To the Editor,
The use of extracorporeal membrane oxygenation (ECMO) circulatory support devices in patients with cardiac arrest, shock, or refractory respiratory failure due to pulmonary thromboembolism is increasingly recognized as a safe and effective therapy.1-3 With the aim of improving the hemodynamic and respiratory status of these patients, the adjuvant use of transcatheter pulmonary thrombectomy through thrombus aspiration is increasingly common.4-6 However, combining these two therapies requires careful consideration of technical issues to ensure procedural success and prevent additional risks.
ECMO consists of a centrifugal pump that rotates at high speed to create negative pressure in the central axis, allowing blood to be aspirated through the venous insertion cannula (figure 1 of the supplementary data). Subsequently, after passing through the ECMO, the blood is pumped through a second cannula—arterial or venous—to be reintroduced into the patient’s circulatory system.
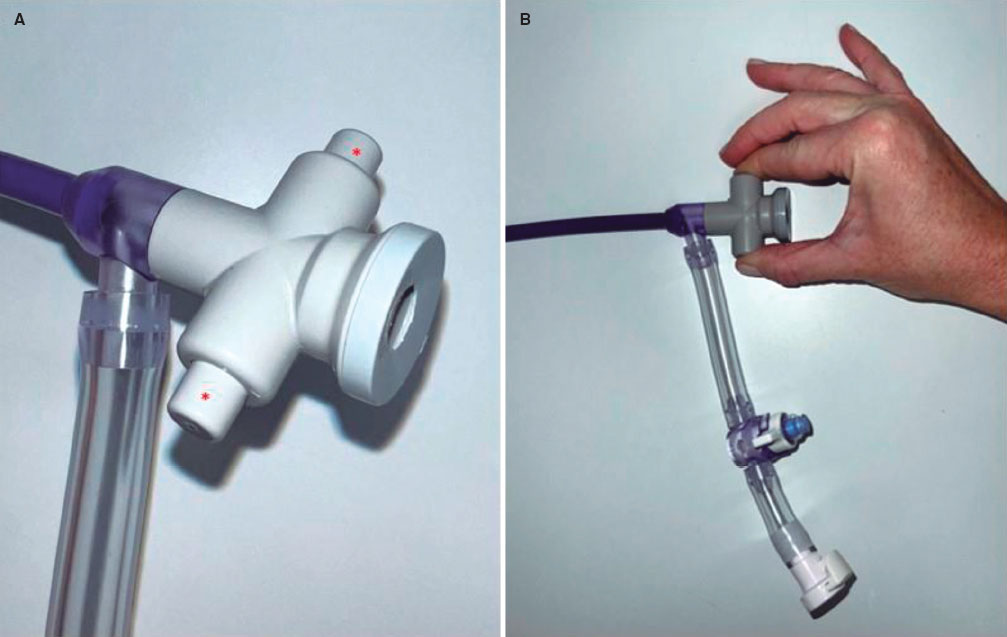
Figure 1. A: valve of a large-bore thrombus aspiration catheter. The asterisk shows the 2 buttons that, when pressed, allow the valve to open. B: opening of the valve by pressing the 2 buttons. Support needs to be reduced or stopped before opening this or any other valve in patients on extracorporeal membrane oxygenation (ECMO).
Sealing refers to the quality of a system or compartment being isolated from the rest, without transfers. Under normal conditions, the vascular system is considered sealed, with no blood losses or entries of other elements. However, its integrity is compromised if a vessel is punctured, creating a shunt with the exterior. When the puncture orifice is closed, the vascular system regains its seal either by closing the catheter or by connecting the catheter or a cannula to another closed system (such as the ECMO circuit). Thus, after cannulating the accesses and connecting them to the ECMO circuit, both the patient’s vascular system and the ECMO system form a common sealed circuit, which is compromised only if openings occur at any point in the system.
Transcatheter thrombus aspiration devices consist of 1 or several usually large-bore catheters, which are inserted through a vein and guided toward the thrombotic material, usually in the main or segmental pulmonary arteries (figure 2 of the supplementary data).
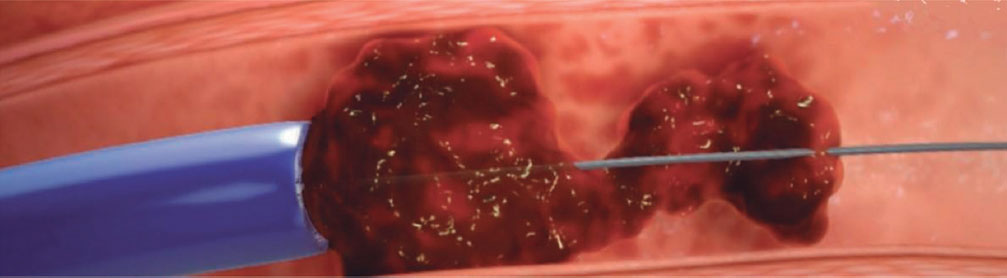
Figure 2. Graphic representation of the obstruction of a thrombus aspiration catheter by a large thrombus, which becomes lodged at the tip of the catheter. Extracorporeal membrane oxygenation (ECMO) flow reduction and rapid catheter withdrawal while on negative pressure reduce the risk of embolization to the ECMO venous cannula.
