ABSTRACT
During March 2020, the SARS-CoV-2 virus spread throughout Europe, with the spread being especially intense in Italy and Spain. Given the emergency created by the COVID-19 outbreak, routine activity has been altered in most cardiac catheterization and electrophysiology labs. Health staff working in these areas are faced with performing procedures in patients with a confirmed diagnosis of COVID-19 or with uncertainty in unconfirmed cases. This article is a consensus document of the Interventional Cardiology Association and Heart Rhythm Association of the Spanish Society of Cardiology and aims to provide information to health care professionals working in these invasive cardiology facilities (cardiac catheterization and electrophysiology labs, pacemaker implantation) in order to guarantee quality patient care and adequate levels of infection prevention.
Keywords: Interventional cardiology. Electrophysiology. Infection. Prevention. Prevention. COVID-19. Coronavirus. Pandemic.
RESUMEN
Durante marzo de 2020, el virus SARS-CoV-2 se ha extendido por toda Europa, con especial intensidad en Italia y España. Ante la emergencia creada por el brote de COVID-19, la inmensa mayoría de las salas de hemodinámica y electrofisiología han visto alterada su actividad habitual. Además se enfrentan a la realización de procedimientos en pacientes con diagnóstico confirmado de COVID-19 o con la incertidumbre en casos no confirmados. El presente texto es un documento de consenso de la Asociación de Cardiología Intervencionista y la Asociación del Ritmo Cardiaco de la Sociedad Española de Cardiología que pretende dar información al personal sanitario de estas instalaciones de cardiología invasiva (hemodinámica y electrofisiología y marcapasos) para garantizar una atención de calidad a los pacientes así como unos niveles los niveles adecuados de prevención de la infección.
Palabras clave: Cardiología intervencionista. Electrofisiología. Infección. Prevención. COVID-19. Coronavirus. Pandemia.
INTRODUCTION
On 31 December 2019, the authorities of the People’s Republic of China informed the World Health Organization of several cases of pneumonia of unknown cause in Wuhan, a city located in the Chinese province of Hubei. One week later, they confirmed that the cases were due to a new coronavirus, named SARS-CoV-2. During February, the virus spread through northern Italy and subsequently throughout the rest of Europe, including Spain, where measures to contain the spread were initiated on 10 March, 2020. On 13 March, 2020, the Spanish Government issued a decree (article 116.2 of the Spanish Constitution) declaring a state of alarm with immediate effect. The decree involves changes to the organization of health care installations, staff, and services. In line with the new legal situation, the respective health departments of the autonomous communities modified the regulations generally affecting the availability of health staff (eg, working hours, granting of leave, holidays or days off, exemptions), clinical care, and procedures, often restricting activity to emergency care. The Interventional Cardiology Association and the Heart Rhythm Association of the Spanish Society of Cardiology understand the need to make our commitment public and to adapt our practice to the best practices in the current regulatory context.
Like other viruses in the coronavirus family, this pathogen causes various clinical manifestations encompassed within the term COVID-19, which include respiratory illness ranging from the common cold to severe pneumonia with respiratory distress syndrome, septic shock, and multiorgan failure.1 Moreover, prognosis is poor in patients with prior cardiovascular disease and COVID-19 infection.2 Most cases of COVID-19 notified to data have been mild, but the virus is highly contagious, mandating measures to be taken in all health care and nonhealth care settings.
Faced with the emergency created by the COVID-19 outbreak, the vast majority of cardiac catheterization and electrophysiology labs have experienced changes in their day-to-day running. Health care staff working in these areas are faced with performing procedures in patients with a confirmed diagnosis of COVID-19 and with uncertainty in those with unconfirmed infection. In addition, interventional cardiology units are generally closed units with the same team members working closely together in these areas, representing a risk for health care delivery if quarantines are declared in entire units.
The present article is a consensus document aiming to provide information to health staff in these invasive cardiology installations (cardiac catheterization, electrophysiology, and pacemakers) to guarantee delivery of quality patient care. The document also aims to provide information on how to ensure adequate levels of protection against infection among family members, persons living with infected individuals, workers in health care centers, health care workers attending infected individuals, and the remainder of the population in general.
STAFF MANAGEMENT AND INDICATIONS FOR PROCEDURES
We recommend that each unit take the appropriate measures to separate workers into groups so that possible quarantines can be applied to groups within each unit rather than the unit as a whole.
In elective patients, we recommend considering delaying procedures whenever possible.
