ABSTRACT
Introduction and objectives: The COVID-19 epidemic and the declaration of the state of alarm have led to a decrease in healthcare activity in interventional cardiology units. The objective of this study is to quantify these changes in activity, with special interest in the treatment of patients with ST-segment elevation myocardial infarction (STEMI).
Methods: A telematic survey of 81 centers involved in STEMI networks in the 17 autonomous communities of Spain. Information was collected on diagnostic activity, percutaneous coronary intervention (PCI), structural interventions, and PCI in STEMI on changes in the organization of STEMI networks, and on the prevalence of COVID-19 among interventional cardiologists. Data was compared for the week of February 24 through March 1 (before the outbreak) and for the week of March 16 through March 22 (during the outbreak).
Results: Response has been obtained from 73 centers (90%). A very significant decrease in the number of diagnostic procedures (─56%), PCI (─48%), structural interventions (─81%) and PCI in STEMI (─40%) has been observed. A slight increase in the use of pharmacological thrombolysis has been reported, although primary angioplasty remains the leading reperfusion strategy. Up to 5% of interventional cardiologists (17) had COVID-19.
Conclusions: An important reduction in the activity in interventional cardiology has been observed during the COVID-19 epidemic. Likewise, a great decrease has been detected in the number of patients treated in the STEMI networks, with the risk of increased morbidity and mortality that this represents. Scientific societies and health authorities have to promote that patients presenting STEMI compatible symptoms proceed with no delay to access the health system to receive reperfusion treatment in an appropriate way.
Keywords: STEMI network. COVID-19. Primary angioplasty. Survey. Pandemic.
RESUMEN
Introducción y objetivos: La epidemia de COVID-19 y la declaración del estado de alarma han propiciado una disminución en la actividad en la cardiología intervencionista. El objetivo de este estudio es cuantificar esta disminución, con especial interés en el funcionamiento del código infarto.
Métodos: Se realizó una encuesta telemática a 81 centros de las 17 comunidades autónomas españolas con procedimientos de código infarto. Se recogió información sobre la actividad diagnóstica, el intervencionismo coronario, el intervencionismo estructural y el intervencionismo en el seno del infarto agudo de miocardio con elevación del segmento ST (IAMCEST) sobre cambios en la organización de las redes del infarto y sobre la afección por COVID-19 de las plantillas de cardiología intervencionista. Se compararon 2 periodos: uno entre el 24 de febrero y el 1 de marzo (antes del inicio de la pandemia en España) y el otro entre el 16 y el 22 de marzo (durante la pandemia).
Resultados: Se obtuvo respuesta de 73 centros (90%) que evidenció una disminución significativa en el número de procedimientos diagnósticos (─56%), terapéuticos coronarios (─48%), terapéuticos estructurales (─81%) y en el seno del IAMCEST (─40%). Se indicó un leve incremento en el uso de trombolisis. Se diagnosticó infección por COVID-19 en 17 cardiólogos intervencionistas (5%).
Conclusiones: Se observó una reducción importante de la actividad asistencial durante la epidemia de COVID-19 y una gran disminución en el número de pacientes tratados con IAMCEST, con el riesgo de incremento de morbimortalidad que esto supone. Las sociedades científicas y autoridades sanitarias deberían promover que los pacientes con síntomas compatibles con IAMCEST demanden asistencia al sistema sanitario para poder recibir el tratamiento de reperfusión de forma adecuada.
Palabras clave: Código Infarto. COVID-19. Angioplastia primaria. Encuesta. Pandemia.
Abreviations: ACI-SEC: Interventional Cardiology Association of the Spanish Society of Cardiology; STEMI: ST-segment elevation myocardial infarction.
INTRODUCTION
The COVID-19 pandemic caused by the SARS-CoV-2 virus has seriously overloaded the Spanish healthcare system. On March 14, 2020 a national state of emergency was declared in Spain with a special call to house confinement in an attempt to stop the progression of the pandemic.1. As a consequence, the management of other conditions, among them cardiovascular diseases, has changed. This can be especially significant when it comes to the urgent management of myocardial infarction that, in our country, has been the responsibility of specialized networks for quite some time with primary percutaneous coronary intervention as first-line therapeutic option.2 The Interventional Cardiology Association of the Spanish Society of Cardiology (ACI-SEC) has taken a proactive approach under the current circumstances with the publication of 2 consensus documents; on the one hand, a document on the invasive approach of ischemic and structural heart disease.3 On the other hand, another document on the management of catheterization laboratories for the performance of cardiac invasive procedures.4
ACI-SEC Working Group on the Infarction Code has developed different actions to promote specialized networks for the management of myocardial infarction and percutaneous coronary intervention as first-line of therapy for patients with ST-segment elevation myocardial infarction (STEMI). One of the main actions taken is the Infarction Code Registry. During 2019 and for 3 months this registry collected data from 5241 consecutive patients in whom the infarction code had been activated in 81 public centers from specific care networks in the 17 Spanish autonomous communities. Using the specific infrastructure of this registry, ACI-SEC has conducted a survey to quantify the degree of damage caused by the COVID-19 pandemic to the catheterization laboratories of our country with special attention to how the infarction code actually works.
