To the Editor,
Constrictive pericarditis (CP) is cause for diastolic heart failure due to the presence of a non-distensible pericardium. Diagnostic suspicion is key here because, even though it is a potentially curable condition, if untreated, its morbimortality rate is high.1 Its differential diagnosis with restrictive cardiomyopathy can be a real challenge.2 We present a case where the invasive hemodynamic assessment performed through cardiac catheterization showed its validity and diagnostic importance in the therapeutic decision-making process.
We present the case of a 59-year old hypertensive woman, former smoker and with a prior medical history of Hodgkin lymphoma at 18 years old —for which she was treated with tele-cobalt therapy and chemotherapy— and carcinoma located in her left breast that was mastectomized when she was 52 years of age. She was re-admitted twice in 2 months due to right heart failure with presence of the Kussmaul sign (video 1 of supplementary data). Due to the poor acoustic window, the transthoracic echocardiography conducted only showed pericardial thickening and preserved biventricular systolic function without significant valvular heart disease. In the presence of severe pericardial calcification (figure 1) and due to the patient’s clinical manifestations and prior medical history of chest radiation, cardiac catheterization was decided to confirm the suspicion of post-radiotherapy CP and indicate surgical pericardiectomy.
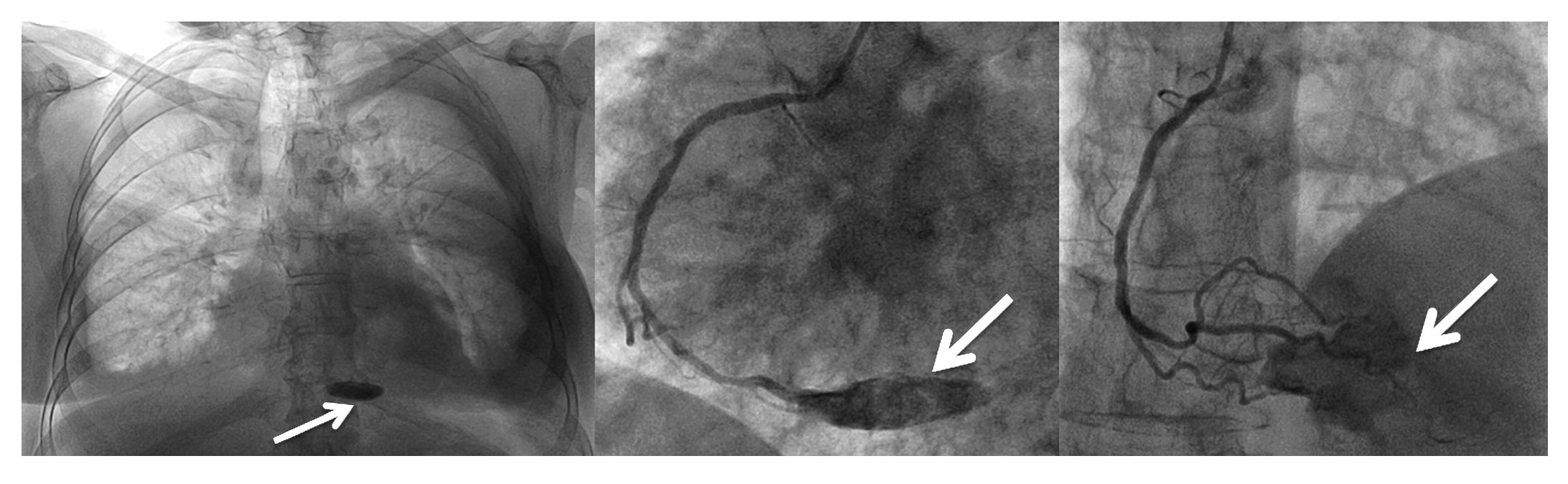
Figure 1. Inferior pericardial calcification (arrows).