APPROACH TO THE PATIENT BEFORE ENTRY TO THE LAB
The following steps are recommended before patients enter cardiac catheterization and electrophysiology labs (figure 1):
- Maximal coordination to minimize pre- and postprocedure waiting times in waiting areas.
- Use of surgical masks in all patients while they wait.
- Questioning of all patients about respiratory symptoms, fever, and close contacts before entry to the lab; we also recommend temperature-taking in all patients.
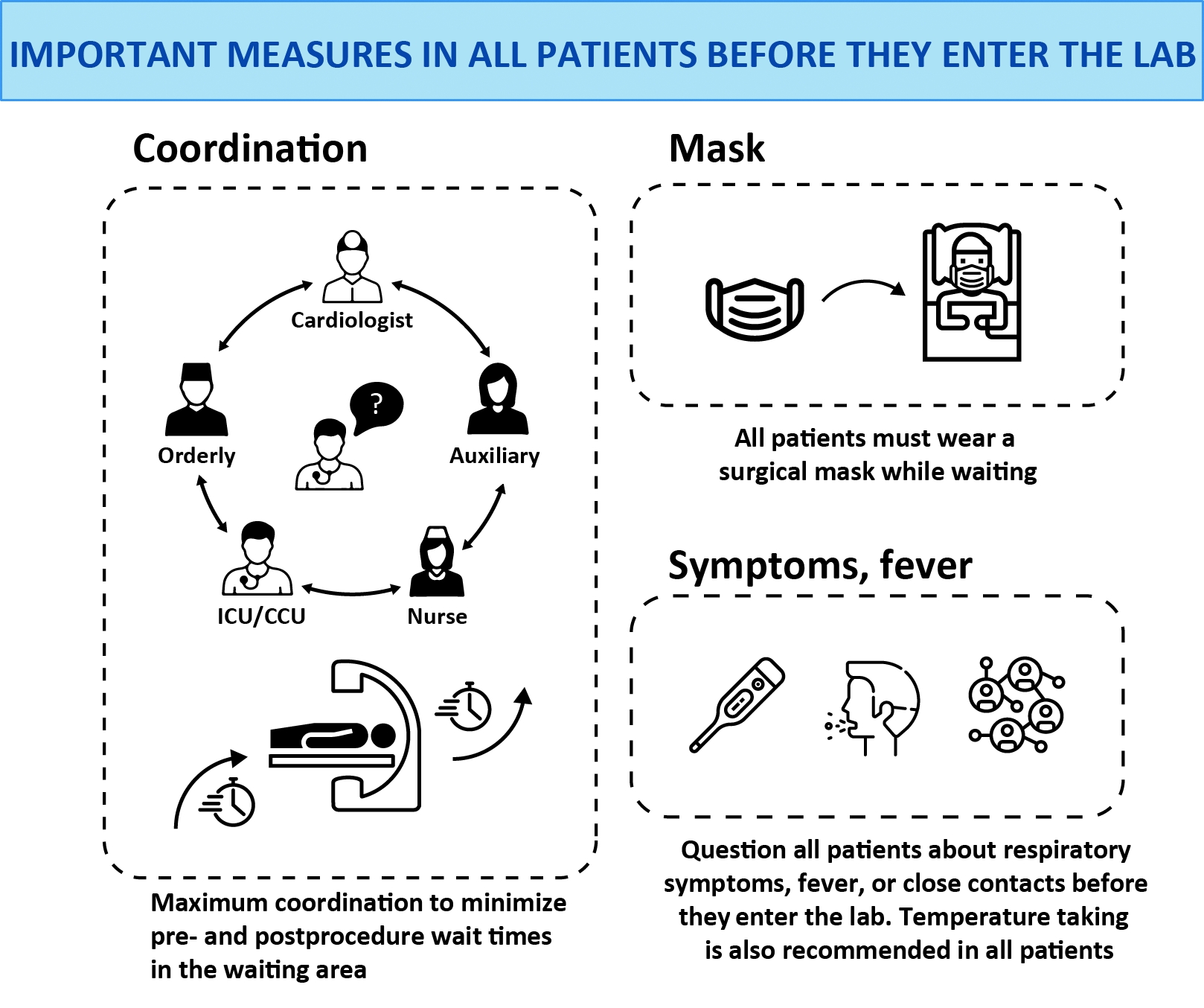
Figure 1. Important measures in all patients before they enter the lab.
CCU, Cardiac/Coronary Care Unit; ICU, Intensive Care Unit.
