ABSTRACT
Introduction and objectives: ST-segment elevation myocardial infarction (STEMI) regional networks pose great organizational differences that may compromise their results. The Working Group on Hemodynamics and Interventional Cardiology has carried out a survey among its members on the level of satisfaction and the state of primary angioplasty programs in Spain.
Methods: On-line, open and anonymous survey, among the Hemodynamics and Interventional Cardiology Working Group members conducted between May 22 and June 5, 2018 on the necessities of the aforementioned programs and the degree of satisfaction of the professionals involved.
Results: Answers were obtained from 172 professionals with representation from 75 centers and 17 autonomous communities. The number of angioplasties performed in the STEMI setting per year and per center was 259 ± 110. The degree of satisfaction of the professionals with the application of the Infarction Code and the degree of personal satisfaction scored 7.2 ± 2.2 and 7.2 ± 2.4 points out of 10, respectively, although with significant regional differences. The main areas of concern detected were logistics issues, insufficient paycheck compensations and lack of rest. The 55% were inclined to leave their on-call duties when possible.
Conclusions: The survey has revealed a high degree of satisfaction by the professionals involved in STEMI treatment, although with notable differences among different autonomous communities and has allowed detecting logistical, structural and paycheck disturbances that can put primary angioplasty programs in situations of vulnerability.
Keywords: Infarction Code. ST-segment elevated myocardial infarction. Survey. Satisfaction. Primary PCI.
RESUMEN
Introducción y objetivos: Las redes regionales de atención al infarto agudo de miocardio con elevación del segmento ST presentan grandes diferencias en términos de organización que puede llegar a comprometer sus resultados. La Sección de Hemodinámica y Cardiología Intervencionista ha realizado una encuesta entre sus miembros sobre el grado de satisfacción y la situación de los programas de angioplastia primaria en España.
Métodos: Se realizó una encuesta online, abierta y anónima, entre los miembros de la Sección de Hemodinámica y Cardiología Intervencionista entre los días 22 de mayo y 5 de junio de 2018, sobre las necesidades de los programas y el grado de satisfacción de los profesionales.
Resultados: Se obtuvieron 172 respuestas de profesionales, con representación de 75 centros y 17 comunidades autónomas. El número de angioplastias en el infarto agudo de miocardio con elevación del segmento ST por año y por centro fue de 259 ± 110. El grado de satisfacción de los profesionales con la aplicación del Código Infarto, así como el grado de satisfacción personal, obtuvieron una puntuación de 7,2 ± 2,2 y 7,2 ± 2,4 puntos sobre 10, respectivamente, aunque con diferencias regionales significativas. Las principales áreas de preocupación detectadas fueron las limitaciones logísticas, la retribución insuficiente y la falta de descanso. Si fuera posible, un 55% estaría dispuesto a dejar las guardias.
Conclusiones: La encuesta ha puesto de manifiesto un alto grado de valoración del sistema por parte de los profesionales, aunque con diferencias notables entre las comunidades autónomas, y ha permitido detectar disfunciones logísticas, estructurales y retributivas que pueden poner a los programas de angioplastia primaria en situación de vulnerabilidad.
Palabras clave: Código Infarto. Infarto con elevación del segmento ST. Encuesta. Satisfacción. Angioplastia primaria.
Abbreviations: PPCI: primary percutaneous coronary intervention. SHCI: Working Group on Hemodynamics and Interventional Cardiology. STEMI: ST-segment elevation myocardial infarction.
INTRODUCTION
The ST-segment elevation acute myocardial infarction (STEMI) is one of the leading causes of cardiovascular morbimortality. Primary percutaneous coronary intervention (pPCI) or primary angioplasty is the recommended reperfusion therapy for the management of STEMI since it reduces mortality and major ischemic events compared to pharmacological reperfusion therapy. This benefit is only evident when the pPCI is performed in adequate centers (infarction centers) by experienced professionals and ideally within the first 2 hours after the patient first medial contact contact with the healthcare system1. These conditions require a huge organizational effort in order to guarantee early diagnoses, quick transfers of patients to the infarction centers, and the availability of a team capable of performing the procedure swiftly and 24/7.2-4.
Over the last few years Spain has seen the gradual arrival of regional networks for the management of STEMI that, in most cases, have spread nationwide. The heterogeneity implicit in the structures of the different healthcare systems has produced great organizational differences in these networks from programs created exclusively by healthcare providers with almost no institutional support to programs where the Administration has been involved providing detailed analyses of subdivisions, logistics, infrastructure, and all necessary resources5,6. The particular characteristics and specific requirements of pPCI programs can put them in a scenario of vulnerability which can gradually make very difficult to keep their sustainability while limiting the favorable prognostic impact they have on patients with STEMI.
In order to study the current situation of pPCIs in Spain, detect vulnerabilities in the system, and establish minimum requirements from the point of view of organization, infrastructure, and outcome assessment, the Working Group on Hemodynamics and Interventional Cardiology (SHCI) of the SEC promoted the creation of the SHCI Infarction Code Working Group. This paper shows tHe results of a survey on the actual situation of primary angioplasty programs in Spain, and the degree of satisfaction of the interventional cardiologists involved.
Methods
Study population
A survey was conducted online through a website and a mobile app. The survey was open and anonymous and was carried out among SHCI members. The respondents received an invitation through a link sent directly to their e-mail accounts and through direct access from the SHCI official website.
Data mining
The survey was conducted from May 22 through June 5, 2018. It included 4 different sections: personal data from respondents (while keeping their anonymity), information from the corresponding center, characteristics of the pPCI program, and opinions on this program. This last section included a blank box to write areas for improvement, grouped into 3 sections for analysis: issues related to improving logistics, changes in the rate pay model and changes in the resting hours model. Table 1 shows the survey questions. Answering these questions took no more than 5 minutes.