Methods
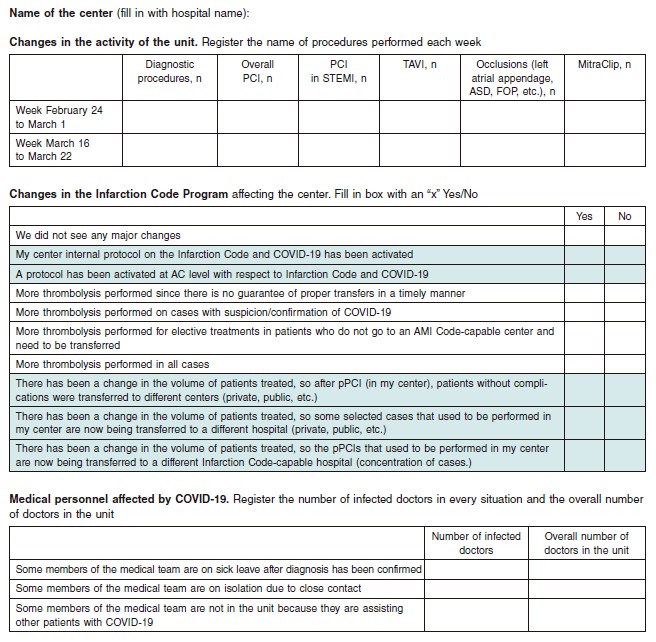
A remote survey was conducted among 81 centers that participated in the Infarction Code Registry. Almost all centers were part of the specific infarction care networks (only one center did not participate in the survey). The survey was sent back on March 24 and answers were received until March 30; the content of the survey is shown on figure 1.
Figure 1. Questionnaire filled out by each center. AC, autonomous communities; AMI, acute myocardial infarction; ASD, atrial septal defect; PCI, percutaneous coronary intervention; PFO, patent foramen ovale; pPCI, primary percutaneous coronary intervention; TAVI, transcatheter aortic valve implantation; STEMI, ST-segment elevation myocardial infarction.
The primary objective can be divided into 3 main points: a) quantify the changes in the volume of patients assisted by the healthcare system: diagnostic procedures, therapeutic coronary interventional procedures, therapeutic procedures for the management of structural heart disease, and therapeutic procedures in the STEMI setting; b) assess the changes caused to the activity of the infarction code by the COVID-19 pandemic; and c) assess the impact of COVID-19 on interventional cardiologists health status and activity.
Data on the activity displayed were collected during the week of February 24 through March 1 (prior to the start of the pandemic in our country) and during the week of March 16 through March 22 (during the pandemic). We should mention that during the first week there was a local festivity in Andalusia (February 28) and in Canary Islands (February 25) and during the second week there was another local festivity (March 19) in the autonomous communities of Castile-La Mancha, Region of Murcia, Chartered Community of Navarre, Valencian Community, Basque Country, and Galicia.