APPROACH TO PATIENTS WITHOUT CONFIRMATION OF COVID-19 INFECTION
Given the current panorama and the possibility of having to treat asymptomatic patients or those with undiagnosed infection, we recommend taking maximal protection measures,3 especially in patients referred from the emergency department. Procedures involving manipulation of the airway and/or esophagus should also be considered high risk. The following measures are recommended:
- Patients: surgical mask before entry to the lab.
- Physicians and nurses: hand-washing, sterile fluid-impermeable gowns, sterile gloves, splash goggles, cap covering hair, and surgical mask.
- Cardiologists or circulating nurses: splash goggles, gloves, cap, and surgical mask.
In patients with respiratory symptoms in areas of community transmission, those with confirmed contacts and those who may require transesophageal echocardiography, manual ventilation, intubation, or any other type of airway manipulation, we recommend that the approach to infection prevention be the same as that used in patients being tested for COVID-19 infection or with confirmed infection (see next section). The approach to unstable patients, especially those with ST-segment elevation, should also be the same as that in patients with confirmed COVID-19 infection.
APPROACH TO PATIENTS WITH SUSPECTED OR CONFIRMED COVID-19 INFECTION
In patients with suspected or confirmed COVID-19 infection, we recommend the following measures:
- Consider procedures involving airway and/or esophageal manipulation as very high risk.
- Allow only essential staff to enter the lab.
- Keep doors shut at all times.
- Prepare drugs before patient entry to the lab.
- Avoid leaving the lab with contaminated equipment (eg, gown, gloves, mask, etc.) to collect material (eg, stents, catheters, etc) and consequently try to predict the necessary material as much as possible.
Material
The recommended material is shown figure 2 and is described below:
- Patients: surgical mask. It is important to stress that FFP2 masks are personal protection masks and not barrier masks. The air expelled by these masks is contaminated and so they should not be worn by infected patients. Patients should wear a face mask that acts as a barrier to secretions.
- Physicians and nurses: hand-washing, coated fluid-impermeable gown with cuff (if the gown is not fluid-impermeable, a plastic apron should be added), 2 pairs of gloves (whose use is recommended by some local authorities), splash goggles or conventional goggles and face shield, cap, and high filtration efficiency FFP2 mask if available4 (for procedures such as placement of implantable cardioverter-defibrillators, pacemakers and transcatheter prostheses, a surgical mask should be placed over the FFP2 mask). Closed work shoes are recommended or, if unavailable, boots.
- Cardiologists or circulating nurses: gloves, cap, fluid-impermeable gown and FFP2 face mask (if available).
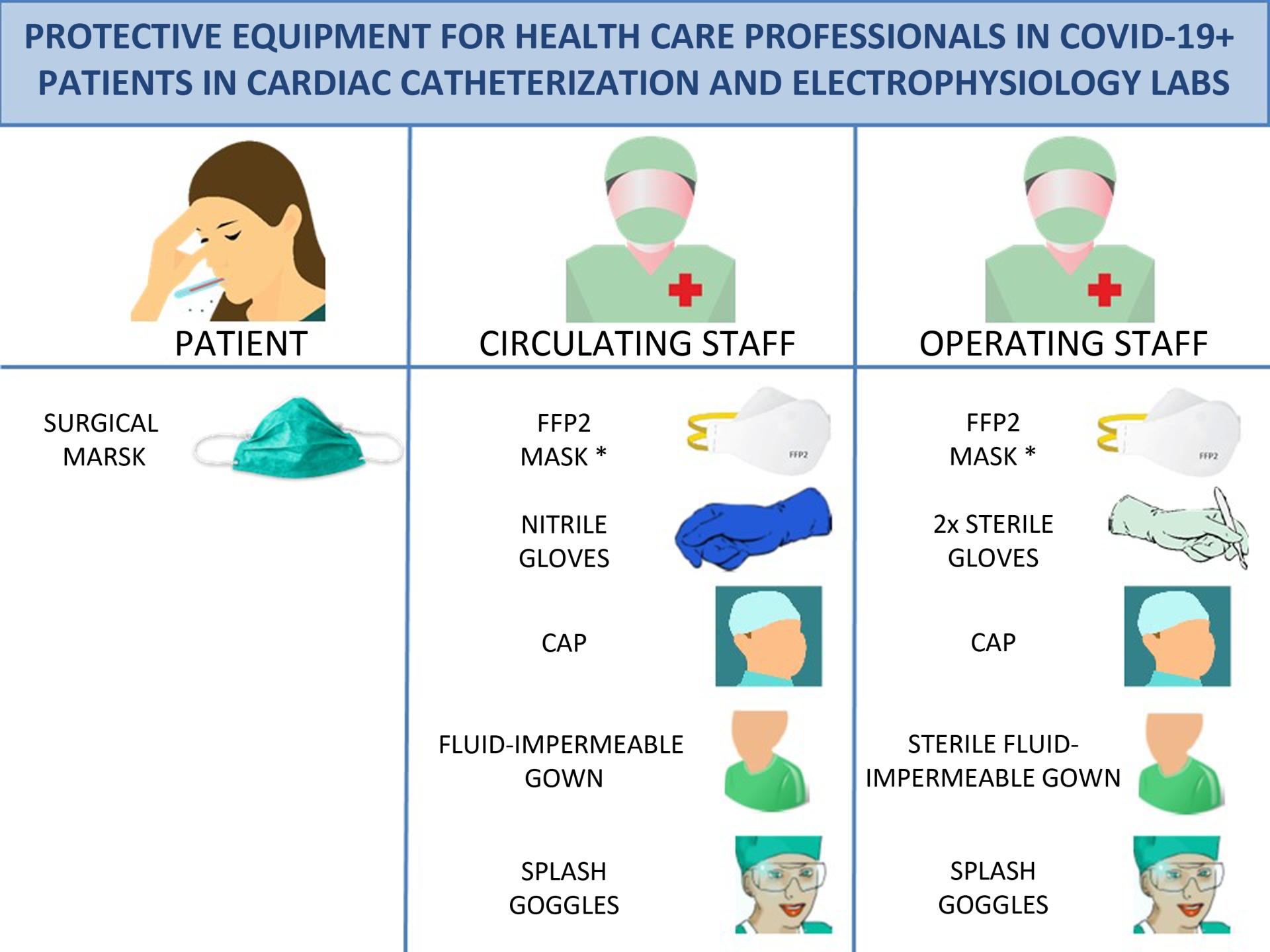
