these high doses have adverse effects, particularly unwanted conduction disorders in diagnostic testing.12
This study shows that the use of regadenoson in a single peripheral intravenous bolus at a fixed dose regardless of the patient’s weight and renal function could be an alternative to adenosine. A good linear correlation has been described between the FFR measured using intracoronary adenosine or intravenous regadenoson (r = 0.925; P < .001).
Also, the comparative analysis conducted showed that the bolus of intravenous regadenoson achieved FFR values that were significantly lower compared to the FFR values obtained using boli of intracoronary adenosine (difference of 0.014 ± 0.028; 95% confidence interval, 0.005-0.023; P = .002).
Maybe the higher hyperemia achieved with regadenoson was the reason why, in four cases with FFR values > 0.80 after the administration of adenosine, FFR values ≤ 0.80 were obtained after the administration of regadenoson, which led to reclassifying the lesion as hemodynamically significant.
On the other hand, the exact administration of intracoronary adenosine dose required the positioning of the guide catheter inside the coronary ostium, which was not always possible, and was the reason why the dose administered was not always the established one.
Thus, due to the administration of an insufficient dose or the use of an inaccurate technique, the fact of the matter is that in 9.8% of the cases maximum hyperemia was not achieved with adenosine. Our data are consistent with former studies that show that up to 10% of the cases may show suboptimal hyperemia with intracoronary adenosine.13-14 In this sense, one recent meta-analysis revealed differences in the FFR similar to those observed in our study when comparing intracoronary adenosine administration and the intravenous infusion of adenosine.15 This may be relevant to indicate revascularization.
Another interesting aspect of regadenoson is that maximum hyperemia was maintained for longer periods of time. Even though our study only analyzed vessels with focal lesions, the longer average time of hyperemia observed with regadenoson (174 ± 72 s) may be useful to perform multiple FFR measurements in vessels with serial lesions or diffuse disease.
One potential limitation of regadenoson is its higher cost compared to adenosine. In this sense, and with no cost-effectiveness studies, a more efficient use of resources has been reported when regadenoson was administered compared to adenosine and dipiridamol in stress tests with isotopes.16
Finally, in our study adverse events were mild with both drugs. However, the negative arrhythmogenic and dromotropic effects of adenosine are well-known. The administration of regadenoson in a single bolus at a fixed dose through peripheral intravenous route showed a good safety profile and complications such as bronchospasm and high-grade atrioventricular block were rare. On rare occasions, the more prolonged vasodilation effect of regadenoson may be unwanted. A 50 mg bolus of intravenous aminophylline may be administered to reverse its effect.17
Limitations
The data presented should be interpreted taking into consideration a series of limitations. This was an observational, open, multicenter study with a small sample, meaning that results may be affected by confounding factors common to this type of studies.
Even though the half-life of intracoronary adenosine is short, we cannot rule out that its prior administration may alter the posterior effect of regadenoson due to preconditioning phenomena.
The maximum dose of adenosine was used at the discretion of the operator, which may have turned out insufficient to induce maximum hyperemia.
Finally, we should not forget that new non-hyperemic indices have stormed into the coronary physiology setting as an alternative to the functional assessment of stenosis without requiring vasodilating agents.
CONCLUSIONS
The administration of regadenoson in a single intravenous bolus has shown greater effectiveness in the measurement of FFR compared to the administration of boli of intracoronary adenosine, and the differences seen may be relevant for the clinical decision-making process. Because of how easy it is to use and because of its safety profile, regadenoson seems like a useful alternative for the hemodynamic assessment of intermediate coronary stenoses.
CONFLICTS OF INTEREST
The authors declared no conflicts of interest whatsoever.
WHAT IS KNOWN ABOUT THE TOPIC?
- Measuring the FFR is a useful tool in the functional assessment of intermediate coronary stenoses.
- In order to measure the FFR we need maximum hyperemia and as the vasodilating agent we need regadenoson, one selective agonist of adenosine A2a receptors that seems like a good option since it requires one single intravenous bolus at a fixed dose regardless of the patient’s weight and renal function.