Results
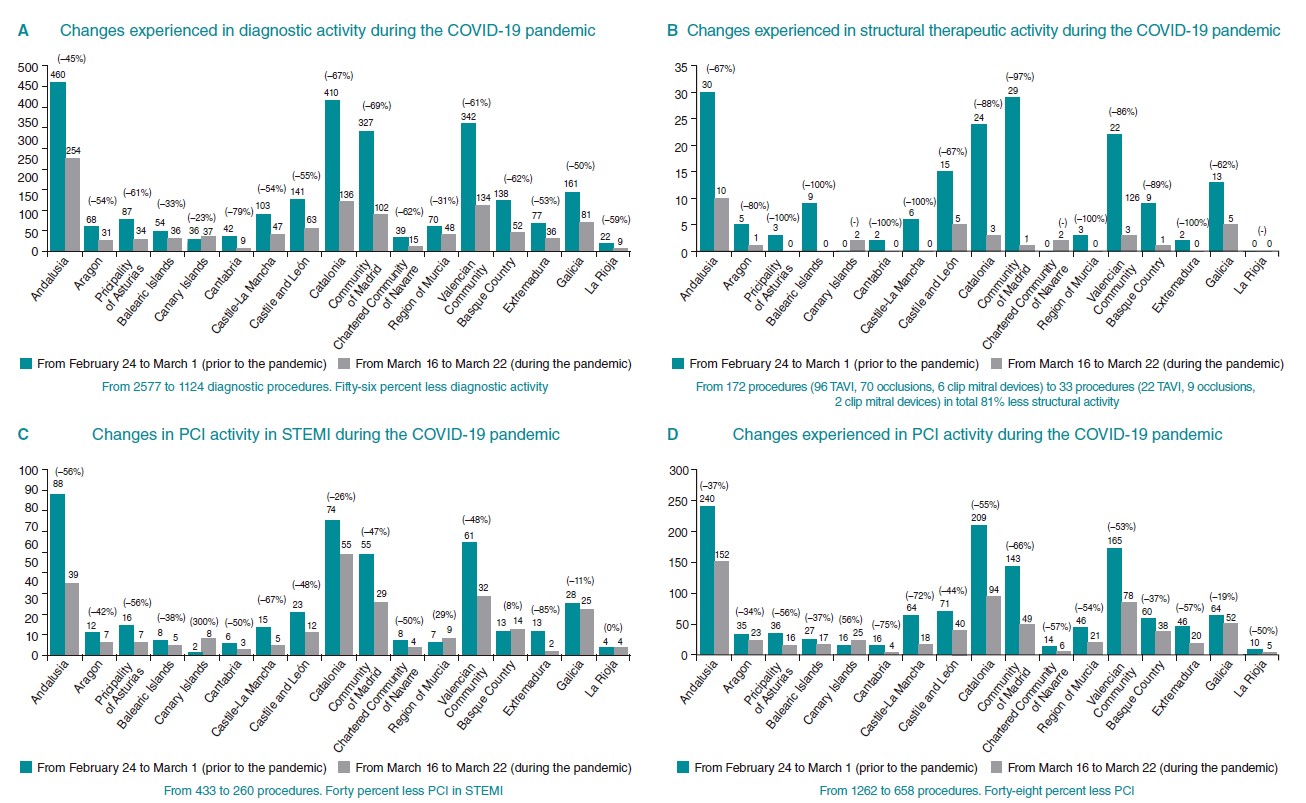
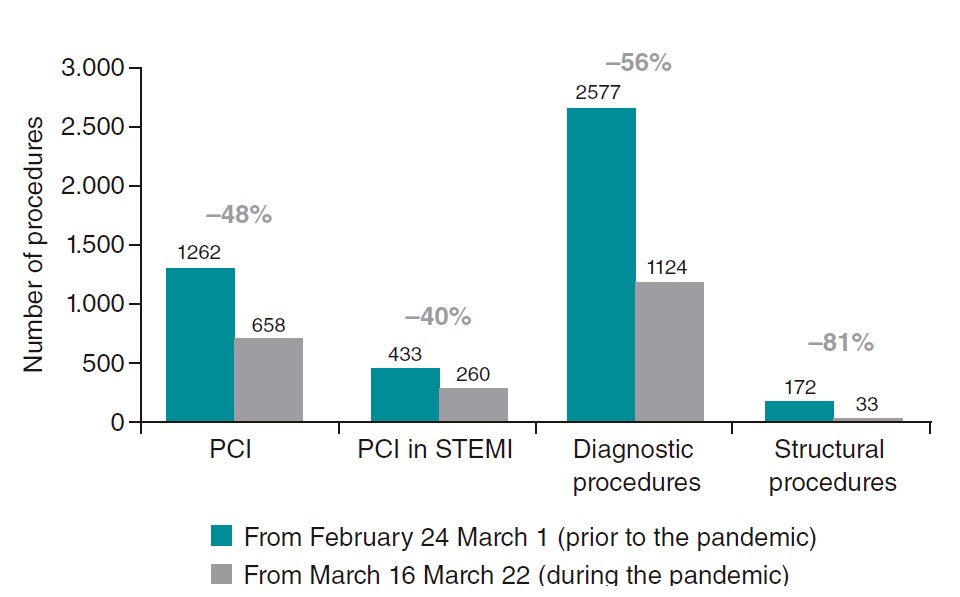
Data from 73 centers were received (90% of the total). The nationwide overall data showed a significant reduction in the number of diagnostic procedures (–56%), therapeutic coronary interventional procedures (–48%), structural therapeutic procedures (–81%), and procedures performed in the STEMI setting (–40%). Overall data and data by autonomous communities are shown on table 1, table 2, table 3, table 4 y en la figure 2. The overall data for Spain is shown on figure 3.
