To the Editor,
Spontaneous coronary artery dissection (SCAD) is a low incidence disease that can cause acute coronary syndromes.1,2 Although substantial advances have been made in the knowledge of the physiology, diagnosis, clinical management, and prognosis of SCAD, the degree to which such knowledge has entered the medical community is still uncertain. For this reason, it was decided to conduct a descriptive research on the knowledge and attitude of the Spanish interventional cardiologists towards SCAD.
The authors developed a 24-question survey including the clinical presentation, diagnosis, and acute and postcritical management of SCAD.3 The initiative was approved and supported by the Working Group on Hemodynamics and Interventional Cardiology of the Spanish Society of Cardiology. The survey was closed in December 2018 with 161 answers from 72 centers (26 respondents did not complete the variable “center”).
Figure 1 shows the answers given to the question “diagnosis”. Two thirds of the respondents associated the SCAD with the profile of a young woman without any risk factors or pregnancy/puerperium- related. Regarding the angiographic manifestation, the most common pattern recognized by the respondents was not an angiographic dissection, but the loss of diffuse caliber in the blood vessel (type 2). Also, most respondents reported a low use of intracoronary imaging for the diagnosis of SCAD. More detailed answers to other questions can be found on the supplementary data.
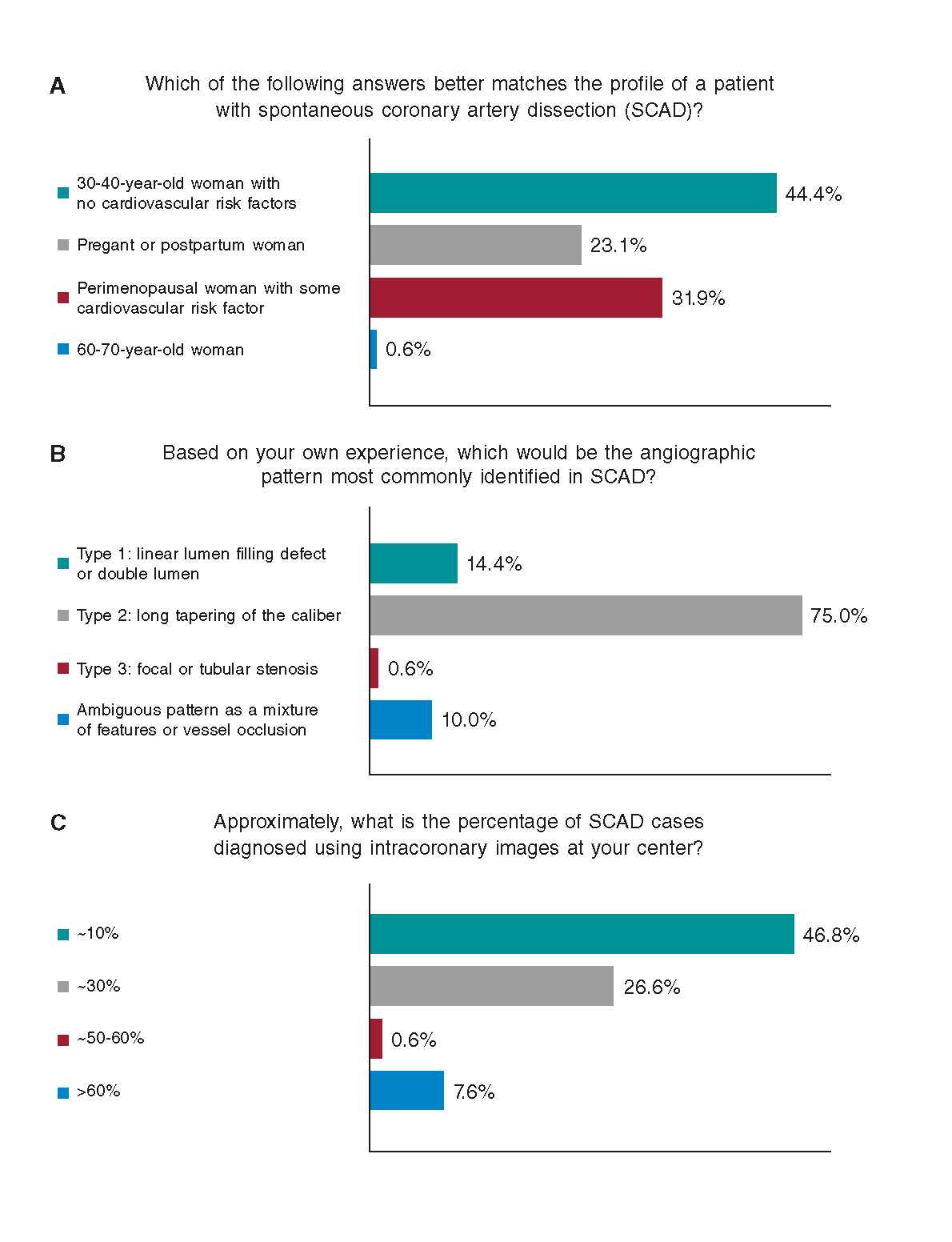
Figura 1. Questions on presentation and diagnosis.