Table 1. Questions asked in the survey
| Personal data |
| Center (optional) |
| Atuonomous community |
| Age (N) |
| Sex (male/female) |
| Years performing pPCI (N) |
| Data from the center |
| Type of hospital management (public/private) |
| Human resources of the center (professionals participating in the pPCI program): Number of interventional cardiologists (N) Number of nurses (N) Number of assistant nurses (N) |
| Annual number of pPCI performed per STEMI at the center (N) |
| Specifics of the center pPCI program |
| Possibility of rest after the pPCI while on-call duty (Yes/No) |
| Type of rest after the pPCI while on-call duty (next day/some other day) |
| Hours of rest after being activated while on-call duty (N) |
| Distribution of the calls (in weeks/days) |
| Number of professionals within the on-call duty program: Number of interventional cardiologists (N) Number of nurses (N) Number of assistant nurses (N) Number of technicians (N) |
| Type of payment per on-call duty: Payment of on-call duty only (Yes/No) Payment of on-call duty plus payment of physical presence during activation hours (Yes/No) Payment of on-call duty with physical presence in case of activation only (Yes/No) Payment per procedure (Yes/No) On-call daily double list (Yes/No) On-call double list during the weekend (Yes/No) Payment per monthly on-call duty (Yes/No) |
| Opinion on the center pPCI program |
| ¿Would you say that the implementation of the Infarction Code initiative carried out by your center was satisfactory? Score from 1 to 10 |
| ¿Do you think that the management of STEMI patients can be improved at your center? (Yes/No) |
| In your professional opinion, not in the patient’s opinion, and regarding the management of ST-segment elevation acute coronary syndrome, are you satisfied with your job? Score from 1 to 10 |
| ¿Would you say that the pay received per activation is fair? (Yes/No) (Sí/No) |
| ¿In your opinion, can you have sufficient rest after being activated? (Yes/No) |
| ¿Would you say that there is enough personnel to handle all on-call duties (Yes/No) (Sí/No) |
| ¿In your opinion, how many doctors should your cath lab have to be able to handle all hemodynamic on-call duties? (N) |
| ¿In your opinion, the implementation of the Infarction Code initiative has improved the management of patients with ST-segment elevation acute coronary syndrome? (Yes/No) |
| ¿Would you say that the responsibility that your job requires receives the recognition it deserves? (Yes/No) |
| Would you consider leaving the on-call mandatory program once you are not eligible anymore? (Yes/No) |
| Write all possible areas with room for improvement. What kind of rest would you need? What about the pay? And what about your numbers? (free writing) |
|
N, number; pPCI, primary percutaneous coronary intervention; STEMI, ST-segment elevation acute myocardial infarction. |
Analysis
The descriptive variables are expressed as means ± standard deviations, the continuous variables as ranges, and interquartile ranges (between square brackets), and the discrete variables are expressed as a numbers (percentage of frequency).
All analyses were conducted using the STATA 15.1 statistical software package (StataCorp, College Station, Texas, United States).
RESULTS
Study population
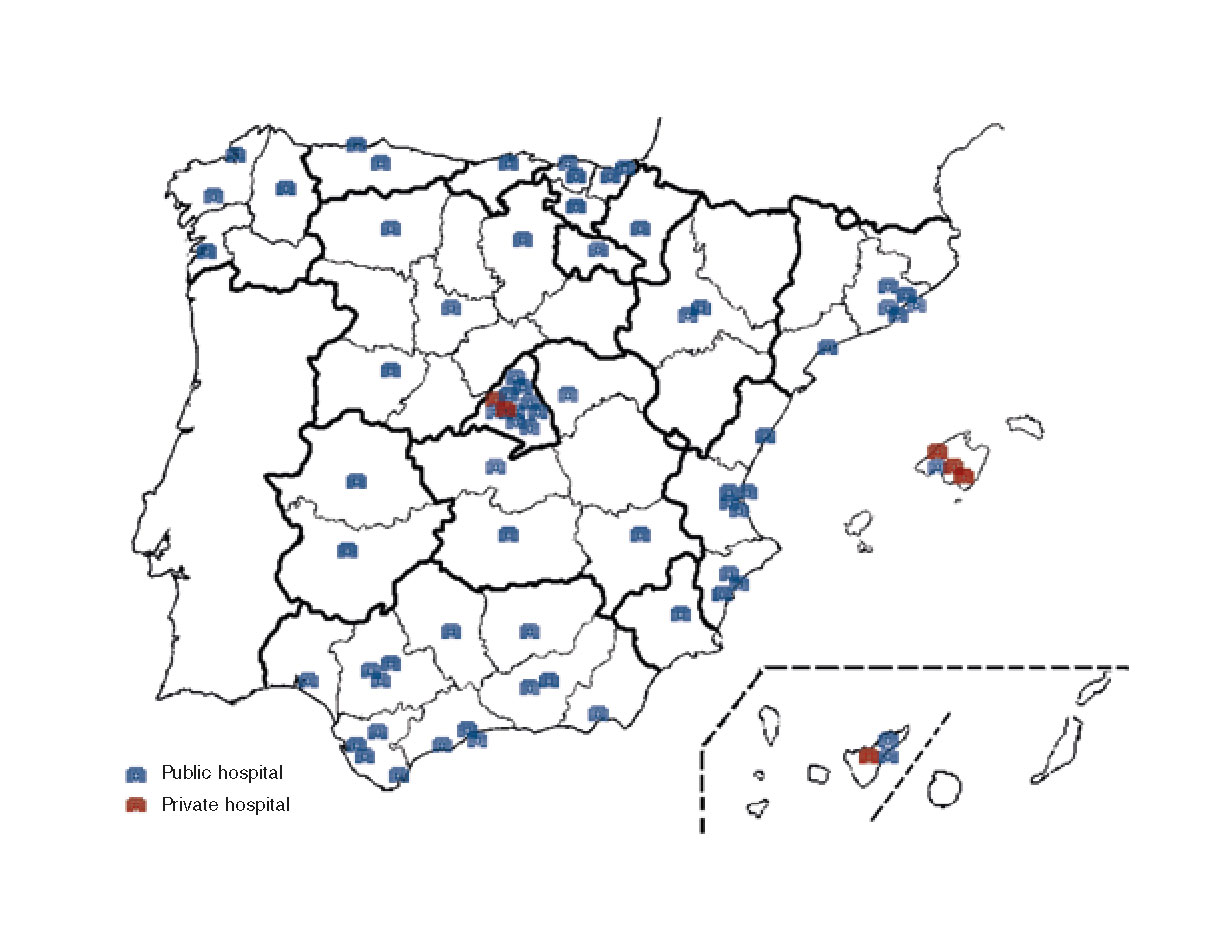
Out of the 823 invitations sent, 172 interventional cardiologists and SHCI members (21%) from 75 hospitals (71 public and 4 private) of the 17 Spanish autonomous communities responded to the survey. Figure 1 shows the location of the hospitals. Ninety-fivepoint-six percent of participants were part of infarction teams that remained available on a 24/7/365 basis, and 26% of them were the directors of their corresponding interventional cardiology unit (in 59% of participating centers, the person who responded to the survey was the director of the unit). The mean age of respondents was 45 ± 8 years (range, 28-66 years), [39-50 years]. The years of experienced performing primary angioplasty procedures were 9.5 ± 5.7 (range, 0-21), [5-13].