Table 1. Variation in the number of diagnostic procedures performed by autonomous community
| Autonomous Community | Weekly diagnostic procedures performed prior to the COVID-19 pandemic | Weekly diagnostic procedures performed during the COVID-19 pandemic | Variation, % |
|---|---|---|---|
| Andalusia | 460 | 254 | -45 |
| Aragon | 68 | 31 | -54 |
| Principality of Asturias | 87 | 34 | -61 |
| Balearic Islands | 54 | 36 | -33 |
| Canary Islands | 36 | 37 | -23 |
| Cantabria | 42 | 9 | -79 |
| Castille-La Mancha | 103 | 43 | -54 |
| Castille and León | 141 | 63 | -55 |
| Catalonia | 410 | 136 | -67 |
| Community of Madrid | 327 | 102 | -67 |
| Chartered Community of Navarre | 39 | 15 | -62 |
| Region of Murcia | 70 | 48 | -31 |
| Valencian Community | 342 | 134 | -61 |
| Basque Country | 138 | 52 | -62 |
| Extremadura | 77 | 36 | -53 |
| Galicia | 161 | 81 | -50 |
| La Rioja | 22 | 9 | -59 |
| Total | 2.577 | 1.124 | -56 |
|
* During the week prior to the COVID-19 pandemic there was a local festivity in the middle of the week in Andalusia (February 28) and Canary Islands (February 25) and during the COVID-19 pandemic week there was a local festivity in the autonomous communities of Galicia, Region of Murcia, Chartered Community of Navarre, Basque Country, and Valencian Community (March 19). |
|||
Table 2. Variation in the number of therapeutic coronary interventional procedures by autonomous community*
| Autonomous Community | Weekly therapeutic coronary interventional procedures before the COVID-19 pandemic | Weekly therapeutic coronary interventional procedures during the COVID-19 pandemic | Variation, % |
|---|---|---|---|
| Andalusia | 240 | 152 | -37 |
| Aragon | 35 | 23 | -34 |
| Principality of Asturias | 36 | 16 | -56 |
| Balearic Islands | 27 | 17 | -37 |
| Canary Islands | 16 | 25 | 56 |
| Cantabria | 16 | 4 | -75 |
| Castille-La Mancha | 64 | 18 | -72 |
| Castille and León | 71 | 40 | -44 |
| Catalonia | 209 | 94 | -55 |
| Community of Madrid | 143 | 49 | -66 |
| Chartered Community of Navarre | 14 | 6 | -57 |
| Region of Murcia | 46 | 21 | -54 |
| Valencian Community | 165 | 78 | -53 |
| Basque Country | 60 | 38 | -37 |
| Extremadura | 46 | 20 | -57 |
| Galicia | 64 | 52 | -19 |
| La Rioja | 10 | 5 | -50 |
| Total | 1.262 | 658 | -48 |
|
* During the week prior to the COVID-19 pandemic there was a local festivity in the middle of the week in Andalusia (February 28) and Canary Islands (February 25) and during the COVID-19 pandemic week there was a local festivity in the autonomous communities of Galicia, Region of Murcia, Chartered Community of Navarre, Basque Country, and Valencian Community (March 19). |
|||
Table 3. Variation in the number of procedures in the STEMI setting by autonomous community*
| Autonomous community | Weekly procedures in the STEMI setting before the COVID-19 pandemic | Weekly procedures in the STEMI setting during the COVID-19 pandemic | Variation, % |
|---|---|---|---|
| Andalusia | 88 | 39 | -56 |
| Aragon | 12 | 7 | -42 |
| Principality of Asturias | 16 | 7 | -56 |
| Balearic Islands | 8 | 5 | -38 |
| Canary Islands | 2 | 8 | 300 |
| Cantabria | 6 | 3 | -50 |
| Castille-La Mancha | 15 | 5 | -67 |
| Castille and León | 23 | 12 | -48 |
| Catalonia | 74 | 55 | -26 |
| Community of Madrid | 55 | 29 | -47 |
| Chartered Community of Navarre | 8 | 4 | -50 |
| Region of Murcia | 8 | 4 | -50 |
| Valencian Community | 61 | 32 | -48 |
| Basque Country | 13 | 14 | 8 |
| Extremadura | 13 | 2 | -85 |
| Galicia | 28 | 25 | -11 |
| La Rioja | 4 | 4 | - |
| Total | 433 | 260 | -40 |
|
STEMI: ST-segment elevation myocardial infarction. |
|||
Table 4. Variation in the number of structural interventional procedures by autonomous community*
| Autonomous Community | Weekly structural interventional procedures before the COVID-19 pandemic | Weekly structural interventional procedures during the COVID-19 pandemic | Variation, % |
|---|---|---|---|
| Andalusia | 30 | 10 | -67 |
| Aragon | 5 | 1 | -80 |
| Principality of Asturias | 3 | 0 | -100 |
| Balearic Islands | 9 | 0 | -100 |
| Canary Islands | 0 | 2 | - |
