CASE PRESENTATION
We hereby present the case of a 73-year-old male with a past medical history of high blood pressure, diabetes mellitus type 2, dyslipidemia, and former smoker as cardiovascular risk factors. The patient showed chronic ischemic heart disease that started as unstable angina with coronary artery disease of the right and circumflex coronary arteries, undergoing complete percutaneous revascularization in 2008 with everolimus-coated stents.
Ten years later the patient suffered from a non-ST segment elevation acute coronary syndrome of inferior location with low blood pressure and need for vasoactive amines, which is why he was transferred to the cath. lab for an early invasive strategy.
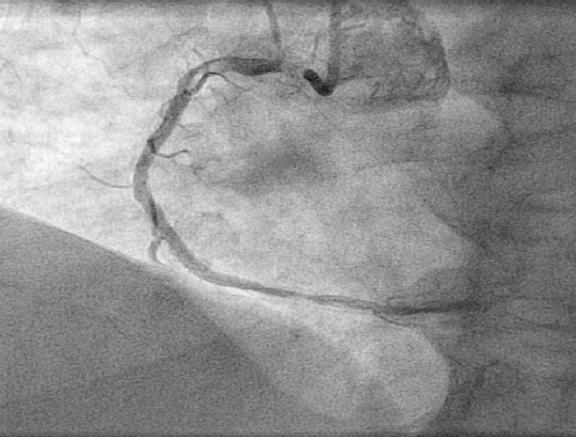
The diagnostic coronary angiography performed using the right radial access showed the presence of a plaque complicated with a thrombus in the ostium of the right coronary artery with Thrombolysis in Myocardial Infarction grade flow 3 (figure 1).
Figure 1. Acute complicated lesion in the ostium of the right coronary artery.
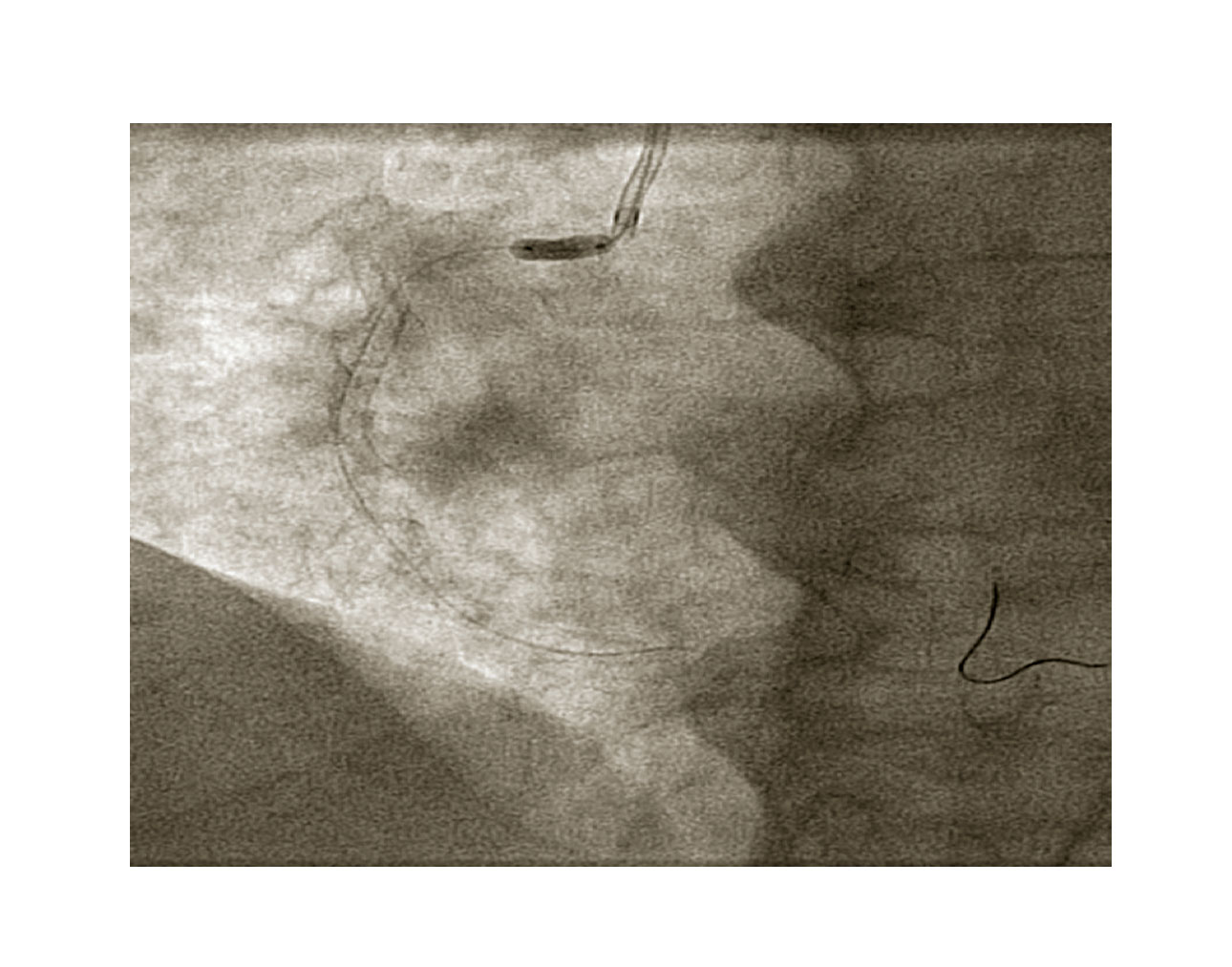
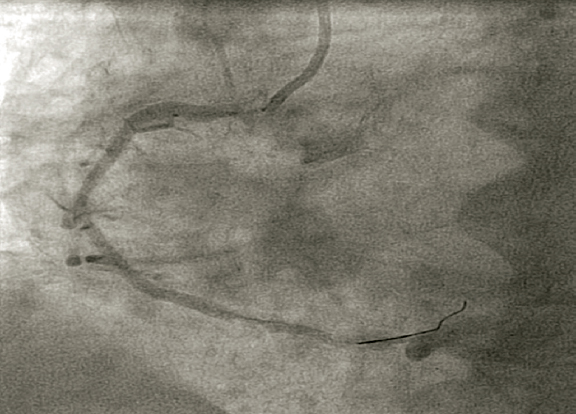