WHAT DOES THIS STUDY ADD?
- Several studies have drawn comparisons between regadenoson and intravenous adenosine but, to our knowledge, no study has ever compared regadenoson and intracoronary adenosine.
- Our study showed that the bolus of intravenous regadenoson achieves significantly lower FFR values compared to the ones obtained using boli of intracoronary adenosine.
- This greater effectiveness in the measurement of FFR, which is essential to indicate revascularization, its ease of use, and good tolerability turn regadenoson into a good option for FFR functional assessments.
REFERENCES
1. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
2. De Bruyne B, Pijls NH, Barbato E, et al. Intracoronary and intravenous adenosine 5'triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation. 2003;107:1877-1883.
3. Nair PK, Marroquin OC, Mulukutla SR, et al. Clinical utility of regadenoson for assessing fractional flow reserve. J Am Coll Cardiol Intv. 2011;4:1085-1092.
4. Arumugham P, Figueredo VM, Patel PB, et al. Comparison of intravenous adenosine and intravenous regadenoson for the measurement of pressure-derived coronary fractional flow reserve. EuroIntervention. 2013;8:1166-1171.
5. Prasad A, Zareh M, Doherty R, et al. Use of regadenoson for measurement of fractional flow reserve. Catheter Cardiovasc Interv. 2014;83:369-374.
6. VanNunen LX, Lenders GD, Schampaert S, et al. Single bolus intravenous regadenoson injection versus central venous infusion of adenosine for maximum coronary hyperaemia in fractional flow reserve measurement. EuroIntervention. 2015;11:905-913.
7. Stolker JM, Lim MJ, Shavelle DM, et al. Pooled comparison of regadenoson versus adenosine for measuring fractional flow reserve and coronary flow in the catheterization laboratory. Cardiovasc Revasc Med. 2015;16:266-271.
8. Lee JZ, Singh N, Nyotowidjojo I, et al. Comparison of regadenoson and nitroprusside to adenosine for measurement of fractional flow reserve:A systematic review and meta-analysis. Cardiovasc Revasc Med. 2018;2:168-174.
9. Toth GG, Johnson NP, Jeremias A, et al. Standardization of fractional flow reserve measurements. J Am Coll Cardiol. 2016;7:742-753.
10. Adjedj J, Toth GG, Johnson NP, et al. Intracoronary adenosine:dose-response relationship with hyperemia. J Am Coll Cardiol Intv. 2015;8:1422-1430.
11. Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary artery stenoses. N Engl J Med. 1996;334:1703-1708.
12. Lopez-Palop R, Carrillo P, Frutos A, et al. Comparison of effectiveness of high-dose intracoronary adenosine versus intravenous administration on the assessment of fractional flow reserve in patients with coronary heart disease. Am J Cardiol. 2013;111:1277-1283.
13. Jeremias A, Whitbourn RJ, Filardo SD, et al. Adequacy of intracoronary versus intravenous adenosine-induced maximum coronary hyperemia for fractional flow reserve measurements. Am Heart J. 2000;140:651-657.
14. Casella G, Leibig M, Schiele TM, et al. Are high doses of intracoronary adenosine an alternative to standard intravenous adenosine for the assessment of fractional flow reserve?Am Heart J. 2004;148:590-595.
15. Rigattieri S, BiondiZoccai G, Sciahbasi A, et al. Meta-Analysis of Head-to-Head Comparison of Intracoronary Versus Intravenous Adenosine for the Assessment of Fractional Flow Reserve. Am J Cardiol. 2017;120:563-568.
16. Friedman M, Spalding J, Kothari S, et al. Myocardial perfusion imaging laboratory efficiency with the use of regadenoson compared to adenosine and dipyridamole. J Med Econ. 2013;16:449-460.
17. Al Jaroudi W, Iskandrian AE. Regadenoson:A New Myocardial Stress Agent. J Am Coll Cardiol. 2009;54:1123-1130.
E-mail address: pau@comv.es (P. Federico Zaragoza).