HOW WOULD I APPROACH IT?
This is the case of a 57-year-old man with a past medical history of ischemic heart disease treated percutaneously years ago who was admitted with signs of non-ST-elevation acute coronary syndrome and inferior wall hypokinesis on the echocardiogram. The coronary angiography performed 24 hours after admission revealed the presence of restenosis in a stent implanted into the mid left anterior descending coronary artery and severe stenosis of distal right coronary artery. The angiographic imaging suggested the presence of 1 intraluminal thrombus spreading towards the ostium of the posterior descending coronary artery. The right coronary artery underwent immediate percutaneous treatment with balloon predilatation, which immediately triggered the appearance of the no-reflow phenomenon (NRP).
NRP is defined as a reduced coronary flow after the angioplasty for the lack of a mechanical obstruction of the epicardial coronary artery. Although its incidence rate has somehow dropped over the last few years with the use of more powerful antiplatelet drugs and early approach of coronary syndromes, the therapeutic management of this entity is still challenging for the lack of standard therapies. From the pathophysiological point of view, the NRP has been associated with an occlusion of coronary microcirculation of multifactorial origin including microembolization, microcirculation vasospasm, and edema or myocardial bleeding in the necrosis setting. These mechanisms would activate the inflammatory cascade and promote the release of free radicals and eventually platelet therapy.
Former clinical trials have assessed different strategies to prevent this phenomenon from happening using thrombus aspiration prior to angioplasty (TASTE and TOTAL clinical trials) or through the intracoronary administration of abciximab (INFUSE-AMI). However, none of them has been able to prove definitive clinical benefits. Similarly, there are contradictory data on the use of vasodilators like adenosine, verapamil or intracoronary nitroprusside to prevent and treat NRP. Regarding established NRP, only 1 clinical trial recently published (the COAR) has proven the superiority of intracoronary adrenaline compared to adenosine in patients with loss of distal flow after coronary stenting.1
Going back to our case , initially, it would be good to complete the study using an intracoronary imaging modality to discard other possible causes of loss of distal flow like dissection or coronary spasm. Once the presence of thrombus has been confirmed, flow recovery is essential before considering stenting. In this context, my initial strategy would be to repeat aspirations using manual thrombectomy devices towards the posterior descending coronary artery and eventually the posterolateral one even accessing the femoral artery differently if needed to advance higher profile extractors (7-Fr) with greater aspiration capabilities. In the presence of persistent NRP the local administration of vasodilators could be considered (table 1 shows drugs validated in former studies and their corresponding doses). In the presence of hypotension and bradycardia the intracoronary infusion of adrenaline may be advised through coaxial microcatheters advanced into the occlusion region or through dedicated catheters with distal infusion holes to keep advancing the guidewire through the vessel during drug infusion (figure 1). In the presence of an aspiration-resistant thrombus, I would choose the intracoronary administration of anti-IIb/IIIa agents or fibrinolytic drugs (by administering a third of the systemic dose) using dedicated catheters.2 Eventually, I would use the marinade technique3 with vessel distal occlusion and inflate a balloon at posterior descending coronary artery level while administering the fibrinolytic drug through the guide catheter extension system advanced through the middle-distal right coronary artery (figure 2). Finally, if the above measures don’t work, I would treat the restenosis of the mid left anterior descending coronary artery in the same surgical act to reduce myocardial ischemia in other territories.
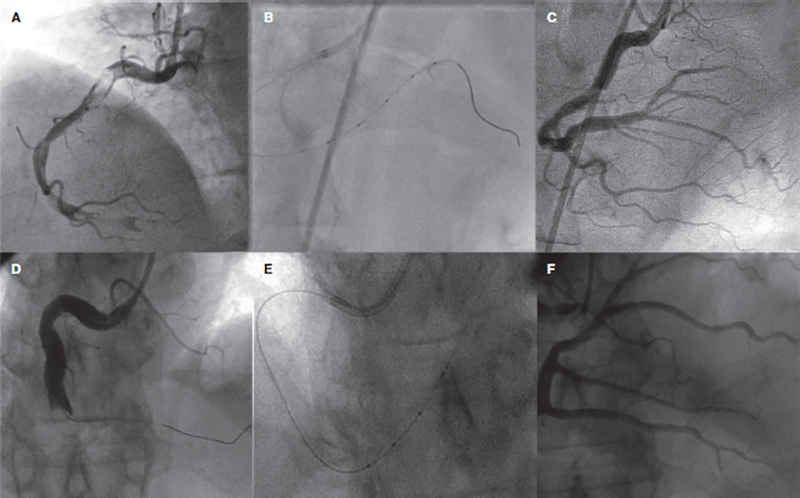
Figure 1. Use of catheter with distal infusion holes for direct administration of intracoronary thrombolytic drug in 2 patients with high thrombotic burden and lack of distal flow after repeated thrombus aspiration. A and D: early right coronary angiography. B and E: image of the catheter into the distal right coronary artery. C and F: final angiographic outcomes.