Figure 1. Map with the distribution of centers represented in the survey. Blue shows public hospitals and red shows private centers. Eight respondents did not tick the working center box and, therefore, are not represented on the map.
Annex 1 shows the participating centers by autonomous communities.
Specificities of pPCI programs
Regarding the management of STEMI, the number of annual pPCIs performed per center (considering the data provided by hospitals to the 20177 SHCI Registry) was 239 ± 112 (range, 14-587), while the number of angioplasties performed per STEMI per center (primary angioplasty, bailout angioplasty, and early angioplasty after effective thrombolysis) was 259 ± 110 (range, 15-596) per year.
On average there were 5 ± 1 interventional cardiologists (range, 2-9) and 8 ± 3 nurses (range, 2-25) per center as part of the infarction team.
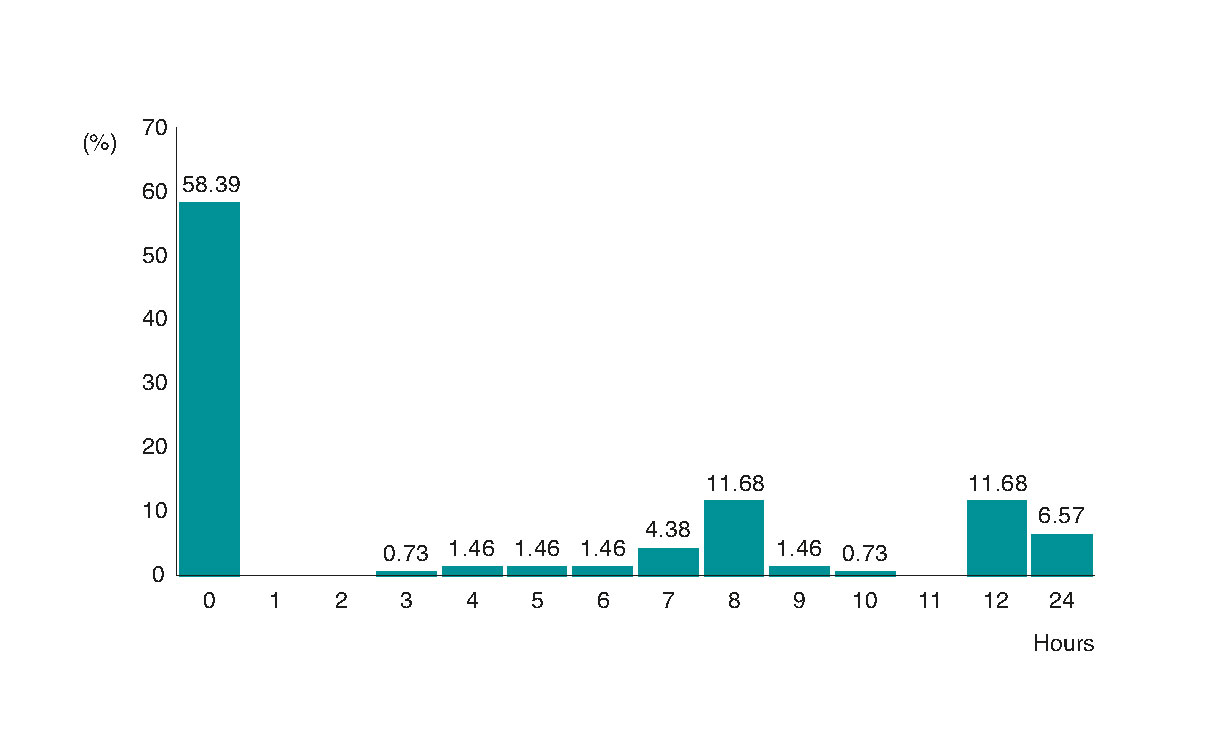
Infarction Code calls were available at all time. The distribution of the calls was mostly throughout days (82%), whereas in 18% of the cases, the period of continuous call spanned throughout 7 days/week. Seventy-two percent of respondents claimed to not have rest hours after being on call. Figure 2 shows the distribution of the number of hours of rest after performing a procedure while being on call; when there is a possibility of rest (which only happens in 54% of the cases), it occurs the next day.
Figure 2. Distribution of the number of hours of rest agreed after performing one procedure while on on-call duty.
