CASE RESOLUTION
The heart team decision was to percutaneously treat both the coronary artery disease and the partial anomalous pulmonary venous connection (PAPVC). Percutaneous coronary intervention was successfully performed in the first place. Treatment of the PAPVC was performed 3 months later. Since it is recommended that the diameter of the device should be 30% to 50% larger than the vessel diameter, a 22 mm Amplatzer Vascular Plug II device (AVP-II) (Abbott, United States) was selected based on the VV computed tomography measurements.
The procedure was performed under local anesthesia and with fluoroscopic control. A 7-Fr introducer sheath was inserted into the right femoral vein. A 6-Fr multipurpose diagnostic catheter was advanced using a 0.035 in exchange guidewire to reach the VV through the left innominate vein (figure 1A). Angiography confirmed the presence of a left upper pulmonary vein (LUPV) with dual drainage and significant contrast flow from the LUPV to the innominate vein that filled the right chambers (left-to-right shunt) (figure 1, video 1 of the supplementary data). Using a femoral 7-Fr 90 cm Destination Guiding Sheath (Terumo, United States) the AVP-II device was placed and delivered into the VV (figure 2A, video 2 of the supplementary data). The correct position, absence of residual shunt, patency of innominate vein, and LUPV flow were confirmed by angiography in both the innominate vein (figure 2B,C) and pulmonary artery (figure 2D).
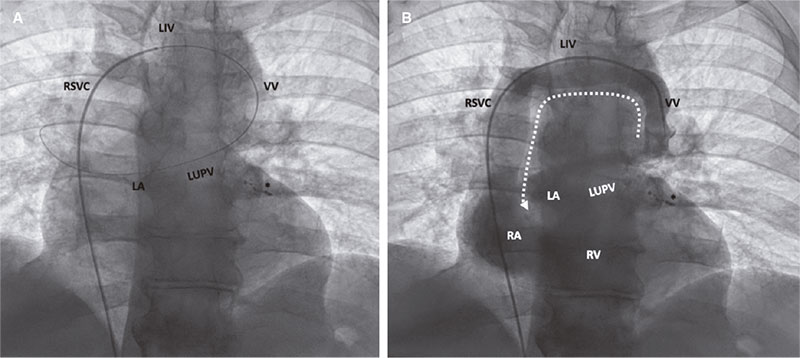
Figure 1. Fluoroscopic image showing the wire pathway from the femoral vein into the left atrium through the right atrium, right superior vena cava (RSVC), left innominate vein (LIV), vertical vein (VV), and left upper pulmonary vein (LUPV) (A); angiogram shows the caudocranial contrast flow from the VV into the LIV, and contrast filling of both the RSVC and the right chambers (B). LA, left atrium; RA, right atrium, RV, right ventricle. Coils used in the previous coronary procedure to treat diagonal branch perforation (*).
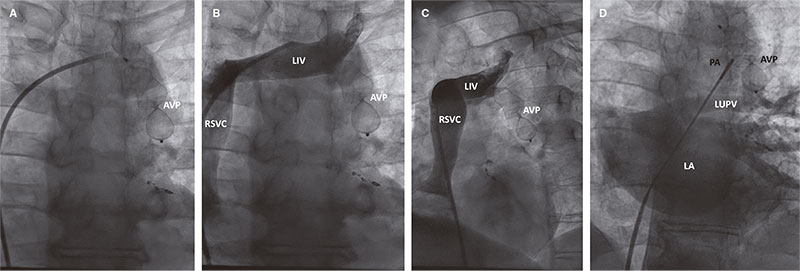
Figure 2. Fluoroscopic image showing the Amplatzer Vascular Plug II device (AVP II) delivery using the Guiding Sheath (A). The angiograms reveal the correct position of the AVP II device, and the patency of the left innominate vein (LIV) flow: posterior-anterior (B) and left anterior oblique (C) views. Contrast injection into the pulmonary artery using a pigtail catheter with left atrium (LA) filling revealing the proper inferior position of the AVP II device, proper flow through the left upper pulmonary vein (LUPV), and lack of caudocranial flow through the occluded vertical vein (D). PA, pulmonary artery, RSVC, right superior vena cava.
Two days later a control computed tomography (figure 3) and a transthoracic echocardiography with microbubble contrast agent were performed. They confirmed the correct position of the AVP-II device, and the lack of pulmonary infarction. At 7-month follow-up the patient remained asymptomatic and cardiac catheterization showed similar successful fluoroscopic findings (videos 3 and 4 of the supplementary data), and significantly improved pulmonary pressures (figure 4).
