CASE RESOLUTION
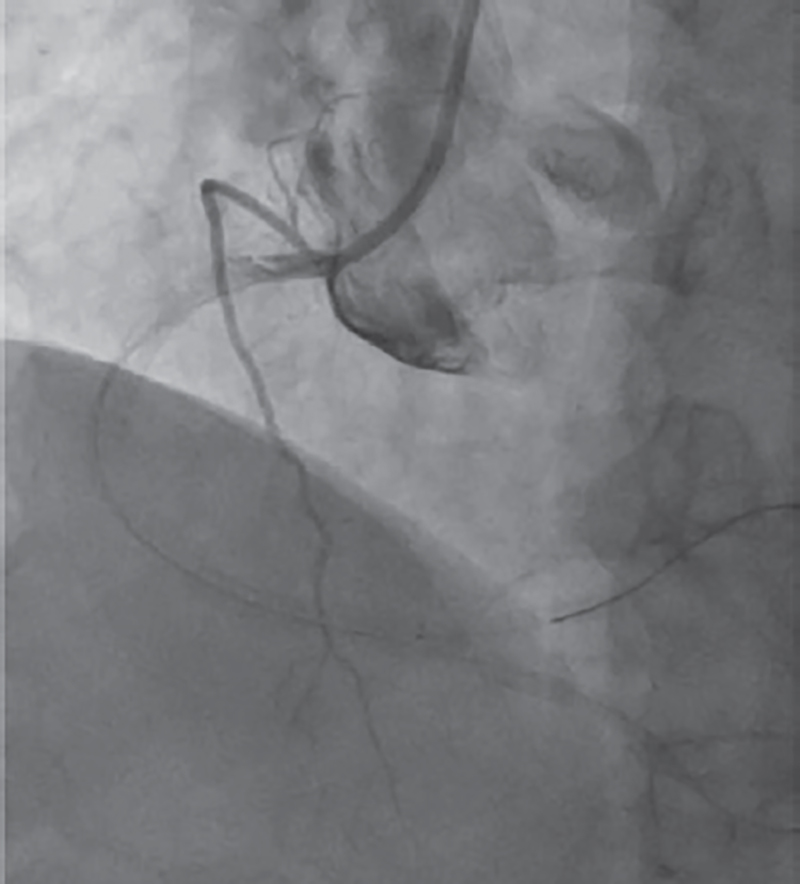
Intensive intracoronary vasodilators, including intracoronary nitrates and adenosine also proved ineffective. A total of 0.3 mg/Kg of enoxaparin were given during the procedure. Finally, intracoronary fibrinolysis was attempted with the administration of tenecteplase (8000 IU). About 10 minutes after instillation, recanalization was not possible, and the procedure was terminated. A type 4a myocardial infarction was diagnosed and an additional 48-hour course of eptifibatide was administered (bolus of 180 µg/Kg followed by the perfusion of 2 µg/Kg/min) (figure 1).
Figure 1. Angiography after instilling 8000 IU of tenecteplase with no repermeabilization; then, the procedure was terminated.
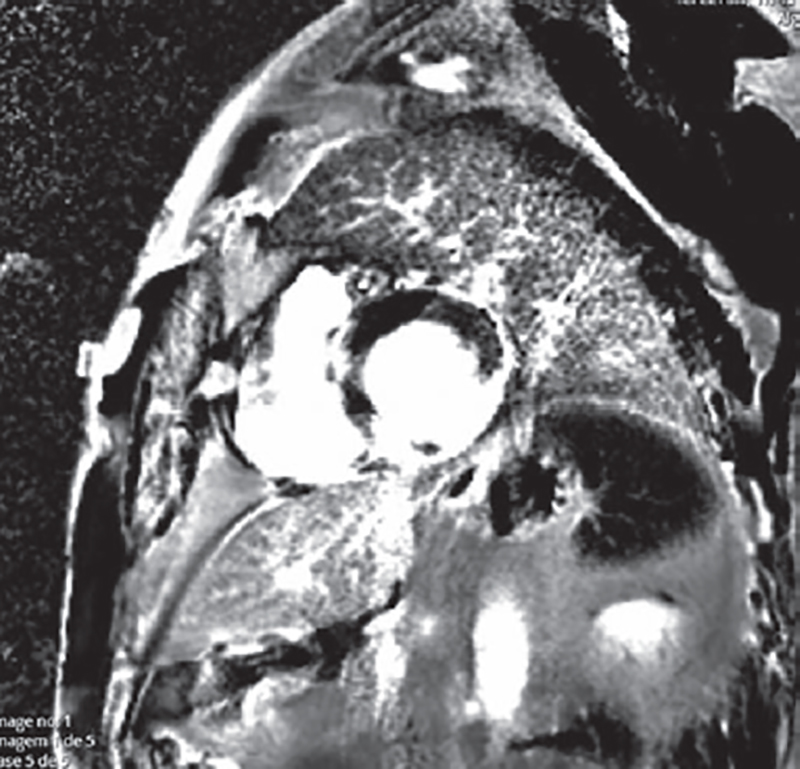
After the procedure, the patient complained of chest pain and an ST-segment elevation was seen. Pain was successfully controlled within the first 12 hours. The troponin peak levels were 113 ng/mL. A triple antithrombotic strategy with aspirin, ticagrelor, and full-dose enoxaparin was maintained during hospitalization (1 week). Serial echocardiographic evaluation revealed the presence of mild left ventricular dysfunction with severe inferior wall hypokinesis. Right ventricular systolic function was depressed (a 12 mm tricuspid annular plane systolic excursion [TAPSE]). The patient was discharged on dual antiplatelet therapy. The patient remained asymptomatic at 5-month follow-up. Cardiac magnetic resonance imaging (figure 2) showed a normal-sized right ventricle with preserved function, but mild hypokinesis of the right ventricle free wall. Middle and basal segments showed late gadolinium enhancement. Left ventricular systolic function remained slightly depressed with akinesia of the inferior-lateral and inferior walls. Test for residual ischemia was negative.
Figure 2. Short-axis cardiac magnetic resonance imaging.
This case report illustrates a rare complication of a frequent procedure. Our patient developed an acute coronary occlusion after an attempted elective angioplasty. Furthermore, we rushed and tried revascularization through aspiration and intracoronary fibrinolysis. The no-reflow phenomenon was most likely associated with local thrombosis; nonetheless, mechanisms like iatrogenic coronary dissection are plausible. Intracoronary imaging was considered dangerous in this setting due to the possibility of progression into a hypothetic dissection. Despite the fact that these techniques failed, the case illustrates the numerous possibilities for revascularization. The underlying autoimmune disease and chronic corticosteroid therapy may have contributed to this thrombotic catastrophe.
