Surgery was discarded due to the patient’s critical condition and low body weight. Emergency cardiac catheterization with stenting was attempted to reduce the risk of early re-coarctation. Ultrasound-guided percutaneous access was used via right carotid artery (4-Fr introducer sheath). The angiography performed confirmed the critical preductal aortic coarctation and the ductus arteriosus (figure 1, video 1 of the supplementary data) with a 3.2 mm underdeveloped transverse arch and a 4.5 mm distal and diaphragmatic aorta. A 4 mm × 16 mm coronary stent was implanted, the distal transverse arch was slightly oversized, and the left subclavian artery was crossed resulting in the uneventful angiographic resolution of the coarctation (figure 2, video 2 of the supplementary data). Gradients were not measured due to the patient’s unstable condition.
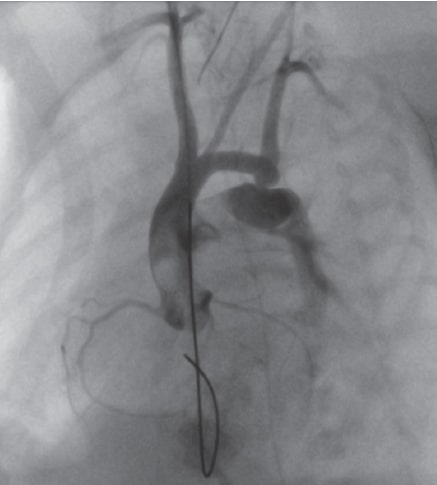
Figure 1. Critical preductal aortic coarctation and large ductus arteriosus.
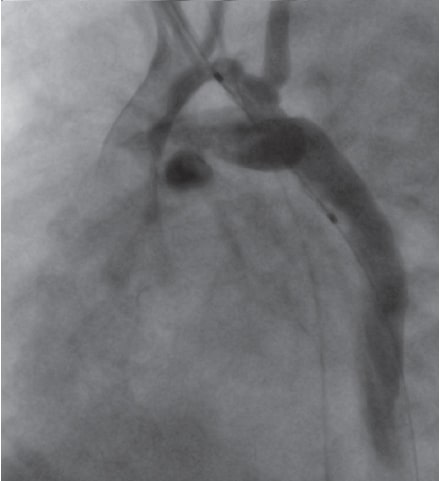
Figure 2. Resolution of coarctation after stent implantation.
Over the following days, postaglandines and vasoactive support were withdrawn, and the patient was extubated. The early echocardiograms performed revealed the presence of residual mild gradients, left ventricular normalization, and the closure of ductus arteriosus. The patient developed occlusive thrombosis of the right common carotid artery and required bemiparin.
Due to the increasing arterial blood pressure levels and the presence of a gradient of between 45 mmHg and 50 mmHg according to the ultrasound data, the patient was re-catheterized when he was 70 days old (2100 grams) via right femoral artery. A gradient of 30 mmHg and endoluminal proliferation were seen (figure 3, video 3 of the supplementary data) as well as a 3.5 mm transverse arch. After dilatation with a 4.5 mm coronary balloon to solve the proliferation the angiography improved (figure 4, video 4 of the supplementary data) and the gradient dropped to 15 mmHg.
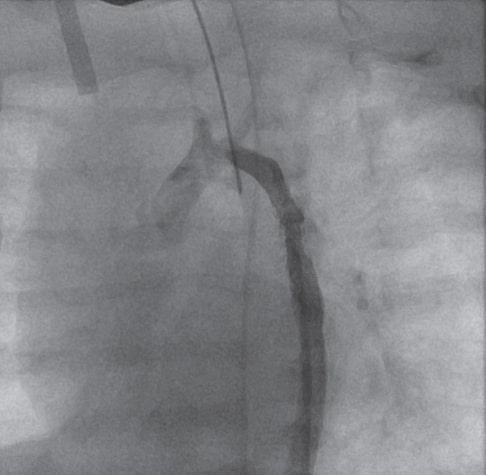
Figure 3. In-stent endoluminal proliferation.