On suspicion that a stenosis can be a SCAD in the mid anterior descending artery with preserved flow in a patient with acute coronary syndrome, 40% of the respondents said they would use intracoronary images to clarify the diagnosis, while 58.7% responded that they would choose a purely conservative approach and complete the procedure; most of these respondents (72.4%) would perform a follow-up coronary angiography.
Another question in the survey revealed the lack of consensus on the time frame recommended to perform the follow-up coro- nary angiography. On the indications for performing a coronary computed tomography angiography, 39.8% of respondents said they use it for follow-up purposes of SCADs with high-risk anatomies without revascularization (proximal/multivessel), while 39.1% said they use it for routine follow-up. A minority of respondents (18.6%) indicated the coronary computed tomography angiography in patients diagnosed with SCAD with recurring pain and no confirmed ischemia.
During the acute management at the cath lab, most respondents (54.7%) claimed that less than 20% of the patients with SCADs are treated using percutaneous angioplasties at their centers. For patients with SCAD who require interventional management, 67.7% of respondents said they choose drug-eluting stents; 14.3%, bioresorbable stents; 3.1%, conventional stents, and 14.9% said they always try to avoid implanting a stent (angioplasty without stent). To the question on the experience with cutting balloons, only 8.1% claimed to have used them in the past, while 45% thought this technique was interesting. Coronary revascularization surgery had been indicated as a bailout surgery for percutaneous angioplasty (19.3%) more or less for the left main coronary artery/multivessel (34.7%). However, 46% of respondents admitted they had never indicated surgery.
Figure 2 shows the answers given to the question of postcritical care in patients with SCAD in the mid left anterior descending artery undergoing conservative therapy. It should be mentioned that most respondents recommended prolonged monitoring (> 3 days).
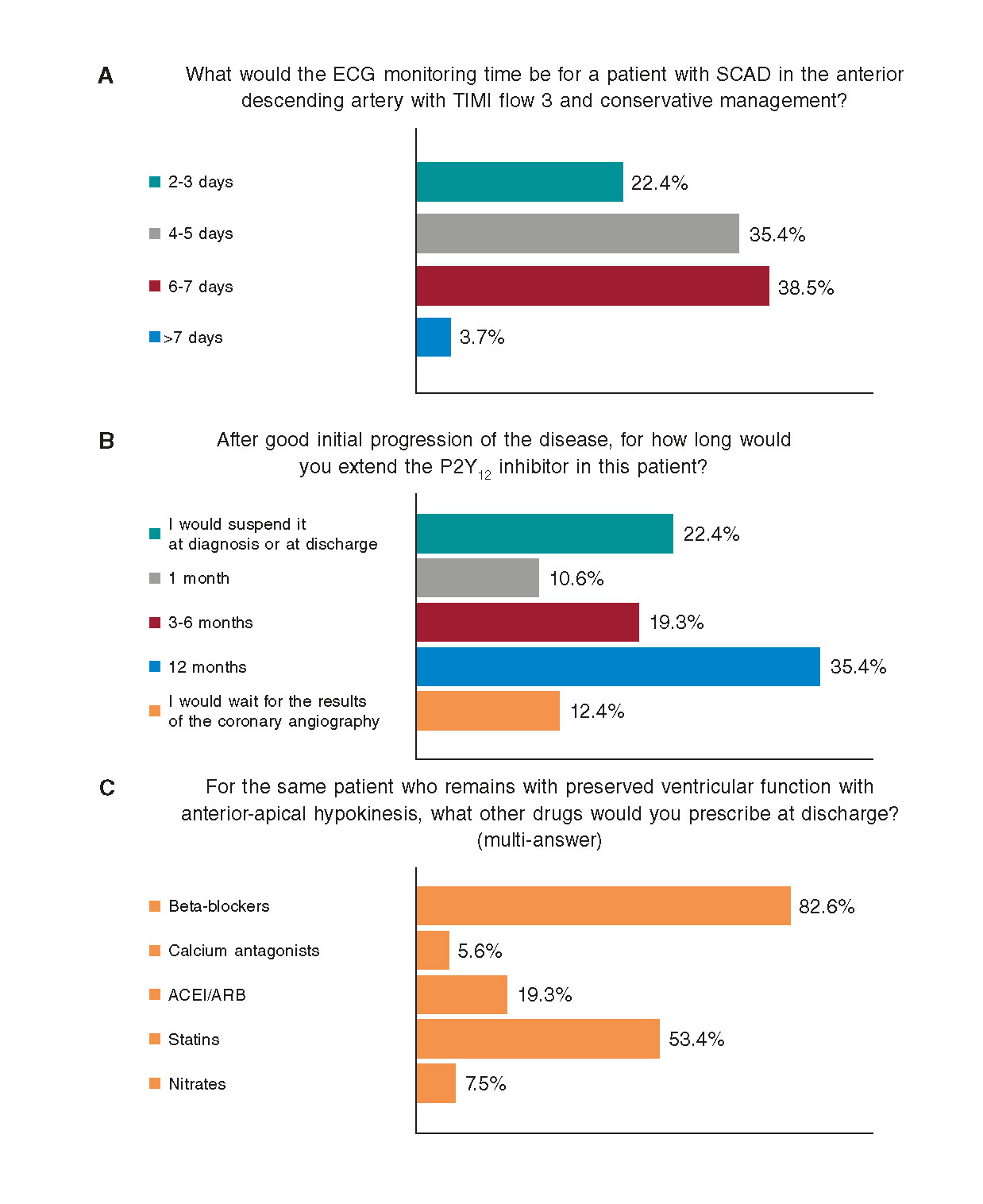
Figura 2. Questions on the postcritical care of patients with spontaneous coronary artery dissections treated conservatively. ACEI/ARB, angiotensin- converting enzyme inhibitor/angiotensin receptor blocker; ECG, electrocardiogram; SCAD, spontaneous coronary artery dissection; TIMI, Thrombolysis in Myocardial Infarction.