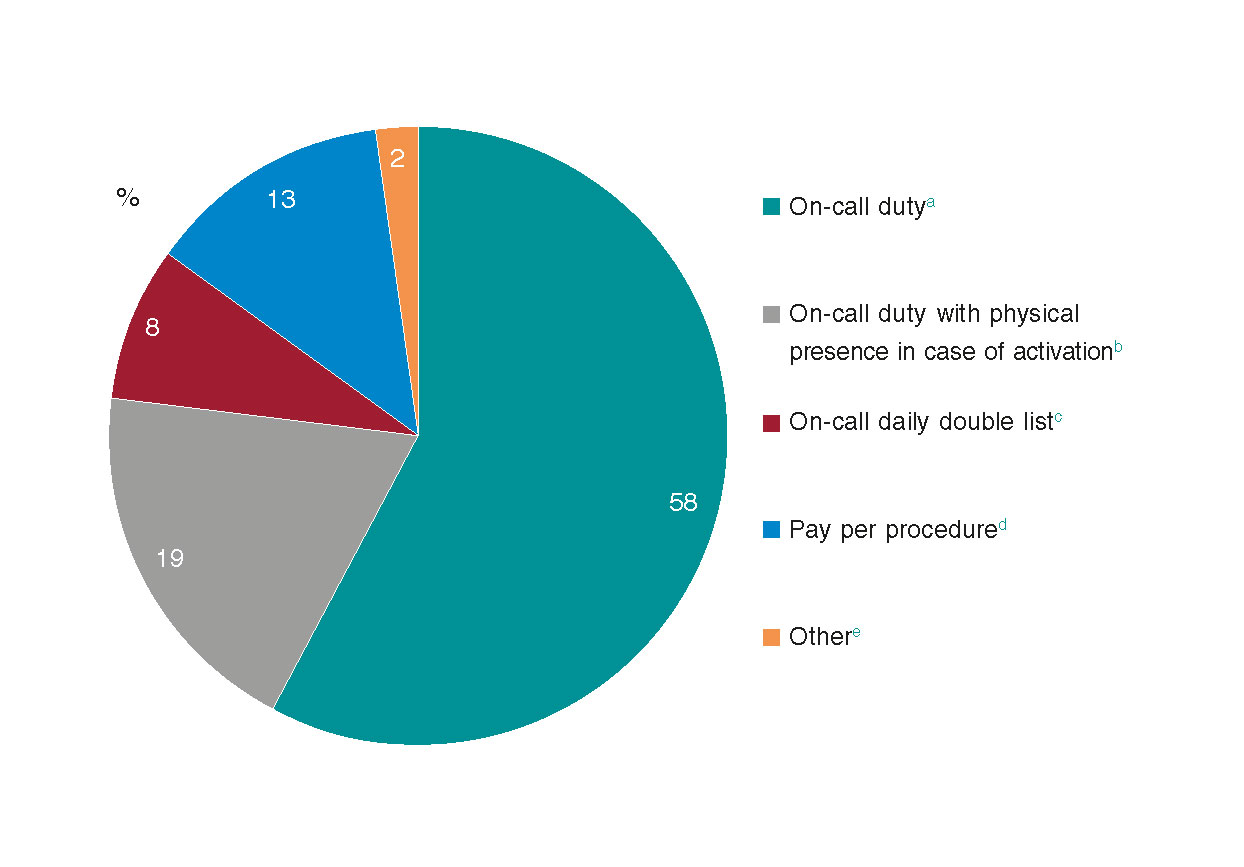
Figure 3 shows how on-call pay rates are arranged. There is a heterogeneous pattern but in almost two thirds of the cases, the pay rate is only location based regardless of the number of procedures performed. If pay rate from centers with the largest volumes of procedures performed while on call (> 300) is analyzed, we will see that these pay rates vary slightly: 58% to 45% for on-call duty, 19% to 25% for on-call physical presence, 8% to 10% for on-call daily double list, and from 13% to 16% for pay per procedure.
Figure 3. Pay per on-call duty within the Infarction Code initiative.
a Payment on an on-call duty basis only regardless of the activity performed.
b Payment on an on-call duty basis that in case of activation turns into payment on an on-call duty basis plus physical presence.
c Payment on an on-call duty basis with two interventional cardiologists on call.
d Payment per every procedure performed.
e Others includes 2 cases (1.2%) of payment on an on-call duty basis with 1 interventional cardiologist available during business days and 2 interventional cardiologists available during public holidays, plus payment of hours of physical presence per procedure performed, and 1 case (0.6%) of monthly payment on an on-call duty basis.