| Cantabria | 2 | 0 | -100 |
| Castille-La Mancha | 6 | 0 | -100 |
| Castille and León | 15 | 5 | -67 |
| Catalonia | 24 | 3 | -88 |
| Community of Madrid | 29 | 1 | -97 |
| Chartered Community of Navarre | 0 | 2 | - |
| Region of Murcia | 3 | 0 | -100 |
| Valencian Community | 22 | 3 | -86 |
| Basque Country | 9 | 1 | -89 |
| Extremadura | 2 | 0 | -100 |
| Galicia | 13 | 5 | -62 |
| La Rioja | 0 | 0 | - |
| Total | 172 | 33 | -81 |
|
The procedures included are transcatheter aortic valve implantation, appendage occlusion, closures of interatrial and intraventricular communications, foramen ovale, perivalvular leaks, mitral or tricuspid clip device. |
|||
Figure 2. Changes experienced in Spain in different healthcare activities during the current COVID-19 pandemic on an AC basis. A: changes experienced in diagnostic activity; B: changes experienced in structural therapeutic activity; C: changes experienced in PCI activity in the STEMI setting; D: changes experienced in PCI activity. AC, autonomous communities; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; TAVI, transcatheter aortic valve implantation.
Figure 3. Changes experienced in Spain in different healthcare activities during the current COVID-19 pandemic. STEMI, ST-segment elevation myocardial infarction.
From March 16 through March 22 a total of 40 centers (56%) followed a center specific protocol for the management of patients with COVID-19. On the other hand, in 13 centers (18%) a specific protocol from the infarction code network was followed for the management of patients with COVID-19.
We saw a slight change in the indication for reperfusion treatment in 2 centers (in the Community of Madrid and the Basque Country) that indicated a greater use of thrombolysis due to the inability to transfer patients to the infarction code center in a timely manner; 4 centers (2 in the Region of Murcia, 1 in the Community of Madrid, and 1 in Aragon) reported a greater use of thrombolysis in cases of patients with suspicion or confirmation of COVID-19; finally 3 centers (1 in Aragon, 1 in the Community of Madrid, and 1 in the Region of Murcia) reported a greater use of thrombolysis for elective treatment in patients admitted to non-PCI centers and who required transfer to a different center.
Some hospitals reported a change in the management before percutaneous coronary interventions hadbeen detected, in such a way that in 14 centers (1 in the Community of Madrid, 8 in Catalonia, 1 in Castile and León, 3 in Andalusia, and 1 in the Balearic Islands) the patients treated with uncomplicated percutaneous coronary intervention were transferred to other centers for their follow-up; in 4 centers (2 in the Community of Madrid and 2 in Catalonia) some selected cases that used to be treated at the center were treated somewhere else; in 4 centers (1 in the Valencian Community, 1 in the Basque Country and 2 in the Community of Madrid) there was a change in the volume of patients to the extent that all cases of percutaneous coronary intervention that used to be performed at the center were performed somewhere else.
Finally, on the degree of infection of the interventional cardiologists who perform percutaneous coronary interventions, of a total of 339 healthcare workers 17 were infected with COVID-19 (5%), 10 needed isolation because they had been in close contact (3%), and 27 quit interventional cardiology related practices to assist patients with COVID-19 (8%).
Discussion
The results of this study show a significant decrease of interventional cardiology procedures performed after the COVID-19 pandemic was declared in our country. The 40% decrease in interventional procedures performed in the STEMI setting is particularly disturbing. Also, we should mention here the implementation of local or regional protocols to assist these patients in many centers and, last but not least, the significantly high rate of contagion among healthcare workers. We anticipate that with the progression of the pandemic this activity will gradually drop in several centers and many more healthcare workers will be infected with COVID-19.
