To the Editor,
Drug-coated balloons (DCB) have emerged as a promising strategy to treat coronary bifurcation lesions. Although the results of published studies are favorable, a significant clinical benefit has not yet been demonstrated, unlike the angiographic benefit already reported due to the phenomenon of positive remodeling. However, knowledge is scarce on the prognostic factors that may influence outcomes after DCB for treating side branches and the subgroups of patients who might derive the greatest benefit.
We present the results of a registry of all coronary bifurcation lesions treated at our center with the SeQuent Please Neo DCB (BBraun, Germany) from November 2018 through February 2024. The inclusion and exclusion criteria, and lesion management strategy have been extensively described in a previous publication.1 Various clinical, anatomical, and procedural variables were analyzed. Rates of target lesion revascularization (TLR) and major adverse cardiovascular events (MACE) were recorded during clinical follow-up, which extended up to a maximum of 2 years. All patients provided informed consent, and the study was approved by the ethics committee.
A total of 144 patients with 146 lesions were included. The characteristics of the sample and rate of adverse events (mean follow-up, 439 ± 272 days; range, 9-730 days) are shown in Table 1. All cases of TLR occurred in symptomatic patients.
Table 1. Sample characteristics and rate of adverse events
| Clinical characteristics (n = 144) | ||
|---|---|---|
| Age | 65.8 ± 11.1 years (range, 38-91) | |
| Male sex | 79.9 (115) | |
| Hypertension | 64.6 (93) | |
| Dyslipidemia | 81.9 (118) | |
| Smoking | 27.8 (40) | |
| Diabetes | 33.3 (48) | |
| Previous PTA | 45.8 (66) | |
| Indication for coronary angiography | ||
| NSTEACS | 36.8 (53) | |
| STEACS | 15.3 (22) | |
| Stable angina | 31.3 (45) | |
| Ventricular dysfunction | 6.9 (10) | |
| Other | 9.7 (14) | |
| Anatomic and procedural characteristics (n = 146) | ||
| Damaged vessel | ||
| LMCA-LCx | 11.6 (17) | |
| LAD-Diagonal | 52.1 (76) | |
| LCx-OM | 23.3 (34) | |
| PDA-PLA | 13 (19) | |
| ISR-type of lesion | 20.5 (30) | |