The hemodynamic assessment confirmed a reduced cardiac index (1.82 L/min/m2) and a significant increase of pressure in the right cardiac cavities and other classical signs of constrictive pericarditis,1-3 such as very deep x and y descent in the right atrium (figure 2A) and dip-plateau morphology in the right ventricular pressure curve (figure 2B). The simultaneous registry of pressures from both ventricles also showed the equalization of their end-diastolic pressures (figure 2C) and ruled out the expected increase of ventricular interdependence with the existence of parallel changes in both pressures with breathing movements (figure 2D). Also, the patient showed moderate postcapillary pulmonary hypertension (figure 2E,F). No significant coronary lesions were found, al-though the most distal branches of the right coronary artery were somehow fixed at the level of the inferior pericardial calcification (figure 1 and video 2 of supplementary data), a finding considered specific of CP.1
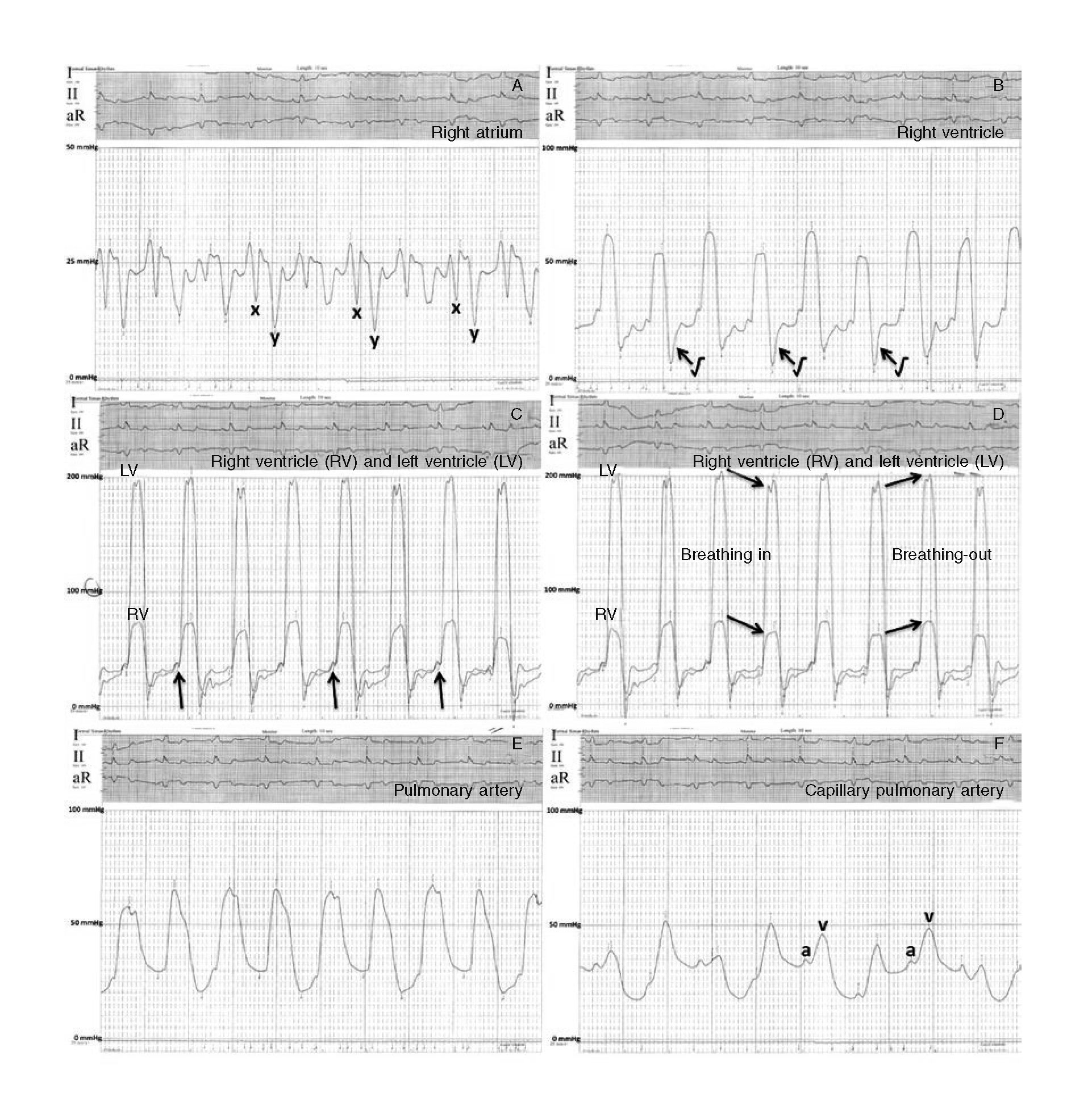
Figure 2. Registry of pressures. A: right atrium (average 22 mmHg) with deep sinuses x and y; B: right ventricle (61/10-27 mmHg) with square root symbol (arrow); C and D: right and left ventricles with equalization of both end-diastolic pressures (arrows), parallel decrease (ventricular match) of pressure curves while breathing in parallel increase while breathing-out; E: pulmonary artery (65/25(42) mmHg); and F: capillary pulmonary artery (31 mmHg) with a prominent v wave.
