Thirty-six-year-old male referred to the emergency room by the general practitioner with chest pain of 1-month duration. After the initial assessment revealed the presence of diffuse T-wave flattening, normal troponin levels, and a normal echocardiogram, the patient was discharged with a diagnosis of low-risk atypical chest pain. However, due to symptom recurrence and the fact that the treadmill test triggered angina-like symptoms and the ECG showed transient T-wave abnormalities, a coronary angiography was performed that ruled out the presence of epicardial stenosis (video 1 of the supplementary data).
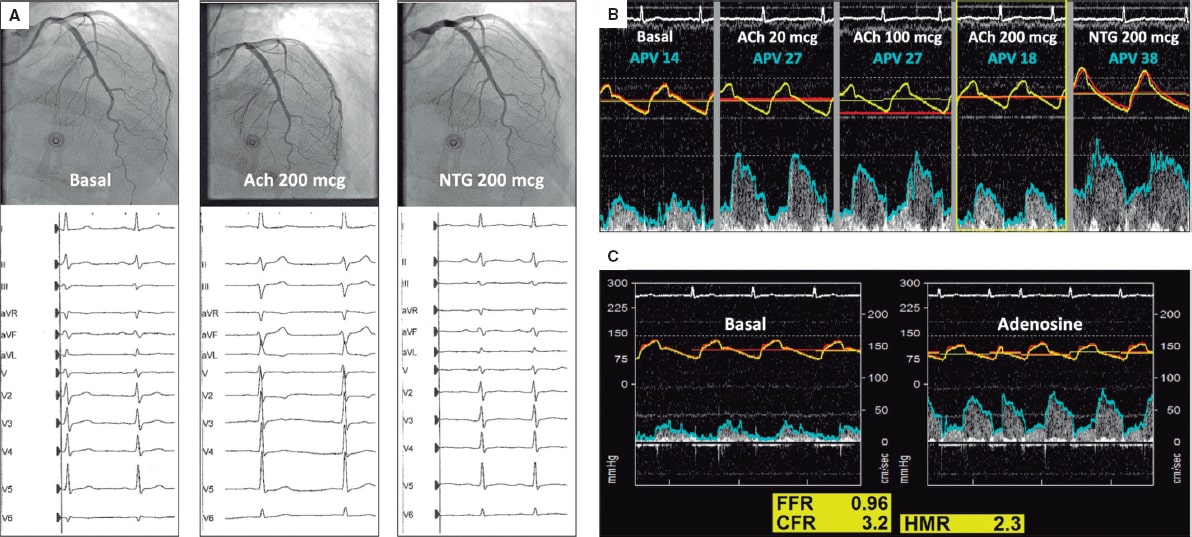
The patient was readmitted a week later due to disabling oppressive chest pain related to low intensity exercise. Due to persistent angina without coronary stenosis, an intracoronary physiological assessment was scheduled with acetylcholine, adenosine, and simultaneous pressure and flow measurements in the left anterior descending coronary artery using a dual-sensor pressure and Doppler velocity guidewire. Acetylcholine (Ach) (200 mcg) triggered the patient’s typical symptoms, the repolarization abnormalities seen on the ECG and the 50% decrease of coronary artery flow velocity (APV) without epicardial spasm (video 2 of the supplementary data). Intracoronary nitroglycerin (NTG) solved all abnormalities (figure 1A,B). The adenosine non-endothelium-dependent assessment revealed a normal fractional flow reserve (FFR), hyperemic microcirculatory resistance (HMR), and coronary flow reserve (CFR) (figure 1C). Because of the clinical features present (acetylcholine-triggered angina with repolarization abnormalities seen on the ECG without epicardial spasm), microvascular vasospastic angina was diagnosed. Medical therapy adjustment with calcium channel blockers as first-line treatment improved the patient’s symptoms at the follow-up.
Figure 1.
This case illustrates the value of comprehensive intracoronary physiological assessment to evaluate specific pathways of vascular dysfunction in patients with persistent angina. This approach is supported by the 2019 ESC clinical practice guidelines on the management of chronic coronary syndromes in patients without obstructive coronary stenoses. The patient’s consent was obtained to report his case anonymously.
FUNDING
The manuscript has not been funded.
AUTHORS' CONTRIBUTIONS
The text has been prepared and revised with the participation of all signatory authors.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Provencio A. DOI: 10.24875/RECICE.M20000180
Vídeo 2. Provencio A. DOI: 10.24875/RECICE.M20000180