Opinions on the pPCI program
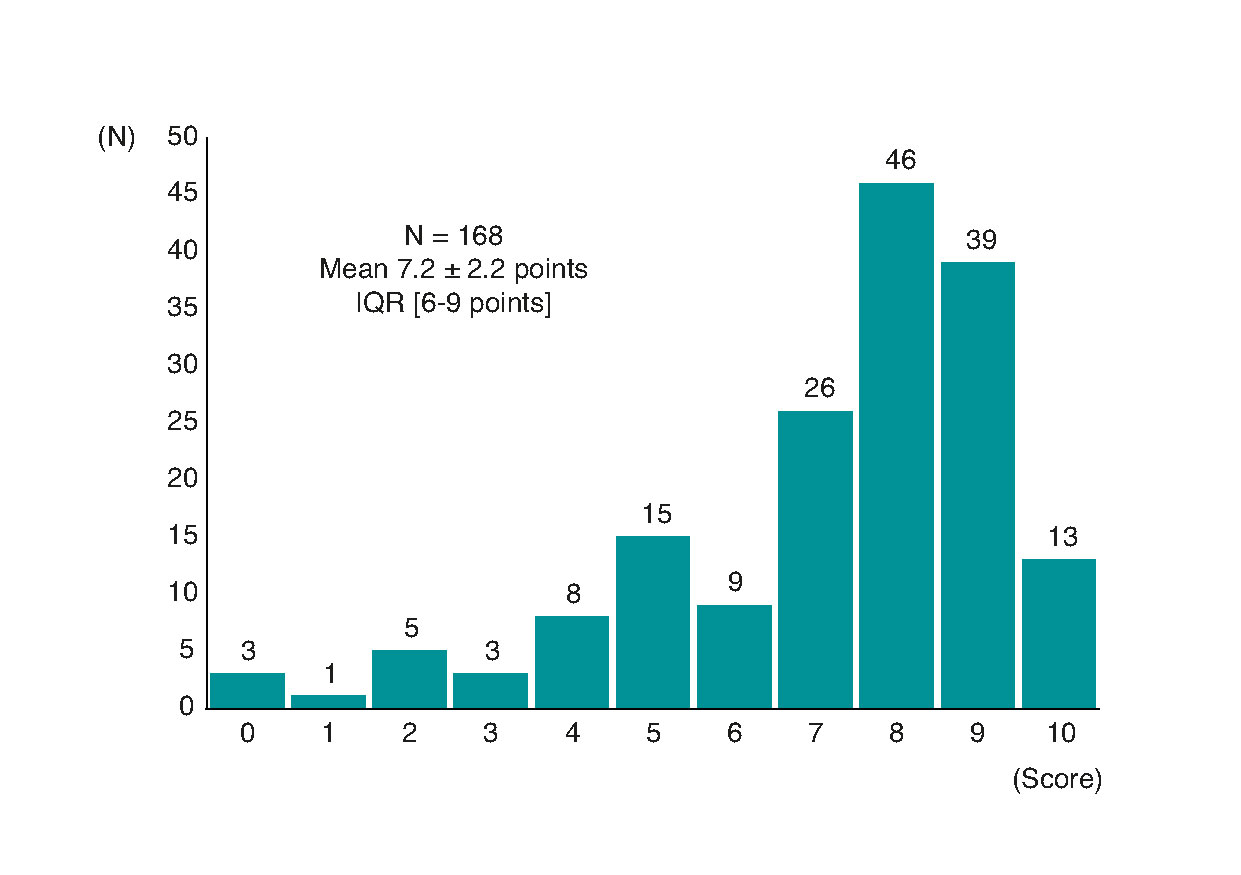
Figure 4 shows the distribution of the score attributed to the degree of satisfaction of the professionals involved in the Infarction Code initiative of their center on a scale from 0 to 10. Fourteen percent of respondents gave scores < 5 points, whereas 33% of respondents gave scores between 9 and 10 points.
Figure 4. Distribution of the score given on the degree of professional satisfaction after the implementation of the Infarction Code initiative (on a scale from 0 to 10). IQR, interquartile range.
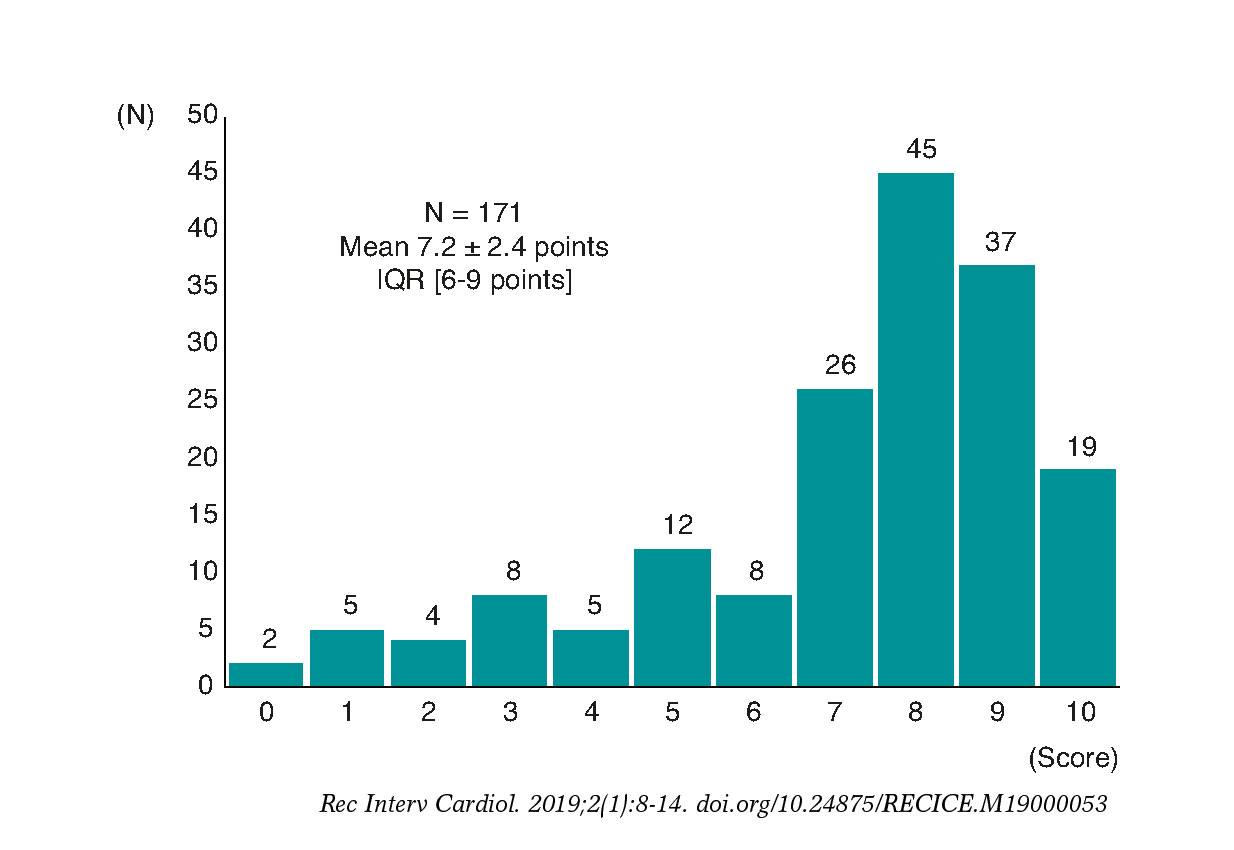
Figure 5 shows the distribution of the scores given to the question of the degree of satisfaction with the job done from the professional and not the patient’s point of view regarding the management of STEMI. Twelve percent of respondents gave scores < 5 points and 31% of respondents gave scores between 9 and 10 points. In this sense, 86% of respondents answered “yes” to the question «Do you think the management of STEMI patients can be improved? Table 2 shows the score attributed to the degree of satisfaction with the implementation of the Infarction Code initiative, and the score attributed to degree of professional satisfaction on the management of STEMI distributed across all autonomous communities.