A 6-Fr JR guiding catheter and a Sion guidewire (Asahi) were selected for the procedure. Predilatation was attempted with a 3.5 × 10 mm noncompliant balloon (figure 2) and a 3.5 × 18 mm Orsiro sirolimus-eluted stent was implanted covering the ostium (figure 3).
Figure 2. Predilatation with one 3.5 × 18 mm noncompliant balloon inflated at 14 atm, with adequate expansion.
Figure 3. Angiography prior to the implantation of the stent adjusted to the ostium of the right coronary artery.
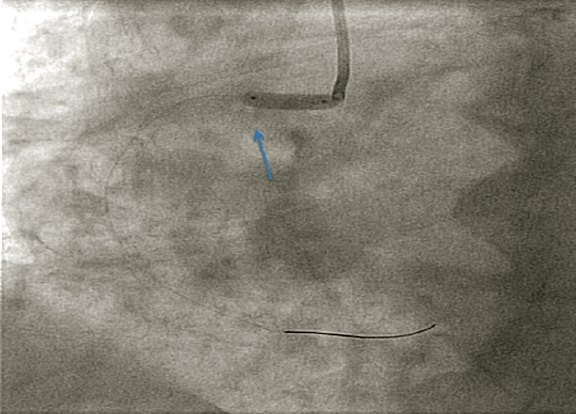
When the stent was deployed and inflated at 6 atm, with the patient in a state of agitation given his hemodynamic situation, he took a deep breath that caused the displacement of the stent towards the aorta (figure 4), that was deployed completely outside the ostium of the right coronary artery.
Figure 4. Stent displaced towards the aorta is observed. The arrow shows the mark of calcium in the sinus of Valsalva.
Therefore, we found ourselves with one under-expanded, displaced or loose stent inside the aorta that made maneuverability difficult with an uncovered thrombus in a complex ostial lesion and in the clinical context of an acute coronary syndrome.