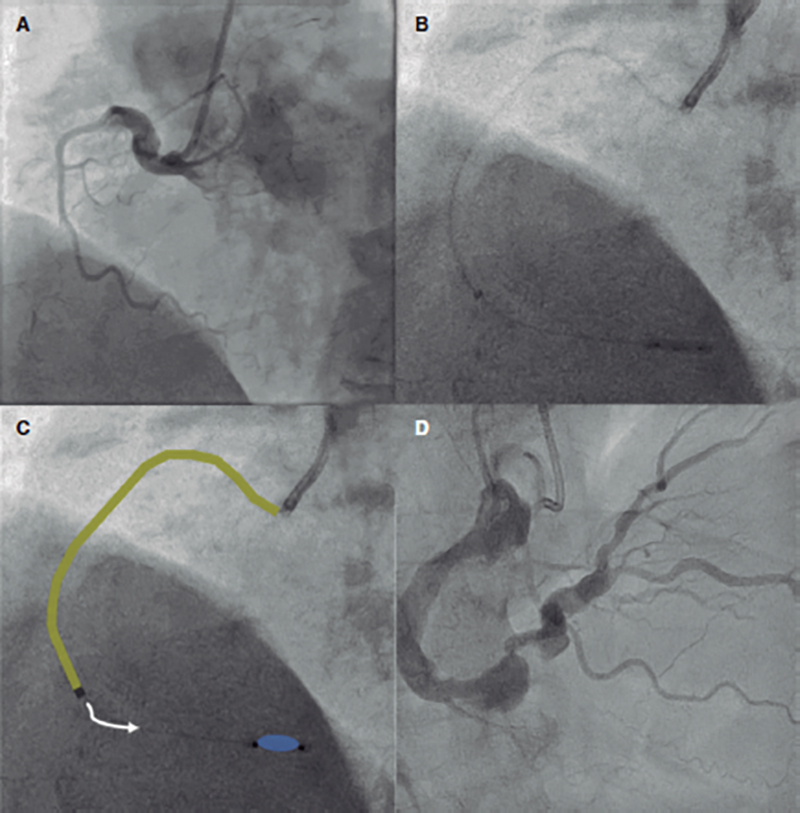
Figure 2. Administration of intracoronary fibrinolytic therapy with distal occlusion (the “marinade” technique). A: early angiographic imaging with right coronary occlusion at first curve level. B and C: infusion of 2000 IU of alteplase through a guide catheter extension system (in yellow) while keeping distal balloon inflation for 5 minutes. D: final angiographic outcomes.
Table 1. Drugs used to treat no-reflow phenomenon (dose of intracoronary bolus, and maximum dose described)
| Drug | Dose of intracoronary bolus | Maximum dose |
|---|---|---|
| Vasodilators | ||
| Adenosine | 100 μg | 2000 μg |
| Nitroprusside | 50 μg | 300 μg |
| Nicardipine | 50μg | 400 μg |
| Verapamil | 0.5 μg | 1 mg |
| Nicorandil | 0.5 μg | 4 mg |
| Nicardipine | 100 μg | 2200 μg |
| Dipyridamole | 0.56 mg/kg | 200 mg |
| Anti-IIb/IIIa | ||
| Abciximab | 0.25 mg/kg | IV infusion of 0.125 μg/kg/min |
| Eptifibatide | 180 μg | IV infusion of 2 μg/kg/min |
| Other drugs | ||
| Adrenaline | 100 μg | 400 μg |
| Cyclosporine A | IV 2.5 mg/kg | – |
After finishing the procedure and in the presence of persistent NRP, I would consider using percutaneous circulatory assist devices to improve myocardial diastolic flow.
Some authors have described the use of non-pharmacological therapies to treat NRP like induced hypothermia or the intracoronary high-pressure injection of autologous blood. However, the effectiveness of these strategies is still to be determined. Similarly, multiple studies have been published on the use of different agents both vasodilators (papaverine) and anti-free radical drugs (anisodamine), and growth factors in this context. However, their availability is limited, and their efficacy has not been demonstrated in randomized clinical trials.
Given the multifactorial nature of NRP, the combination of different strategies can be advised considering techniques to eliminate the thrombotic burden (repeat aspiration or local administration of antithrombotic drugs) in cases with predominant distal embolization. Also, the local administration of vasodilators is advised to treat patients with suspected microcirculation disorders.
FUNDING
None whatsoever.
CONFLICTS OF INTEREST
None reported.
REFERENCES
1. Khan KA, Qamar N, Saghir T, et al. Comparison of Intracoronary Epinephrine and Adenosine for No-Reflow in Normotensive Patients With Acute Coronary Syndrome (COAR Trial). Circ Cardiovasc Interv. 2022;15:e011408.
2. Unzue L, Garcia E, Teijeiro R, et al. Local intracoronary fibrinolysis in acute mycardial infarction of ectatic coronary arteries in the post-abiximab era. Cardiovasc Revasc Med. 2021;32:69-74.
3. Unzue L, García E, Teijeiro-Mestre R. Local fibrinolysis with distal occlusion: “marinade” technique. Rev Esp Cardiol. 2022;75:86.