Figure 2. Protective equipment for health care professionals in COVID-19+ patients in cardiac catheterization and electrophysiology labs. * For implantation of pacemaketers, implantable cardioverter-defibrillators and transcatheter prostheses, place a surgical mask over the FFP2 mask. FFP2, filtering face piece type 2.
Recommended steps for moving patients from the gurney to the operating table
Staff responsible for transferring patients with COVID-19 infection from the gurney to the operating table must wear previously placed individual personal protection equipment, including fluid-impermeable gown, cap, cuff-covering gloves, goggles and FFP2 mask (if available). On finishing the transfer, staff must undress as follows, remembering not to remove the mask under any circumstances while inside the lab.
How to dress
The steps for dressing are described below (figure 3).
Outside the lab
- Do not wear jewelry.
- Tie hair back (if necessary).
- Put on lead apron.
- Perform correct hand hygiene using routine method.
- • Place FFP2 mask. The rubber bands should be placed in the following way: the bottom bands in the upper part of the neck and the top bands on the top of the head. Then adjust the height of the mask at the bridge of the nose and cheeks to isolate them and prevent leaks.5
- Place splash goggles.
- Place the cap.
- Perform second hand-washing, with use of alcohol-based hand sanitizer and rubbing.
- Put on the first pair of gloves.
- Put on the gown.
Inside the lab
- Roll the second pair of gloves over your fist.
How to undress
- We recommend that staff undress as shown in figure 3 and described below.
Inside the lab
- As you remove the gown, peel off the outer pair of gloves at the same time6 and discard into a group III container (do not push the gown down into the container to avoid releasing aerosol, which could be contaminated).
Outside the lab
- Remove cap.
- Peel off the second pair of gloves.
- Wash hands.
- Remove splash google with eyes closed.
- Remove the mask by lifting the elastic bands. Under no circumstances touch the front of the mask (which should be assumed to be contaminated).
- Wash hands
If only 1 pair of gloves are worn, first remove them, taking extreme care to avoid contact with the contaminated surface. Then remove the gown by grasping the inside of the gown, taking maximal caution to avoid skin contact with the outer surface.7
Important: Contaminated gowns and gloves (outer ones) should never leave the lab. Staff should never be inside the lab without an FFP2 mask, as a minimum precaution. Masks must always be placed before entering the lab and must not be removed until after staff have left the lab.
After completion of the procedure
After the end of the procedure:
- • We recommend disinfecting goggles with wipes impregnated with a wide spectrum biocidal agent to disinfect surfaces. Leave them wet and air dry. Use gloves to disinfect, due to the toxicity of the wipes and potential contamination of surfaces.