Once the catheter is in position, the thrombus is removed using various techniques, such as manual or automatic aspiration, etc. During the procedure, different valves of the system usually need to be opened or even removed for device reinsertion, which may interfere with ECMO in a patient requiring combined therapy.
When thrombus aspiration is performed in a patient connected to a pump system that creates negative pressure in the venous line, various special situations should be considered to prevent complications or dysfunctions resulting from the interaction of these devices. Although veno-arterial ECMO is the most widely used system in this context, other systems that create negative pressure, such as veno-venous ECMO, may lead to similar complications, which can be prevented in the same way, as they all stem from the aspiration generated by the venous cannula. The most frequent complications are outlined below.
The most common and potentially serious complication is air embolism. When any of the valves or taps of the thrombus aspiration catheters are opened, the patient-ECMO system loses its seal. If this occurs while ECMO is running, the negative pressure created by the pump in the venous system (ideally up to −60 mmHg) generates a pressure difference with the ambient air (1 atm = 760 mmHg), leading to air movement or aspiration from the outside into the venous system, causing venous air embolism. To prevent this complication, we need to clamp the ECMO arterial cannula or reduce the revolutions when performing any of these operations: a) introducing or extracting the dilators or introducer sheaths/catheters; b) opening the valves that make up the catheters or the introducer sheaths (figure 1); c) entering or removing the devices through the introducer sheath.
Since the patient is supported by the device, meticulous coordination between the interventional cardiologist and the ECMO operator is required to minimize support reduction or clamping times (less than 2-4 seconds in experienced groups).
Another potential complication is obstruction of the ECMO venous cannula due to embolization of thrombotic material, which can cause the system to stop. The obstruction of the venous cannula is a consequence of thrombus embolization from the thrombus aspiration catheter (figure 2). This usually occurs when the thrombus aspiration catheter is obstructed by a large thrombus and requires manual extraction outside the patient’s vein. As the catheter advances toward the exterior, it approaches the distal end of the venous cannula, which is when the risk of embolization is highest. Precautions during thrombus removal include the following: a) maintaining negative pressure in the thrombus aspiration catheter; b) decreasing the ECMO flow to reduce the suction power of the venous cannula; c) quickly and continuously removing the thrombus aspiration catheter.
Finally, another complication is venous suction. The continuous blood suction generated by the system in the venous line reduces both the volume and velocity of blood flow reaching the pulmonary arteries, thus decreasing the suction pressure that the catheter can create, along with its effectiveness. Although not imperative, in cases of failed aspirations, we recommend reducing ECMO flow during aspiration to increase efficacy, reduce the duration of the procedure, and minimize blood loss.
In conclusion, pulmonary thrombectomy through thrombus aspiration in patients with high-risk pulmonary embolism who require ECMO support is feasible and can improve the patient’s clinical status. Considering some technical aspects can facilitate the procedure and prevent the risk of complications. Adequate team communication and coordination are essential to ensure the success of the procedure.
FUNDING
The authors declare that they have no affiliations or involvement with any organization or entity with financial interest (such as fees, educational grants, participation in conferences, memberships, employment, consulting, stock ownership, or other financial interests, and agreements for expert testimony or patent licenses), nor any nonfinancial interests (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the topic or materials presented in this article.
ETHICAL CONSIDERATIONS
Informed consent or validation by an ethics committee was not deemed necessary since no patients were included in this study. Possible biases of sex and gender were taken into consideration while drafting this article.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence tools have been used in the preparation of this work.
AUTHORS’ CONTRIBUTIONS
All authors significantly contributed to the drafting of this work.
CONFLICTS OF INTEREST
R. Moreno is an associate editor of REC: Interventional Cardiology; the journal’s editorial procedures to ensure the impartial processing of the manuscript have been followed. The remaining authors declared no conflicts of interest related to this work.
REFERENCES
1. Giraud R, Laurencet M, Assouline B, De Charrière A, Banfi C, Bendjelid K. Can VA-ECMO Be Used as an Adequate Treatment in Massive Pulmonary Embolism?J Clin Med. 2021;10:3376.
2. Scott JH, Gordon M, Vender R, et al. Venoarterial Extracorporeal Membrane Oxygenation in Massive Pulmonary Embolism-Related Cardiac Arrest:A Systematic Review. Crit Care Med. 2021;49:760-769.
3. Pasrija C, Kronfli A, George P, et al. Utilization of Veno-Arterial Extracorporeal Membrane Oxygenation for Massive Pulmonary Embolism. Ann Thorac Surg. 2018;105:498-504.
4. Kucher N, Ouda A, Voci D, et al. Percutaneous large-bore aspiration embolectomy with veno-arterial extracorporal membrane oxygenation support or standby in patients with high-risk pulmonary embolism and contraindications to thrombolysis:a preliminary single centre experience. Eur Heart J Acute Cardiovasc Care. 2023;12:232-236.
5. Munakata R, Yamamoto T, Hosokawa Y, et al. Massive pulmonary embolism requiring extracorporeal life support treated with catheter-based interventions. Int Heart J. 2012;53:370-374.
6. Toma C, Khandhar S, Zalewski AM, D'Auria SJ, Tu TM, Jaber WA. Percutaneous thrombectomy in patients with massive and very high-risk submassive acute pulmonary embolism. Catheter Cardiovasc Interv. 2020;96:1465-1470.