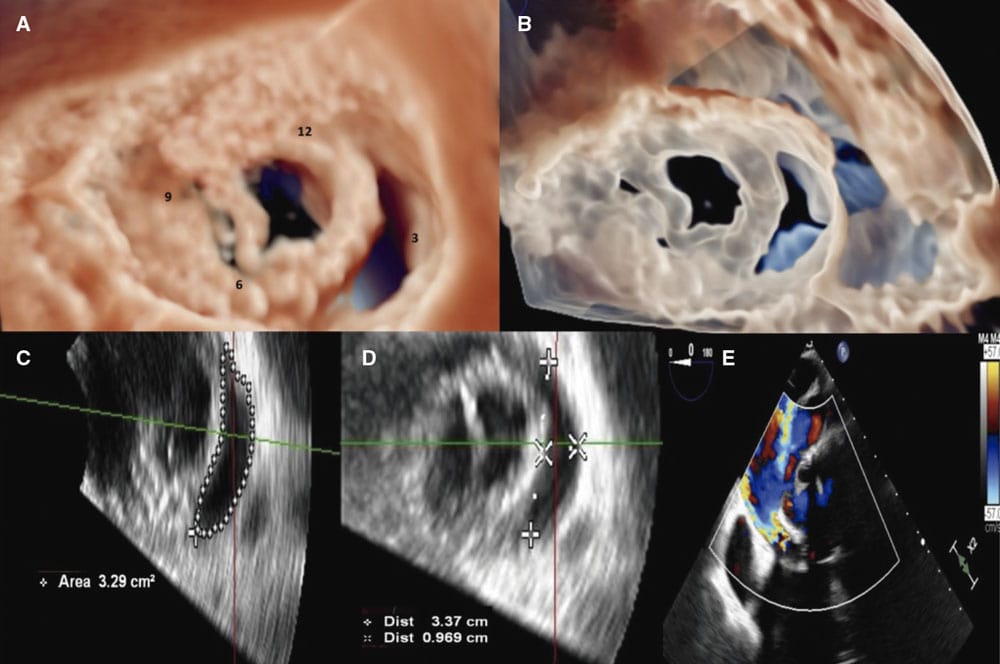
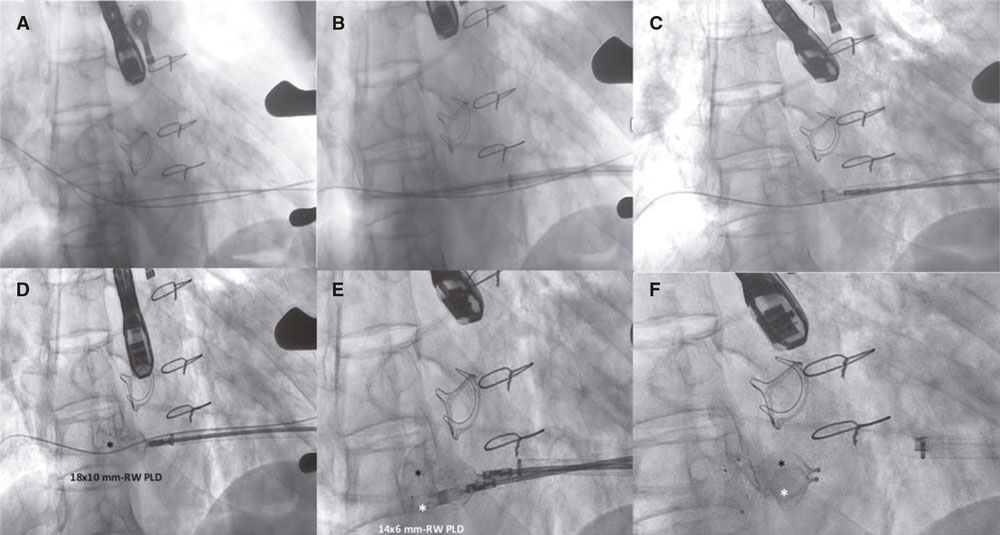
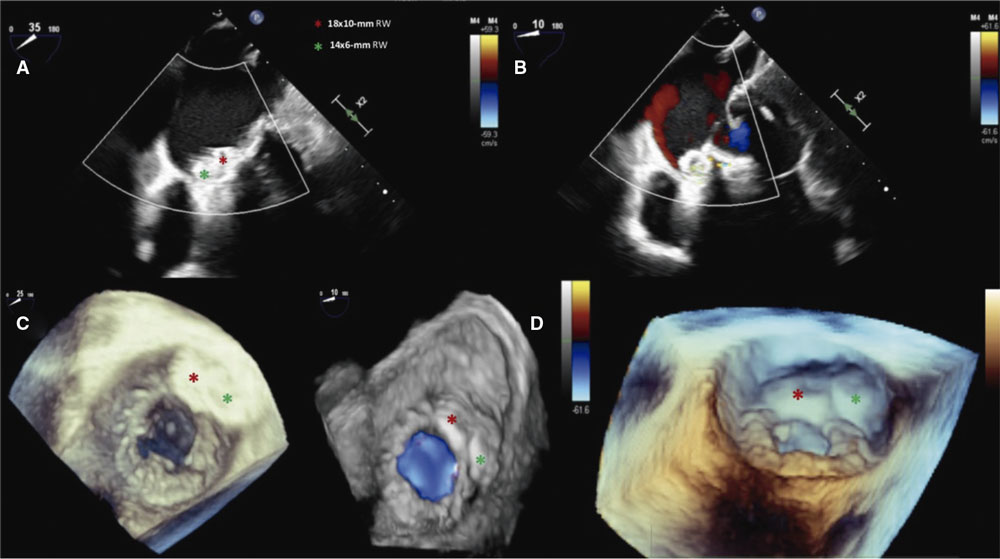
This is the case of a 75-year-old man with heart failure (HF) due to severe aortic regurgitation caused by infective endocarditis treated with aortic and mitral bioprosthetic valve replacement. At 6 months, HF relapsed due to severe mitral paravalvular leak (PVL) regurgitation caused by a giant 33 mm x 9 mm crescent-shaped leak of medial-posterior location (2 to 5 o’clock position), with an area of 3.29 cm2 (figure 1A-E, video 1 of the supplementary data). The patient was deemed at prohibitive surgical risk, and gave his informed consent to undergo catheter based PVL closure. The procedure was performed in a hybrid operating room under general anesthesia, continuous real-time 2D/3D transesophageal echocardiography (TEE) color Doppler imaging and fluoroscopic guidance. An open surgical retrograde double transapical access (hybrid technique) was preferred due to the considerably huge size of the leak and the possible need for multiple simultaneous large devices. Through the 2 short sheaths placed at the left ventricle apex we easily passed the leak in sequence with 2 0.035-in hydrophilic guidewires that were later exchanged for 2 extra-stiff guidewires placed in the pulmonary veins (figure 2A-B). Afterwards, we implanted a 18 mm x 10 mm rectangular waist (RW) paravalvular leak device (PLD, Occlutech, Sweden) followed by a 14 mm x 6 mm RW PLD, simultaneously (figure 2C-F, video 2 of the supplementary data). The final 2D/3D TEE confirmed the effective closure of this gigantic mitral PVL (figure 3A-D). The postoperative course was uneventful, and the patient was discharged with an improved clinical condition. At 2-month follow-up, 2D/3D TEE color Doppler imaging confirmed the stable position of the device with trivial residual leak. In the case of this giant mitral PVL, the choice of specifically designed device technology and the double transapical access were the key to success.
Figure 1.
Figure 2.
Figure 3.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
E.M. Onorato drafted the initial manuscript. All authors critically reviewed the manuscript and approved its final version.
CONFLICTS OF INTEREST
E.M. Onorato is a consultant for Occlutech. The remaining authors declared no conflicts of interest whatsoever.
SUPPLEMENTARY DATA
Vídeo 1. Onorato EM. DOI: 10.24875/RECICE.M22000307
Vídeo 2. Onorato EM. DOI: 10.24875/RECICE.M22000307