Back in 2018 a total of 21261 interventional procedures were performed in our country in the STEMI setting.2 During the COVID-19 pandemic patients still suffer from STEMI. A recent study on the management of infarctions in Hong Kong, China during the COVID-19 pandemic showed that the time elapsed between the infarction until care was received delayed significantly with median times since symptom onset until the first medical contact of 318 min on average. In the cases managed before the pandemic, median time was only 82 minutes.5 Our data confirm that added to this additional delay, there is a significant number of patients with STEMI who don’t seek medical attention. The reason may be that they are afraid of being infected at the hospitals. This is especially worrying since many patients with STEMI end up with sudden death due to early ventricular fibrillation and never have the chance to be treated.6 The remaining times until reperfusion—including in-hospital times—were also significantly delayed in the Hong Kong study.5 We can expect something similar to happen here in Spain.
We are therefore faced with a very unfavorable scenario in patients with STEMI. On the one hand, many will not seek medical attention and, on the other , for those who seek it, time to reperfusion will be longer than usual. In this situation, STEMI driven mortality is expected to grow, due to an increase in sudden out-oh-hospital death and longer ischemia times. Besides, the lack of or the delay in reperfusion will increase the incidence of heart failure, cardiogenic shock, and infarct related mechanical complications.7 Scientific societies and health authorities need to take strong action to minimize this excess of cardiovascular morbimortality that is expected during the current pandemic. The population needs to be told that seeking medical attention in health centers is safe, that protection against contagion is guaranteed, and that infarction- like symptoms or other serious conditions (strokes, pulmonary embolisms, aorta dissections) require urgent medical attention.
We cannot rule out the possibility that STEMI are being misdiagnosed in patients who go to the hospital seeking medical attention since the healthcare activity displayed these days is focused on the management of patients with COVID-19. Therefore, for staff who are working in the emergency services during this pandemic, The best revascularization option today is still percutaneous coronary intervention that has consistently proven to reduce mortality, reinfarction, stroke, and mechanical complications compared to thrombolysis.7 The ACI-SEC and the Spanish Society of Cardiology Working Group on Cardiac Catheterization and Interventional Cardiology have both proposed an algorithm where percutaneous coronary intervention should be the treatment of choice. Also, patients with anticipated time delays until mechanical reperfusion should be treated with thrombolysis. Patients with COVID-19 who present at the hospital 3 hours before symptom onset who are hemodynamically stable and have no contraindication for thrombolysis should receive thrombolytic treatment.3
Another disturbing piece of information is the reduction in the number of non-emergent diagnostic and interventional procedures not related to STEMI being performed. These procedures will need to be rescheduled after the peak number of patients hospitalized with COVID-19 has been reached. Also, the lack of intensive care unit beds (most filled with patients with COVID-19) can reduce the capacity to perform cardiac surgeries and treat patients with surgical indications. This anticipates more interventional procedures being performed in complex patients who would have required surgical treatment in other circumstances.
Finally, we should mention that up to 5% of interventional cardiologists who participated in the infarction code program have presented COVID-19, in addition to those who remain under confinement or those who are attending COVID-19 patients outside the interventional cardiology units. This scenario is probably applicable to nurses and other healthcare workers at the cathlab. It is essential to protect all healthcare workers with the appropriate personal protection equipment to avoid exposure to COVID-19. Weekly shifts could also be established to reduce the risk of simultaneous contagion of several members of the unit given that these procedures require a very high level of specialization and cannot be performed by other healthcare workers.
Limitations
Although this is a retrospective analysis, the parameters of activity have been well-established in all interventional cardiology units An important limitation is the unavailability of infarction assistance times, patients’ clinical characteristics and in-hospital complications. However, as already mentioned, a study has confirmed that reperfusion times are being delayed significantly.5 Another limitation is that some autonomous communities have had local festivities that may have altered the number of elective procedures performed. Even so, the great reduction of activity seen cannot be attributed to this fact alone since other autonomous communities without any local festivities have also seen their production reduced. Also, STEMI is managed independently regardless of whether there is a local festivity or not. Lastly, there are 8 centers whose activity has not been reported. In Canary Islands there is data for only 50% of centers. Despite the number, the volume of cases reported by those centers is low and only represents less than 5% of all percutaneous coronary interventions performed in the infarction setting.2
Conclusions
This study analyzes the significant reduction of healthcare in interventional cardiology that is being sustained during the current COVID-19 pandemic. Similarly, a great reduction in the number of STEMI patients treated has been observed with the corresponding risk of higher morbimortality. Scientific societies and health authorities need to take strong actionso patients with STEMI-like symptoms can seek medical attention and be properly diagnosed and receive reperfusion treatment.