In the medical practice, there is a great variety of antiaggregant drugs and other therapies to be prescribed; still, beta-blockers are indicated by most respondents (82.6%) in patients with preserved ventricular function.
The systematic practice of screening extra-coronary arteriopathy is performed by 44.8% of respondents. On this regard, the most widely used imaging modality is the computed tomography scan (76.4%) followed by magnetic resonance imaging (27.6%) and invasive catheterization (18.1%).
The results from this survey show that there is a significant variety in the perception and management of SCAD by the interventional cardiologists of our country.
Contrary to the classical profile of a fertile young woman, contemporary epidemiological data on SCAD reveal the prototypical profile of a 50-year-old woman during perimenopause and with a few risk factors.2
On the other hand, becoming familiar with the angiographic manifestation of this disease has facilitated diagnosis and reduced the use of intracoronary images, a technique with associated risks.4
When it comes to the time frame for performing the control coronary angiography, we have seen that most SCADs improve or resolve within a month; however, waiting a little longer turned out to be safe and can improve the diagnostic performance of this second coronary angiography.2
The percentage of conservative management reported in this survey is below the percentage reported in other series published, which may be a positive piece of information if we consider the preference of conservative treatment for this pathology.1 Choosing prolonged monitoring in these patients makes total sense and is consistent with the fact that recurring events happen during the first week of convalescence.5 Finally, the predominant use of beta-blockers is also logical considering their potential advantages and effects. Also because these are the only drugs with some degree of evidence of prophylaxis against SCAD recurrences.1
Despite the recent advances made on what we know about this disease and the clinical management of SCAD, there are some key issues in the clinical management of these patients that still need to be solved. The present survey showed a moderate degree of acceptance of the evidence and recommendations available today,1,2 but also lack of consensus on other issues. If we want to move forward, a huge collective effort for the study of this disease is required through collaborations and prospective registries.
ACKNOWLEDGEMENTS
The authors wish to thank the interventional cardiologists for their time spent on filling this report, as well as the support received from the Working Group on Hemodynamics and Interventional Cardiology of the Spanish Society of Cardiology while conducting this study. The first author has received a grant from the Fundación Interhospitalaria Investigación Cardiovascular.
REFERENCES
1. Adlam D, Alfonso F, Maas A, Vrints C;Writing Committee. European Society of Cardiology, acute cardiovascular care association, SCAD study group:a position paper on spontaneous coronary artery dissection. Eur Heart J. 2018;39:3353-3368.
2. Macaya F, Salinas P, Gonzalo N, Fernández-Ortiz A, Macaya C, Escaned J. Spontaneous coronary artery dissection:contemporary aspects of diagnosis and patient management. Open Heart. 2018;5:e000884.
3. Percepción y experiencia sobre la disección coronaria espontánea:encuesta a cardiólogos intervencionistas de España. 2018. Available online: https://forms.gle/8aySBLo3WxxbU88w9. Accessed 3 Jun 2019.
4. Macaya F, Salazar CH, Pérez-Vizcayno MJ, et al. Feasibility and Safety of Intracoronary Imaging for Diagnosing Spontaneous Coronary Artery Dissection. JACC Cardiovasc Imaging. 2019;12:763-764.
5. Waterbury TM, Tweet MS, Hayes SN, et al. Early Natural History of Spontaneous Coronary Artery Dissection. Circ Cardiovasc Interv. 2018;11:e006772.
Corresponding author: Instituto Cardiovascular, Hospital Universitario Clínico San Carlos, Profesor Martín Lagos s/n, 28040 Madrid, Spain.
E-mail address: fernando@macaya.eu (F. Macaya).