| Medina classification | ||
| 1-1-1 | 41.1 (60) | |
| 1-1-0 | 20.5 (30) | |
| 1-0-0 | 6.8 (10) | |
| 0-0-1 | 11 (16) | |
| 1-0-1 | 2.7 (4) | |
| 0-1-1 | 9.6 (14) | |
| 0-1-0 | 8.2 (12) | |
| Length of side branch lesion | ||
| Without lesion | 33.6 (49) | |
| Short lesion < 10 mm | 45.2 (66) | |
| Long lesion > 10 mm | 21.2 (31) | Anatomical and procedural characteristics (n = 146) |
| Radial access | 95.9 (140) | |
| 96.6 (141) | ||
| Predilatataion | 92.5 (135) | |
| Side branch | 92.5 (135) | |
| Main branch | 71.2 (104) | |
| Treatment of main branch | ||
| Stent | 82.2 (120) | |
| DCB | 7.5 (11) | |
| Application of DCB pre-stenting in the main branch | 4.8 (7) | |
| Diameter of DCB for the side branch | ||
| < 2.5 mm | 34.2 (50) | |
| ≥ 2.5 mm | 65.8 (96) | |
| Postdilatation | ||
| Main branch | 69.2 (101) | |
| POT technique | 41.1 (60) | |
| Side branch | 24 (35) | |
| Kissing-balloon | 38.4 (56) | |
| OCT-IVUS | 11 (16) | |
| Rate of adverse events | ||
| Target lesion revascularization | 4.1 (6) | |
| Target lesion thrombosis | 1.4 (2) | |
| Probable | 0.7 (1) | |
| Definitive | 0.7 (1) | |
| Death | 6.3 (9) | |
| Cardiac cause | 1.4 (2) | |
| Noncardiac cause | 4.9 (7) | |
| MACE | 5.5 (8) | |
DCB, drug-coated balloon; ISR, in-stent restenosis; IVUS, intravascular ultrasound; LAD, left anterior descending; LCx, left circumflex artery; LMCA, left main coronary artery; MACE, major adverse cardiovascular events; NSTEACS, non-ST-segment elevation acute coronary syndrome; OCT, optical coherence tomography; OM, obtuse marginal; PCI, percutaneous coronary intervention; PDA, posterior descending artery; PLA, posterolateral artery; POT, proximal optimization technique; PTA, percutaneous transluminal angioplasty; STEACS, ST-segment elevation acute coronary syndrome; TLR, target lesion revascularization. Values are expressed in percentages and absolute number of cases (in brackets). | ||
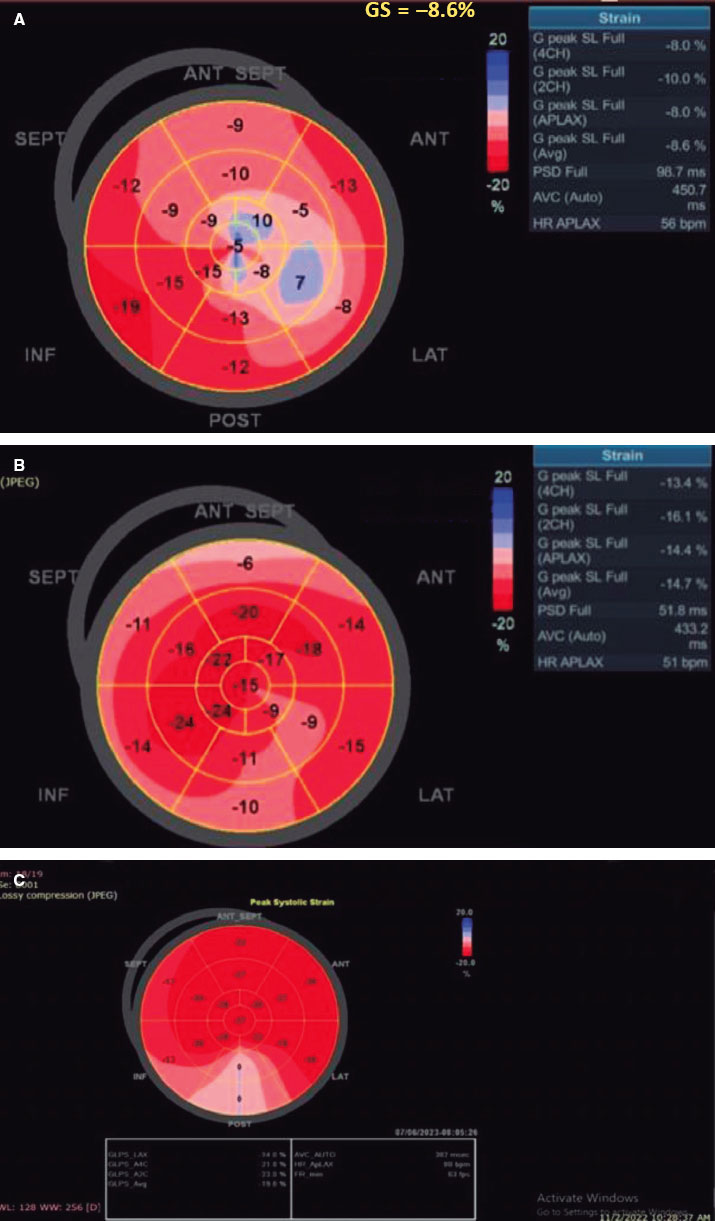
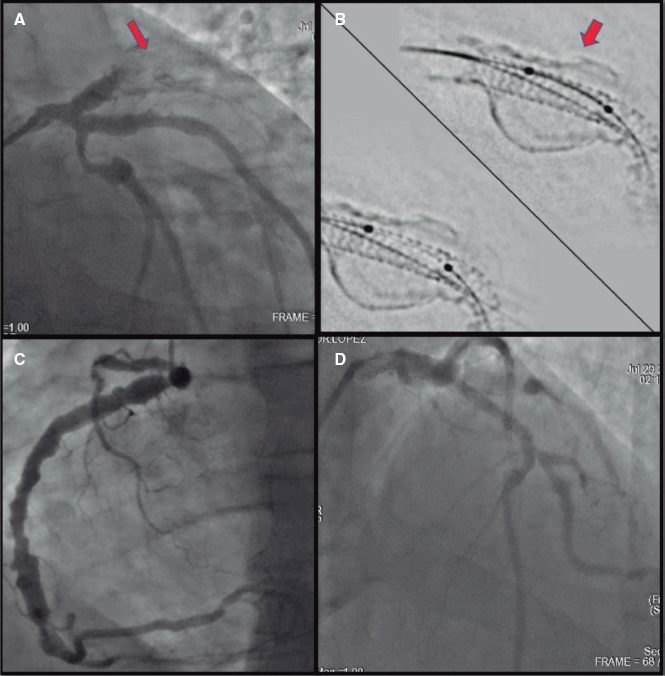