We should consider the diagnosis of CP in the presence of mainly right heart failure-like symptoms. Clinical findings and non-invasive diagnostic modalities allow to diagnose it in 70% of all cases.1 However, the remaining patients may need cardiac catheterization for a correct differentiation between CP and restrictive cardiomyopathy, especially those with a prior medical history of radiotherapy or heart surgery in whom pericardial and myocardial damages are usually coexistent.2,3
The classical criteria of CP (et, early fast ventricular filling or end-diastolic pressure equalization of the 4 cardiac chambers, lack of pulmonary hypertension, etc.) have low sensitivity and specificity for differential diagnosis purposes when it comes to restrictive cardiomyopathy.1-3 To this day, it is widely accepted that the dynamic breathing variations of intracardiac pressures are very accurate1,2 and have a 97% sensitivity rate and a 100% positive predictive value for the identification of patients with CP.3 In CP there is a dissociation between intrathoracic and intracardiac pressures with reduced intrathoracic pressure not transferred to the cardiac cavities during breathing, which leads to reduced left ventricular filling. In the presence of a non-distensible pericardium with a relatively fixed intrapericardial volume, this reduced left ventricular filling simultaneously increases to the right ventricular filling. The opposite happens when breathing out. This increased ventricular interdependence automatically translates into impaired ventricular systolic pressures. In other clinical scenarios there is an increase and decrease of both pressures consistent with the breathing cycle (ventricular match), but in the case of CP, these variations simply do not match,1,2 which is a highly sensitive and specific marker3 not found in our patient.
Even though the Doppler echocardiogram can assess these changes during the respiration phase using the analysis of transmitral flow pattern and septal movements,1 patients who have undergone heart surgery or received radiotherapy in the past usually show acoustic windows that complicate this assessment. As it has already been confirmed, the detection of thickening or pericardial calcification in the different imaging modalities available today does not necessarily reflect a purely constrictive pathophysiology.3
Our hemodynamic assessment shows a probable mixed condition of myocardial constriction and restriction due to chest radiation sustained by the patient in her youth. With the data presented here, we believe that the case reinforces the need to perform very precise hemodynamical assessments of these patients before indicating any surgical interventions2 especially when the perioperative mortality rate of pericardiectomy of these patients can exceed 20%.1 That is why we initially took a conservative approach and waited on the patient’s clinical progression after a slow and adequate optimization of the medical therapy.
SUPPLEMENTARY DATA
Video 1. Ruiz-Garcia J. DOI: 10.24875/RECICE.M19000027
Video 2. Ruiz-Garcia J. DOI: 10.24875/RECICE.M19000027
REFERENCES
1. Miranda WR, Oh JK. Constrictive Pericarditis:A Practical Clinical Approach. Prog Cardiovasc Dis. 2017;59:369-379.
2. Geske JB, Anavekar NS, Nishimura RA, Oh JK, Gersh BJ. Differentiation of Constriction and Restriction:Complex Cardiovascular Hemodynamics. J Am Coll Cardiol. 2016;68:2329-2347.
3. Talreja DR, Nishimura RA, Oh JK, Holmes DR. Constrictive pericarditis in the modern era:novel criteria for diagnosis in the cardiac catheterization laboratory. J Am Coll Cardiol. 2008;51:315-319.
E-mail address: j.ruizgarcia@hotmail.com (J. Ruiz-García).