In the modern era of potent antiplatelet agents, the risk of myocardial infarctions associated with percutaneous coronary revascularization is rare. In many cases, there is an underlying condition that appears to increase the risk of thrombotic events. Moreover, the treatment of type 4a infarcts is difficult, and the emergence of new bailout techniques is essential. Intracoronary fibrinolysis has been suggested as a rescue therapy for patients with high thrombotic burden, but it may become deleterious in certain scenarios due to increasing bleeding complications.1,2
Our case shows that not all type 4a infarctions have a favorable outcome, but also highlights the variety of percutaneous approaches that remain at our disposal for the management of these rare complications. The recovery of right ventricular systolic function highlights the adaptability of the coronary tree and right circulation.3 A written informed consent was obtained from the patient.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
R. Flores analyzed data and designed the manuscript. J. Costa, C. Braga, C. Vieira, and C. Quina-Rodrigues revised the manuscript.
CONFLICTS OF INTEREST
None reported.
SUPPLEMENTARY DATA
Vídeo 1. Flores R. DOI: 10.24875/RECICE.M22000306
Vídeo 2. Flores R. DOI: 10.24875/RECICE.M22000306
Vídeo 3. Flores R. DOI: 10.24875/RECICE.M22000306
Vídeo 4. Flores R. DOI: 10.24875/RECICE.M22000306
REFERENCES
1. Unzue L, Garcia E, Teijeiro R, et al. Local Intracoronary Fibrinolysis in Acute Myocardial Infarction of Ectatic Coronary Arteries in the Post-Abciximab Era. Cardiovasc Revasc Med. 2021;32:69-74.
2. Kelly RV, Crouch E, Krumnacher H, et al. Safety of adjunctive intracoronary thrombolytic therapy during complex percutaneous coronary intervention: initial experience with intracoronary tenecteplase. Catheter Cardiovasc Interv. 2005;66:327–332.
3. Addetia K, Patel AR. Beyond right ventricular size and function: the importance of evaluating the right ventricle’s capacity for recovery. Expert Rev Cardiovasc Ther. 2014;12:1269-1273.