On univariate analysis, among clinical factors, previous revascularization with stents was associated with the occurrence of both TLR and MACE (P < .01), while age was associated with a greater need for TLR (73.5% vs 63.5%; P = .03). Among anatomical factors, lesion location showed a statistically significant associated with both study endpoints (TLR, P < .01 and MACE, P = .04); left main coronary artery bifurcation was associated with the worst outcomes, with a greater need for TLR (P = .016) reported in 17.6% of cases, and a higher rate of MACE (P = .039). For procedural factors, main branch postdilatation was associated with a lower rate of adverse events (25% vs 71.7%; P = .01), approaching significance in the case of new TLR (33.3% vs 70.7%; P = .07). The presence of a long lesion (> 10 mm) in the side branch was associated with a worse outcome, with a higher rate of TLR (66.7% vs 19.3%; P = .03) and MACE (50% vs 21.2%; P = .05). Figure 1 shows the TLR-free survival curves in relation to the length of the side branch lesion.
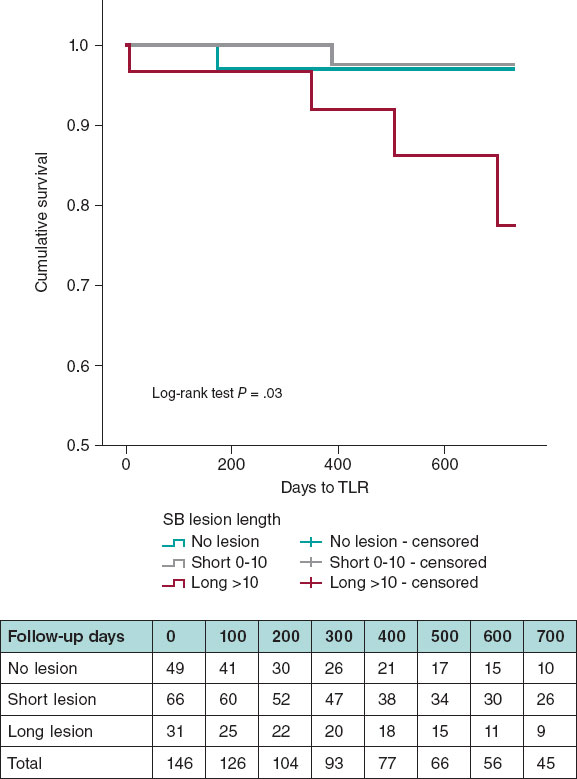
Figure 1. Target lesion revascularization-free survival curves based on the length of the side branch lesion. SB, side branch; TLR, target lesion revascularization.
On multivariate analysis using Cox regression (including factors with P values < .15 from the univariate analysis), the only independent predictor of TLR was the absence of a long lesion in the side branch (P = .034; 95% confidence interval [95%CI], 0.012-0.84), with borderline significance for MACE (P = .062; 95%CI, 0.46-1.08).
Few studies have analyzed the influence of different factors on the clinical outcomes of this type of lesion. Among the factors classically established as unfavorable, in-stent restenosis (ISR) is notable. The main study to date on ISR-type lesions within a bifurcation was conducted by Harada et al.2 in 2017, in which the rate of TLR reached 22%, much higher than the average TLR rate found in other types of lesions (5%-12%). Regarding the specific location of ISR in the left main coronary artery bifurcation, a study3 identified the presence of the lesion in a true bifurcation as the only independent predictor of MACE (hazard ratio, 4.62; 95%CI, 1.57-13.5; P < .01), although it did not specify the length of the side branch lesion.