Figure 5. Distribution of the score given on the degree of satisfaction with the job done from the professional and not the patient’s point of view on the management of ST-segment elevation acute myocardial infarction. IQR, interquartile range.
Table 2. Scores given to the questions on the degree of satisfaction after the implementation of the Infarction Code initiative from the professional point of view and itemized by autonomous community
| ¿Would you say that the implementation of the initiative carried out by your center was satisfactory? (0-10) | When it comes to the initiative, are you satisfied with your job in the professional aspect? (0-10) | Difference in the mean score given between the first and the second question | |
|---|---|---|---|
| Andalusia | 6,2 ± 2,6 (31) | 6,4 ± 2,4 (29) | +0,2 |
| Aragon | 6,6 ± 2,2 (7) | 7,1 ± 2,4 (7) | +0,5 |
| Canary Islands | 6,8 ± 1,5 (5) | 8,2 ± 0,8 (5) | +1,4 |
| Cantabria | 9 ± 1,2 (5) | 7,2 ± 3,1 (5) | −1,8 |
| Castile and Leon | 5,1 ± 2,8 (11) | 6,1 ± 1,9 (11) | +1 |
| Castile-La Mancha | 7,4 ± 2,5 (16) | 6,9 ± 3,2 (8) | −0,5 |
| Catalonia | 8 ± 2,3 (21) | 7,6 ± 2,2 (21) | −0,4 |
| Chartered Community of Navarre | 7 ± 1,8 (4) | 5,2 ± 3,6 (4) | −1,8 |
| Valencian Community | 6,9 ± 2,8 (16) | 7,2 ± 2,1 (16) | +0,3 |
| Community of Madrid | 7,2 ± 2,5 (25) | 7,3 ± 2,3 (24) | +0,1 |
| Extremadura | 6,5 ± 0,7 (2) | 7 ± 1,4 (2) | +0,5 |
| Galicia | 7,9 ± 1,7 (9) | 7,7 ± 1,2 (9) | −0,2 |
| Balearic Islands | 8,2 ± 0,8 (5) | 8,4 ± 0,5 (5) | +0,2 |
| La Rioja | 7 ± 0 (2) | 6 ± 2,8 (2) | −1 |
| Basque Country | 8,7 ± 0,8 (10) | 8,3 ± 0,5 (10) | −0,4 |
| Principalty of Asturias | 8,6 ± 0,9 (8) | 8,8 ± 1 (8) | +0,2 |
| Region of Murcia | 8 ± 0 (2) | 7,5 ± 0,7 (2) | -0,5 |
| Total | 7,2 ± 2,4 (177) | 7,2 ± 2,2 (168) | 0 |
|
The score given to each question is expressed as mean ± standard deviation. The numbers shown in brackets are indicative of the number of professionals who answered the question. |
|||
With respect to the perception of working conditions, 76% of respondents said that they did not rest enough after being activated while on call, 32% claimed that the personnel in charge of the calls is shorthanded, 63% thought that the responsibility involved in this procedure does not receive the recognition it deserves, and 85% of respondents agreed that the on-call pay rate is not right.
The survey included a blank box where the professional could list areas for improvement as part of the primary angioplasty program: 132 respondents (77%) wrote on this box and the answers given were about improving logistics (32%), pay rates (53%) or the hours of rest (47%).
Lastly, 55% of professionals said they would consider leaving these on-call mandatory programs once they were not compulsory anymore.
DISCUSSION
The survey on the needs of pPCI programs in Spain conducted among interventional cardiologists involved in these programs with a sample representative of all autonomous communities has shown 4 basic aspects: a) the assessment given to the Infarction Code initiative in terms of patients’ benefits and professional satisfaction is high; b) there are significant local and regional differences in how professionals perceive their own degree of satisfaction; c) there is a general feeling that there is room for improvement in 3 different fields in terms of patient care/infrastructure, hours of rest after activation, and pay per on-call duty; and d) over half of the respondents are seriously considering leaving these on-call mandatory programs once they become of an age when they are not compulsory anymore.
The identification of a series of deficiencies and shortfalls may put these pPCI programs in a situation of vulnerability that may eventually jeopardize their own sustainability. This has been one of the main goals of SHCI Infarction Code Working Group. One study analyzed the impact that the presence of infarction care networks had on mortality in the management of STEMI in Spain between 2003 and 2012 and showed significant differences among the different autonomous communities in the implementation of pPCI programs such as significant differences in hospital mortality among the different autonomous communities.6 However despite the improvements made over the last few years, these differences still stand.8 In this sense, up to 86% of respondents believe that there is still room for improvement in the management of heart attacks. Since 2012 there has been a growth of regional pPCI programs to the extent that to this day almost every single Spanish autonomous community has implemented a pPCI program for the management of STEMI .