- Discard all material used in the procedure in a group III container for biomedical waste and then seal the container.
- Consider changing scrubs.
- Patients must wear a surgical mask during transfer to the ward or referral center and the orderly or physician (if required) must wear an FFP2 mask.
Lab cleaning
We recommend the following cleaning measures:
- Labs should be cleaned by following specific procedures for contact and drip isolation in each center. For example, by using sodium hypochlorite at a concentration of 1000 parts per million, leaving it in contact with the surface for 5 minutes.
- Cleaning cloths should be discarded (disposable).
- Cleaners should be equipped with personal protection equipment.
- After lab cleaning, consider cleaning all areas where the infected patient has been in contact with an ultraviolet-disinfectant robot.
- Labs should be cleaned at least 1 hour after the procedure, rather than immediately, to allow aerosol deposition.
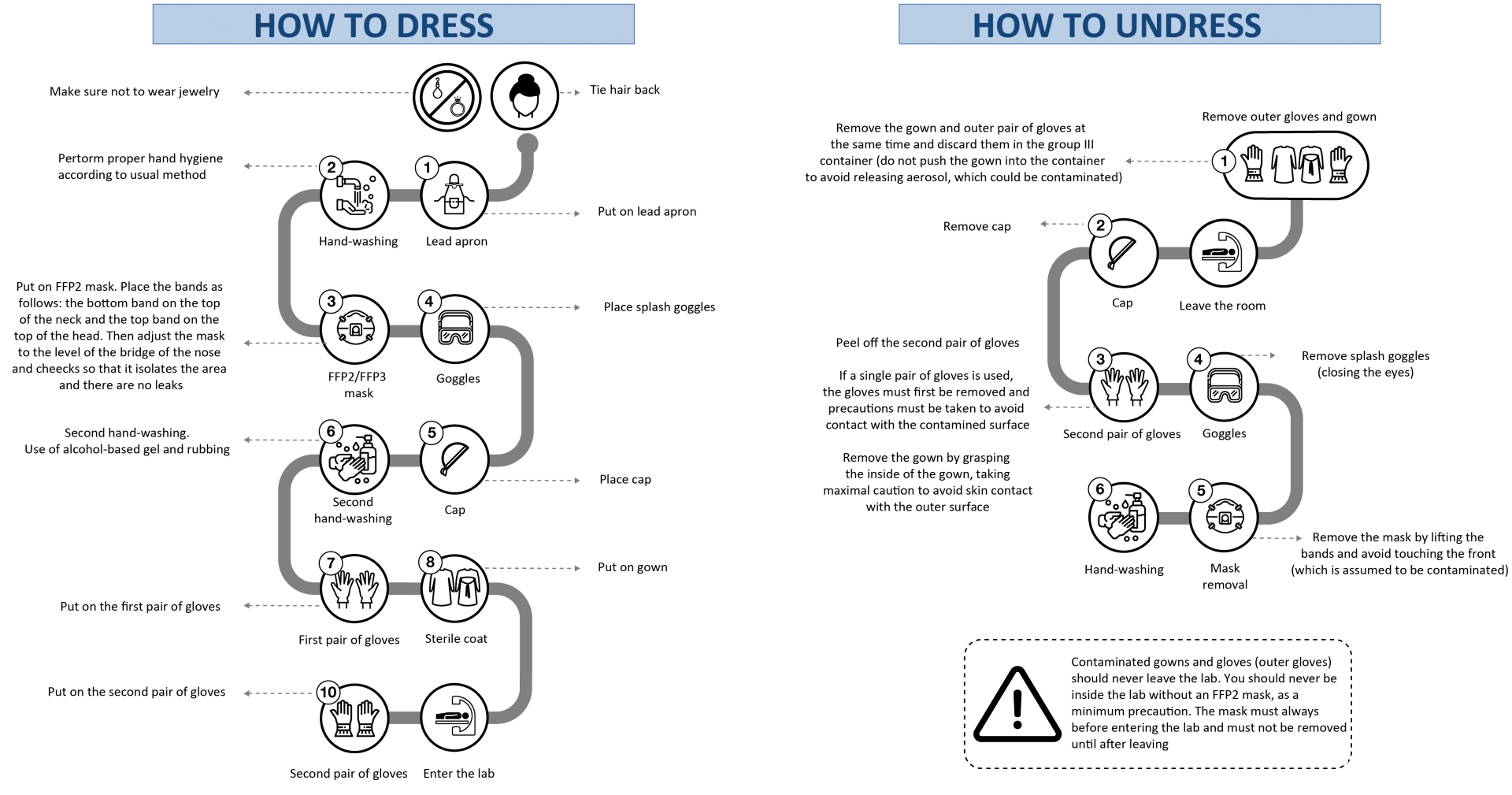
Figure 3. Guidelines on how health staff in cardiac catheterization and electrophysiology labs should dress and undress. FFP, filtering face piece.