In a study by Bruch et al.4 conducted in a registry of 130 lesions treated with DCB, the only predictor of MACE was the degree of pre-existing stenosis in the main branch. In another very recent study by a Japanese group5 that analyzed the results of 1751 de novo coronary artery lesions with unfavorable profiles (including bifurcations in 12% of the sample) treated with DCB, and an overall TLR rate of 9%, the only independent predictors of higher risk were hemodialysis and active smoking.
One of the factors associated with worse prognosis in the present study was the location of the lesion at a bifurcation in the left main circumflex artery. Although this did not remain an adverse prognostic factor in the multivariate analysis, the low rate (only 11%) of intracoronary imaging modalities performed in our patients could have improved results in this subgroup. Previous studies have demonstrated the benefit of these imaging modalities in the specific scenario of unprotected left main interventions.
The only independent predictor of an increased incidence of adverse events found in our study was the presence of a lesion > 10 mm in the side branch. This length was previously indicated as an unfavorable factor in the study by Zimarino et al.,6 which showed a 2-fold higher rate of MACE in the subgroup of patients with side branch lesions > 10 mm. In the registry by Bruch et al.,4 this factor did not appear as an unfavorable predictor, and the mean lesion length in the side branch was 11.8 ± 4.5 mm. Notable, there was no occurrence of TLR in lesions affecting the anterior descending-diagonal bifurcation, confirming the high effectiveness of DCB in this location.
The main limitation of this study is the absence of a control group and a systematic angiographic review, which could have identified any cases of device failure that went clinically silent. In addition, there was a relatively high inclusion rate of small side branch lesions (< 2.5 mm), accounting for 34% of the sample, which could be a relevant factor in potentially underestimating TLR failure. However, one-third of patients requiring TLR had side branch sizes < 2.5 mm.
Paclitaxel-coated balloons are effective in treating side branches in bifurcation lesions, with a low rate of adverse events in long-term follow-up. Although several factors are associated with a worse prognosis, only a long length of the side branch seems to be an independent predictor of the need for TLR.
Randomized clinical trials are needed to draw definitive conclusions on the utility of DCB to treat side branches in coronary bifurcation lesions.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
Prior written informed consent was obtained from all participants, and the study was approved by the ethics committee. Potential gender biases have been considered.
STATEMENT on the use of artificial intelligence
None used.
AUTHORS’ CONTRIBUTIONS
J. Valencia performed the statistical analyses and drafted the manuscript. The remaining authors participated in the procedures and reviewed the article.
CONFLICTS OF INTEREST
None declared.
REFERENCES
1. Valencia J, Torres-Mezcua F, Herrero-Brocal M, et al. Long-term effectiveness of drug-coated balloon in the side branch treatment of bifurcation lesions. REC Interv Cardiol. 2023;5:7-13.
2. Harada Y, Colleran R, Pinieck S, et al. Angiographic and clinical outcomes of patients treated with drug-coated balloon angioplasty for in-stent restenosis after coronary bifurcation stenting with a two-stent technique. Eurointervention. 2017;12:2132-2139.
3. Kook H, Joo HJ, Park JH, Hong SJ, Yu CW, Lim D. A comparison between drug-eluting stent implantation and drug-coated balloon angioplasty in patients with left main bifurcation in-stent restenotic lesions. BMC Cardiovasc Disord. 2020;20:83.
4. Bruch L, Zadura M, Waliszewski M, et al. Results from the international Drug coated balloon registry for the treatment of bifurcations. Can a bifurcation be treated without stents?J Interven Cardiol. 2016;29:348-356.
5. Funatsu A, Sato T, Koike J, Mizobuchi M, Kobayashi T, Nakamura S. Comprehensive clinical outcomes of drug-coated balloon treatment for coronary artery disease. Insights from a single-center experience. Catheter Cardiovasc Interv. 2024;103:404-416.
6. Zimarino M, Barabto E, Nakamura S, et al. The impact of the extent of side branch disease on outcomes following bifurcation stenting. Catheter Cardiovasc Interv. 2020;96:E84-E92.
* Corresponding author.
E-mail address: jvalenciam@hotmail.com (J. Valencia).