The overall average score in the assessment of the Infarction Code initiative in terms of benefits for the patient and degree of professional satisfaction is high: 7.2 points scored by both items. However, when the different autonomous communities are studied separately, the scores of these two items change dramatically. Thus, the degree of satisfaction with how the Infarction Code initiative works varies significantly from the 5.1 points of Castile and León to the 8.7 points of the Basque Country. The degree of professional satisfaction varies as well from the 5.2 points of the Chartered Community of Navarre to the 8.8 points of the Principality of Asturias. The scores given to both questions also vary depending on the autonomous community. For example, the score given by the Canary Islands (1.4 points) to the degree of professional satisfaction, which is higher than the degree of professional satisfaction with the Infarction Code initiative, or the score given by Cantabria (1.9 points), which is lower. There is no question that these differences show heterogeneity in the way these programs have been implemented by each autonomous communities. Analyzing the causes in each autonomous community is not an easy task and cannot be done with the present survey. Still, overall, there are factors that may justify the results obtained.
On the one hand, the implementation of pPCI programs occurred with partial or incomplete prior analyses, limited official support, and poor resources. The implementation of the Infarction Code initiative has had a great impact on daily care since 30%-45% of all emergencies occur within business hours9 altering the normal functioning of the daily agenda and eventually leading to the cancellation of cases (hospitalized patients, scheduled cases or scheduled cases from other centers) or to unforeseen extensions of working hours to avoid these cancellations.
On the other hand, this survey shows that the sizing of the personnel involved in these Infarction Code initiatives is not right in many centers. The correct amount of professionals is required to take care of significant volumes of pPCIs during night time, and also to carry on with the activity scheduled by the unit for the next day and to make sure that these professionals get the hours of rest they need. In this sense, it is significant that up to 72% of respondents said that they did not have enough hours of rest after performing one procedure while on-call, and that on many occasions, these hours of rest were based on the actual healthcare possibilities and not on the needed rest per se. Performing these elective interventional procedures under conditions of lack of sleep and rest has been associated with a higher rate of suboptimal results.10
In this context it should be mentioned that many pPCI programs in Spain are not categorized as individual speciality programs. Therefore, the pay of these healthcare providers is no different from the pay of other providers who deal with urgent performances of lower complexity much less frequently and with low or no risk patients and that can often be scheduled with several hours in advance.
Even though the overall assessment of the pPCI programs made by professionals is high, the structural limitations found by this sUrvey can have a negative impact on the teams and eventually lead to lack of motivation in many of the professionals involved with these programs. It comes as no surprise that this can also impact the degree of excellence provided that should be the goal of all pPCI programs, especially if we take into account the special profile of the patients who benefit from these programs. The fact that over half of the respondents are already thinking about leaving these on-call mandatory programs once they become of an age when they won’t be eligible anymore can jeopardize the sustainability of these pPCI programs and put them in a situation of vulnerability. Ironically, this moment will come when these professionals are at their best and when they would have the best results. Eventually this may lead to a lack of recognition of these professionals from different points of view. In this sense, in each autonomous community, the ongoing monitoring and data measurement should include healthcare information, medical information, and the needs of all the professionals involved with the healthcare process in terms of which areas can be improved. The local and regional administrations should make sure that these pPCI programs are sustainable and certainly in our country they have shown a good cost-effective profile11 when the right investment has been made.
Limitations and strengths
The present study has some limitations. First, the number of participants is relatively low compared to the overall amount of SHCI members. However, the sample seems representative enough since not all SHCI members are involved with pPCI programs and because 75 centers from all autonomous communities were represented in the survey. Also, a 21% participation rate is clearly higher compared to the participation rate from another similar online survey where only 14% of all the possible candidates responded.12. Also, according to data published in the last SCHI registry, the number of active registered interventional cardiologists today is 3907 which amounts to a 44% participation rate. Secondly, the observational and cross-sectional nature of the study is a limitation per se.
The strength of this study is the fact that all Spanish autonomous communities were represented and with the anonymous nature of the survey that guarantees honest answers from respondents.
CONCLUSIONS
The survey on the needs of pPCI programs in Spain shows a high degree of satisfaction in the assessment of the system made by professionals, although with significant local and regional differences among the different autonomous communities. This survey has also allowed us to detect logistical, structural, and payment dysfunctions that may jeopardize the integrity of pPCI programs.
CONFLICTS OF INTERESTS
R. Moreno is an Associate Editor of REC: Interventional Cardiology.
WHAT IS KNOWN ABOUT THE TOPIC?
- Over the last few years, several regional infarction care networks have been implemented in Spain with heterogeneous structure and functioning.
- There is no information on the professional perspective on how these networks work or on the degree of professional and personal satisfaction of the interventional cardiologists involved with these procedures.
WHAT DOES THIS STUDY ADD?
- The assessment of the Infarction Code initiative in terms of benefits for the patient and professional satisfaction is fairly good, although there are significant regional differences in the way professionals perceive this satisfaction.
- There is generalized feeling that there is room for improvement in terms of patient care and infrastructure, hours of rest after activation, and pay per on-call duty.
- Under the actual conditions, over half of the respondents said they would consider leaving these on-call mandatory programs once they become of an age when they won’t be eligible anymore.
ANNEX 1. LIST OF PUBLIC HOSPITALS PER AUTONOMOUS COMMUNITY (INFORMATION ON THE WORKING CENTER WAS NOT PROVIDED IN 8 SURVEYS)
-
– Andalusia: Hospital Universitario Virgen Macarena, Hospital Universitario Virgen del Rocío, Hospital Universitario Virgen de las Nieves, Hospital Universitario de Jerez, Hospital Universitario Reina Sofía, Hospital Punta de Europa, Hospital Regional de Málaga, Hospital Universitario San Cecilio, Hospital Costa del Sol, Hospital Juan Ramón Jiménez, Hospital Universitario de Jaén, Hospital Universitario Puerta del Mar, Hospital Universitario Puerto Real, Hospital Universitario Virgen de Valme, Hospital Universitario Virgen de la Victoria, and Hospital Universitario Torrecárdenas.