SPECIAL SITUATIONS: SEVERELY ILL PATIENTS
If oxygen is required, a mask should be placed over the nasal cannula or oxygen mask.
We discourage the use of nebulizers in patients with COVID-19 and also advise against the use of noninvasive positive pressure ventilation (continuous positive airway pressure [CPAP] and bilevel positive airway pressure [BiPAP]).
In patients requiring intubation and mechanical ventilation or cardiopulmonary resuscitation, extreme care should be taken to apply preventive measures due to the high risk of droplet release.
ROUTINE CARDIOLOGY DRUGS IN PATIENTS WITH COVID-19
Angiotensin converting-enzyme inhibitors/angiotensin II receptor antagonists
There is no evidence to support the hypothesis that these drugs may cause deleterious effects during COVID-19 infection. In contrast, there is much evidence of their cardiovascular benefits in specific populations. Therefore, unless there is a change in current evidence, we advise against their withdrawal unless there is hemodynamic instability.8
Antithrombotic agents
Any inflammatory process increases platelet reactivity. However, there is no current evidence to support any use other than routine use during COVID-19 infection. Therefore, the use of antithrombotic and antiplatelet agents should continue to be considered according to the patient’s clinical situation and bleeding risk.
CONFLICTS OF INTEREST
None declared.
ACKNOWLEDGMENTS
The authors thank Agustín Fernández Cisnal (Hospital Clínico de Valencia, Valencia, Spain) for his help in creating the figures for this article.
EDITOR'S NOTE
This manuscript has undergone an especially rapid internal review by the editorial team due to the strong interest in disseminating the information among the scientific community. The editors thank Permanyer Publications for their collaboration and commitment to the prompt publication of this document.
REFERENCES
1. Jin YH, Cai L, Cheng ZS, et al. A rapid advice guideline for the dianosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (strandard versión). Military Med Res. 2020. https://doi.org/10.1186/s40779-020-0233-6.
2. Zeng YY, Ma YT, Zhang JY, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020. https://doi.org/10.1038/s41569-020-0360-5.
3. Società Italiana di Cardiologia Interventistica. Gestione sale di emodinamica e cardiologia interventistica per emergenza covid-19. Available at: https://gise.it/Uploads/EasyCms/GM%20CF%20per%20PD%20gestione%20covid-19%20-_14892.pdf. Accessed 14 Mar 2020.
4. Procedimiento de actuación par los servicios de prevención de riesgos laborales frente a la exposición al SARS-CoV-2 . Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/PrevencionRRLL_COVID-19.pdf. Accessed 6 May 2020.
5. Generalitat de Catalunya. Procedimiento de actuación frente a casos de infección por el nuevo coronavirus SARS-CoV-2. Available at: http://canalsalut.gencat.cat/ca/salut-a-z/c/coronavirus-2019-ncov/material-professionals/index.html#googtrans(ca|es). Accessed 14 Mar 2020.
6. World Health Organization. Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health. Available at: https://www.who.int/docs/default-source/coronaviruse/who-rights-roles-respon-hw-covid-19.pdf?sfvrsn=bcabd401_0. Accessed 14 Mar 2020.
7. World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19). Interim guidance 27 February 2020. Available at: https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. Accessed 14 Mar 2020.
8. Sociedad Española de Cardiología. No hay evidencia clínica ni científica para suspender tratamientos de IECA y ARA debido a la infección por COVID-19. Available at: https://secardiologia.es/institucional/socios/comunicados/comunicados-oficiales/11446-no-hay-evidencia-clinica-ni-cientifica-para-suspender-tratamientos-de-ieca-y-ara-debido-a-la-infeccion-por-covid-19. Accessed 14 Mar 2020.
Corresponding author: Servicio de Cardiología, Hospital Universitario de Bellvitge, Feixa Llarga s/n, 08907 L’Hospitalet de Llobregat, Barcelona, Spain.
E-mail address: rafaromaguera@gmail.com (R. Romaguera).