Conflicts of interest
The authors declared no conflicts of interest whatsoever. R. Moreno is associate editor of Rev Esp Cardiol. The journal's editorial procedure to ensure impartial handling of the manuscript has been followed.
Editor's note
This manuscript has undergone a process of internal review of exceptional priority by the editorial staff due to the special interest of disclosing the information contained herein to the scientific community. The editors wish to thank Permanyer Publications for its collaboration and commitment for the quick publication of this document.
What is known about the topic?
- Percutaneous coronary intervention is the treatment of choice for patients with STEMI. A recent study conducted in Hong Kong, China during the current COVID-19 pandemic showed it takes longer than usual for patients with infarction to seek medical attention after symptom onset. There is no information available on the number of patients treated during the pandemic compared to the number treated in normal conditions.
What does this study add?
- The COVID-19 pandemic has significantly reduced the number of STEMI patients treated. Also, a significant reduction of elective coronary and structural procedures has been confirmed. This dramatic reduction in the performance of elective procedures may have an impact on future organization and care. Finally, yet despite how serious the current situation is, infarction code systems are still working adequately.
Annex 1
Participant centers and researcher in charge in each particular center
| Andalusia | |
|---|---|
| Hospital Universitario Virgen del Rocío | Manuel Villa |
| Hospital Universitario Virgen Macarena | Rafael Ruiz |
| Hospital Universitario Regional de Málaga | Carlos Sánchez |
| Hospital Universitario Virgen de la Victoria | Antonio Jesús Muñoz |
| Hospital Costa del Sol | Luís Iñigo |
| Hospital Universitario de Jaén | Juan Herrador |
| Hospital Universitario Juan Ramón Jiménez | Antonio Gómez |
| Hospital Universitario Virgen de las Nieves | Eduardo Molina |
| Hospital Universitario San Cecilio | Juan Caballero |
| Hospital Universitario Reina Sofía | Soledad Ojeda |
| Hospital Punta de Europa | Mérida Cárdenas |
| Hospital Universitario Puerta del Mar | Livia Gheorghe |
| Hospital Universitario de Jerez de la Frontera | Jesús Oneto |
| Hospital Universitario Torrecárdenas | Félix Valencia |
| Aragon | |
| Hospital Clínico Universitario Lozano Blesa | José Ramón Ruiz |
| Hospital Universitario Miguel Servet | Juan Sánchez Rubio |
| Principality of Asturias | |
| Hospital Universitario Central de Asturias | Pablo Avanzas |
| Hospital de Cabueñes | Juan Rondan |
| Balearic Islands | |
| Hospital Universitari Son Espases | Vicente Peral |
| Policlínica Nuestra Señora del Rosario | Lucía Vera |
| Canary Islands | |
| Hospital Universitario de Canarias | Francisco Bosa |
| Hospital Universitario Ntra. Sra. de Candelaria | Julio Hernández |
| Cantabria | |
| Hospital Universitario Marqués de Valdecilla | José María de la Torre Hernández |
| Castille-La Mancha | |
| Complejo Hospitalario de Toledo | José Moreu |
| Hospital General de Ciudad Real | Fernando Lozano |
| Hospital General Universitario de Albacete | Jesús Jiménez |
| Hospital Universitario de Guadalajara | Enrique Novo |
| Castille and León | |
| Hospital de León | Armando Pérez de Prado |
| Hospital Clínico Universitario de Valladolid | Ignacio Amat |
| Hospital Universitario de Salamanca | Ignacio Cruz |
| Catalonia | |
| Hospital Universitari Bellvitge | Joan Antoni Gómez |
| Hospital de la Santa Creu i Sant Pau | Joan García Picart |
| Hospital Universitario Vall d’Hebrón | Bruno García |
| Hospital Clínic de Barcelona | Salvatore Brugaletta |
| Hospital Universitari Germans Trias i Pujol | Oriol Rodríguez |
| Hospital del Mar | Neus Salvatella |
| Hospital Universitari Joan XXIII | Mohsen Mohandes |
| Hospital Universitari de Girona Dr. Josep Trueta | Xavier Oliva |
| Hospital Universitari Arnau de Vilanova | Joan Casanova |