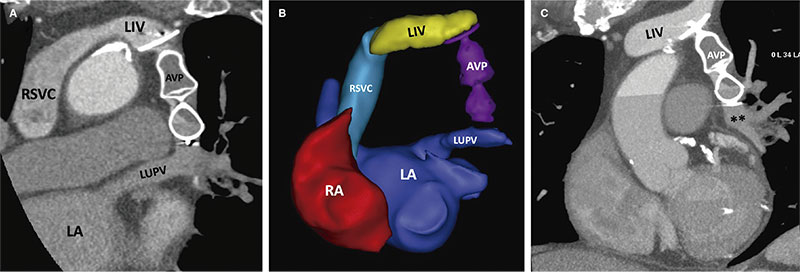
Figure 3. Postoperative thoracic computed tomography. Multiplanar reformatted (A,C), and 3D reconstructed (B) images show the proper position of the Amplatzer Vascular Plug II device (AVP II) occluding the vertical vein that previously connected the left innominate vein (LIV) and the left upper pulmonary vein (LUPV). LA, left atrium; RA, right atrium; RSVC, right superior vena cava.
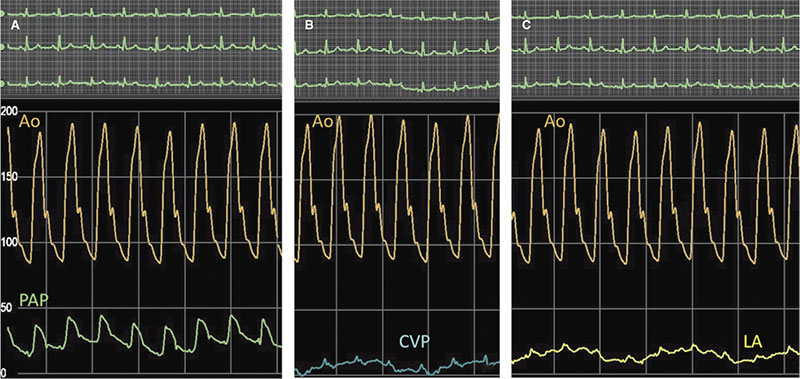
Figure 4. Follow-up hemodynamic measurements showing decreased pulmonary artery pressure (PAP) (A) and left atrial (LA) pressure (C). Central venous pressure (CVP) is similar to the baseline procedure (B). Ao, aorta.
The differential diagnosis of a LUPV with dual drainage should include other left-side vascular structures such as persistent left superior vena cava, which is the most common thoracic venous anomaly and, in most cases, drains into the right atrium. However, it may be connected to the left atrium (LA) through a pulmonary vein. In this scenario the expected direction of blood flow is craniocaudal.
The treatment of PAPVC is indicated with symptoms attributed to significant left-to-right shunt. Shunting is mainly determined by the number and size of anomalous pulmonary veins. In our case, we hypothesize that the dual LUPV connection and the coexistence of an increased LA pressure due to left ventricular dysfunction contributed to a disproportionate shunt for a single anomalous pulmonary vein. This eventually led to right chambers dilatation and symptomatic combined post- and pre-capillary pulmonary hypertension.
Although surgery is the treatment of choice, percutaneous treatment may be a feasible alternative in patients with a pulmonary vein dually draining into a left innominate vein and the LA
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
R. González-Manzanares and G. Flores-Vergara drafted the manuscript and completed its critical revisions. S. Ojeda, J. Suárez de Lezo, S. Espejo, and M. Pan reviewed and revised the manuscript and approved its final version before submission. All authors gave their final approval to the version that would eventually be published.
CONFLICTS OF INTEREST
S. Ojeda is an associate editor of REC: Interventional Cardiology. The journal’s editorial procedure to ensure impartial handling of the manuscript has been followed. The remaining authors declared no conflicts of interest associated with this article.
SUPPLEMENTARY DATA
Vídeo 1. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000302
Vídeo 2. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000302
Vídeo 3. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000302
Vídeo 4. Blanco Borreguero JM. DOI: 10.24875/RECICE.M22000302
REFERENCES
1. Azizova A, Onder O, Arslan S, et al. Persistent left superior vena cava: clinical importance and differential diagnoses. Insights Imaging. 2020;11:110.
2. Mamas MA, Clarke B, Mahadevan VS. Percutaneous treatment of dual pulmonary venous drainage and coarctation of the aorta in a single patient. Exp Clin Cardiol. 2010;15:11-13.
3. Pascual-Tejerina V, Sánchez-Recalde Á, Gutiérrez-Larraya F, Ruiz-Cantador J, Rodríguez-Padial L, Zamorano JL. Transcatheter closure of a vertical vein in a patient with total anomalous pulmonary venous drainage decompressing the left atrium with an AFR device. Rev Esp Cardiol. 2021;74:990-991.
* Corresponding author: Servicio de Cardiología, Hospital Universitario Reina Sofía, Avda. Menéndez Pidal s/n, 14004 Córdoba, Spain.
E-mail address: rafaelglezm@gmail.com (R. González-Manzanares).