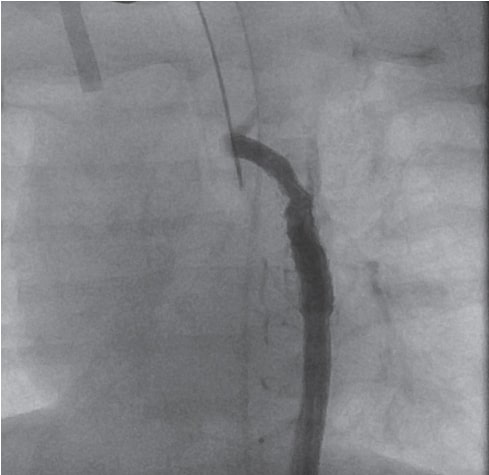
Figure 4. Improvement after angioplasty.
The patient was discharged from the hospital on his 100th day of life with a gradient of 30 mmHg according to ultrasound data, no diastolic prolongation of forward flow, and a normal left ventricular function. The patient remained on antiplatelet therapy with acetylsalicylic acid.
Six months later and with 5.4 kg of body weight the patient showed no signs of re-coarctation (clinical gradient < 20 mmHg, lack of arterial hypertension, and a peak gradient of 26 mmHg on the echocardiogram without diastolic prolongation of forward flow).
The surgical management of aortic coarctation in preterm babies with body weights < 1500 grams is associated with high morbidity, mortality, and re-coarctation rates. The primary angioplasty can be an option here, but with an associated early restenosis rate of up to 50%,1 the risk of vascular damage and aneurysm formation. In a recent series of 5 preterm babies with body weights < 1500 grams treated with primary angioplasty via femoral arterial access, only 1 patient developed restenosis. Surgery was postponed in all the patients until they weighed an average 5.5 kg without any surgical problems derived from the prior stent implantation.2 All of them developed femoral artery thrombosis.
It was decided to attempt this strategy in our patient via carotid access, which allowed his clinical stabilization and postponed surgery for 6 months. However, this triggered a still unsolved carotid artery thrombosis.
Percutaneous treatment as a bridging therapy for the management of preterm babies allows us to postpone surgery and improve results. Although stent angioplasty can reduce the restenosis rate, our patient required reintervention due to endoluminal growth. Whether it should be the technique of choice compared to plain balloon angioplasty is still under discussion. The patient's parents agree with the publication of the clinical case respecting the privacy of the patient’s personal data.
FUNDING
The work has been carried out without funding.
AUTHORS' CONTRIBUTIONS
D. Salas-Mera, and C. Abelleira Pardeiro have drafted and corrected the text of this article. Mr. Ortega Martínez, A. Hernández de Bonis, and F. Gómez Martín have participated in the patient' care and have supervised the text. F. Gutiérrez-Larraya Aguado has supervised the text and contributed to the bibliography.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Salas-Mera D. DOI: 10.24875/RECICE.M20000190
Vídeo 2. Salas-Mera D. DOI: 10.24875/RECICE.M20000190
Vídeo 3. Salas-Mera D. DOI: 10.24875/RECICE.M20000190
Vídeo 4. Salas-Mera D. DOI: 10.24875/RECICE.M20000190
REFERENCES
1. Rothman A, Galindo A, Evans WN, Collazos JC, Restrepo H. Effectiveness and safety of balloon dilation of native aortic coarctation in premature neonates weighing <or =2,500 grams. Am J Cardiol. 2010;105:1176-1180.
2. Stegeman R, Breur JMPJ, Heuser J, et al. Primary coronary stent implantation is a feasible bridging therapy to surgery in very low birth weight infants with critical aortic coarctation. Int J Cardiol. 2018;261:62-65.
Corresponding author: Servicio de Cardiología Pediátrica, Hospital Universitario La Paz, Paseo de la Castellana 261, 28046 Madrid, Spain.
E-mail address: diasalmer@gmail.com (D. Salas-Mera).