| Hospital Universitari Mútua de Terrassa | Juan Francisco Muñoz |
| Community of Madrid | |
| Hospital Universitario Fundación Jiménez Díaz | Juan Franco |
| Hospital Clínico San Carlos | Pablo Salinas |
| Hospital General Universitario Gregorio Marañón | Jaime Elízaga |
| Hospital Universitario 12 de Octubre | Fernando Sarnago |
| Hospital Universitario La Paz | Santiago Jiménez |
| Hospital Universitario de La Princesa | Fernando Rivero |
| Hospital Universitario Puerta de Hierro Majadahonda | Juan Francisco Oteo |
| Hospital Ramón y Cajal | Rosana Hernández Antolín |
| Chartered Community of Navarre | |
| Complejo Hospitalario de Navarra | Valeriano Ruiz |
| Region of Murcia | |
| Hospital Clínico Universitario Virgen de la Arrixaca | Eduardo Pinar |
| Hospital de Santa Lucía de Cartagena | Luciano Consuegra |
| Valencian Community | |
| Hospital General Universitario de Castellón | Ana Planas |
| Hospital Universitario y Politécnico La Fe | José Luís Díez |
| Hospital General Universitario | Alberto Berenguer |
| Hospital Clínico Universitario | Agustín Fernández Cisnal |
| Hospital Universitario Dr. Peset | Pablo Aguar |
| Hospital Universitario de la Ribera | Francisco Pomar |
| Hospital de Manises | Miguel Jerez |
| Hospitales de Torrevieja-Elche-Vinalopó | Francisco Torres |
| Hospital General Universitario San Juan de Alicante | Pilar Carrillo |
| Hospital General Universitario de Alicante | Juan Miguel Ruiz Nodar |
| Basque Country | |
| Hospital Donosti | Miren Tellería |
| Hospital Universitario de Cruces | Koldobika García |
| Hospital de Basurto | Abel Andrés |
| Hospital Galdakao-Usansolo | Mario Sadaba |
| Extremadura | |
| Complejo Hospitalario Universitario de Badajoz | José Ramón López |
| Complejo Hospitalario de Cáceres | Javier Fernández Portales |
| Hospital de Mérida | Juan Carlos Merchán |
| Galicia | |
| Complejo Hospitalario Universitario A Coruña | Guillermo Aldama |
| Complexo Hospitalario Universitario de Vigo | Saleta Fernández |
| Hospital Universitario Lucus Augusti | Melisa Santás |
| Hospital Clínico Universitario Santiago de Compostela | Ramiro Trillo |
| La Rioja | |
| Hospital San Pedro | Pilar Portero |
REFERENCES
1. Boletín Oficial del Estado núm. 67, de 14 de marzo de 2020, páginas 25390-25400. Sección I. Disposiciones generales. Available online:https://www.boe.es/eli/es/rd/2020/03/14/463. Accessed 29 Mar 2020.
2. Cid-Álvarez B, Rodríguez-Leor O, Moreno R, Pérez de Prado A. Spanish Cardiac Catheterization and Coronary Intervention Registry. 28th Official Report of the Spanish Society of Cardiology Working Group on Cardiac Catheterization and Interventional Cardiology (1990-2018). Rev Esp Cardiol.2019;72:1043-4053.
3. Romaguera R, et al. Considerations on the invasive management of ischemic and structural heart disease during the COVID-19 coronavirus outbreak. Consensus statement of the Interventional Cardiology Association and the Ischemic Heart Disease and Acute Cardiac Care Association of the Spanish society of Cardiology. REC Interv Cardiol. 2020. https://doi.org/10.24875/RECICE.M20000121.
4. Romaguera R, et al. Consensus document of the Interventional Cardiology and Heart Rhythm Associations of the Spanish Society of Cardiology on the management of invasive cardiac procedure rooms during the COVID-19 coronavirus outbreak. REC Interv Cardiol. 2020. https://doi.org/10.24875/RECICE.M20000116..
5. Tam CF, Cheung KS, Lam S, et al. Impact of coronarvirus disease 2019 (COVID-19) outbreak on ST-segment elevation myocardial infarction care in Hong-Kong, China. Cardiovasc Qual Outcomes. 2020. https://doi.org/10.1161/CIRCOUTCOMES.120.006631.
6. Larsen JM, Ravkilde J. Acute coronary angiography in patients resuscitated from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2012;83:1427–1433.
7. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177.
Correspondance author: Institut del Cor, Hospital Germans Trias i Pujol, Carretera de Canyet s/n, 08916 Badalona, Barcelona, Spain.
E-mail address: oriolrodriguez@gmail.com (O. Rodríguez-Leor).