-
– Aragon: Hospital Universitario Miguel Servet y Hospital Clínico Universitario Lozano Blesa.
-
– Canary Islands: Hospital Universitario Nuestra Señora de Candelaria y Hospital Universitario de Canarias.
-
– Cantabria: Hospital Universitario Marqués de Valdecilla.
-
– Castile and Leon: Hospital de León, Hospital Clínico Universitario de Valladolid, Hospital Clínico Universitario de Salamanca y Hospital Universitario de Burgos.
-
– Castile-La Mancha: Hospital Virgen de la Salud, Hospital General Universitario de Ciudad Real, Hospital General Universitario de Albacete y Hospital Universitario de Guadalajara.
-
– Catalonia: Hospital Universitari de Bellvitge, Hospital Universitari Germans Trias i Pujol, Hospital del Mar, Hospital Universitari Mútua Terrassa, Hospital de la Santa Creu i Sant Pau, Hospital Clínic de Barcelona, Hospital Universitari Joan XXIII y Hospital Universitari Vall d’Hebrón.
-
– Chartered Community Navarre: Complejo Hospitalario de Navarra.
-
– Valencian Community: Hospital de Alzira, Hospital General Universitari de Castelló, Hospital Clínic Universitari de València, Hospital Universitari i Politècnic La Fe, Hospital de Manises, Hospital Universitari Sant Joan d’Alacant, Hospital General Universitari d’Alacant y Hospital Universitari de Torrevieja-Elche-Vinalopó.
-
– Community of Madrid: Hospital Universitario 12 de octubre, Hospital Universitario Fundación de Alcorcón, Hospital Clínico San Carlos, Hospital Universitario Fundación Jiménez Díaz, Hospital General Universitario Gregorio Marañón, Hospital Universitario La Paz, Hospital Universitario de La Princesa, Hospital Universitario Puerta de Hierro, Hospital Universitario Ramón y Cajal, y Hospital Universitario de Torrejón.
-
– Extremadura: Hospital Universitario Infanta Cristina y Hospital Universitario de Cáceres.
-
– Galicia: Hospital Clínico Universitario de Santiago, Hospital Universitario de A Coruña, Hospital Universitario Lucus Augusti y Hospital Álvaro Cunqueiro.
-
– Balearic Islands: Hospital Universitari Son Espases.
-
– La Rioja: Hospital San Pedro.
-
– Basque Country: Hospital Universitario Basurto, Hospital Universitario Cruces, Hospital Universitario Araba y Hospital Universitario Donostia.
-
– Principality of Asturias: Hospital Universitario Central de Asturias y Hospital Universitario de Cabueñes.
-
– Region of Murcia: Hospital Clínico Universitario Virgen de la Arrixaca.
REFERENCES
1. Ibañez B, James S, Agewal S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation:The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology. Eur Heart J. 2017;39:119-177.
2. Kristensen SD, Laut KG, Fajadet J, et al. European Association for Percutaneous Cardiovascular Interventions. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011:current status in 37 ESC countries. Eur Heart J. 2014;35:1957-1970.
3. Knot J, Widimsky P, Wijns W, et al. How to set up an effective national primary angioplasty network:lessons learned from five European countries. Eurointervention. 2009,5:301-309.
4. Rodriguez-Leor O, Fernandez-Nofrerias E, Mauri J, et al. Integration of a local into a regional primary angioplasty action plan (the Catalan Codi Infart network) reduce time to reperfusion. Int J Cardiol. 2013;168:4354-4357.
5. Goicolea-Ruigómez J, Sabaté-Tenas M, Feldman M, Macaya C. The Current Status of Primary Percutaneous Coronary Intervention in Spain. Rev Esp Cardiol Supl. 2011;11C:15-20.
6. Cequier A, Ariza-SoléA, Elola FJ, et al. Impact on Mortality of Different Network Systems in the Treatment of ST-segment Elevation Acute Myocardial Infarction. The Spanish Experience. Rev Esp Cardiol. 2017;70:155-161.
7. Cid-Alvarez B, Rodriguez-Leor O, Moreno R, Perez de Prado A. Spanish Cardiac Catheterization and Coronary Intervention Registry. 27th Official Report of the Spanish Society of Cardiology Working Group on Cardiac Catheterization and Interventional Cardiology (1990-2017). Rev Esp Cardiol. 2018;71:1036-1046.
8. Mate Redondo C, Rodríguez-Pérez MC, Domínguez Coello S, et al. Hospital mortality in 415 798 AMI patients:4 years earlier in the Canary Islands than in the rest of Spain. Rev Esp Cardiol. 2018. http://dx.doi.org/10.1016/j.rec.2018.06.023.
9. Rodriguez-Leor O, Fernandez-Nofrerias E, Mauri F, et al. Analysis of reperfusion delay in patiens with acute myocardial infarction treated with primary angioplasty based on first medical contact and time of presentation. Rev Esp Cardiol. 2011;64:476-483.
10. Sandoval Y, Lobo AS, Somers VK, et al. Sleep deprivation in interventional cardiology:Implications for patient care and physician-health. Catheter Cardiovasc Interv. 2018;91:905-910.
11. Regueiro A, Bosch J, Martin-Yuste V, et al. Cost-effectiveness of an European ST-segment elevation myocardial infarction network:results from the Catalan Codi Infart network. BMJ Open. 2015;5:e009148.
12. Majani J, Di Tano G, Giardini A, et al. Prevalence of job-related distress and satisfaction in a nationwide cardiology setting:The IANUS –itAliaN cardiologists'Undetected distress Study. J Cardiovasc Med. 2016;17:587-594.